Access to IVF
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Berkshire Echo 52
The Berkshire Echo Issue 52 l The Grand Tour: “gap” travel in the 18th century l Wartime harvest holidays l ‘A strange enchanted land’: fl ying to Paris, 1935 l New to the Archives From the Editor From the Editor It is at this time of year that my sole Holidays remain a status symbol Dates for Your Diary focus turns to my summer holidays. I in terms of destination and invest in a somewhat groundless belief accommodation. The modern Grand Heritage Open Day that time spent in a different location Tour involves long haul instead This year’s Heritage Open Day is Saturday will somehow set me up for the year of carriages, the lodging houses 11 September, and as in previous years, ahead. I am confi dent that this feeling and pensions replaced by fi ve-star the Record Offi ce will be running behind will continue to return every summer, exclusivity. Yet our holidays also remain the scenes tours between 11 a.m. and 1 and I intend to do nothing to prevent it a fascinating insight into how we choose p.m. Please ring 0118 9375132 or e-mail doing so. or chose to spend our precious leisure [email protected] to book a place. time. Whether you lie fl at out on the July and August are culturally embedded beach or make straight for cultural Broadmoor Revealed these days as the time when everyone centres says a lot about you. Senior Archivist Mark Stevens will be who can take a break, does so. But in giving a session on Victorian Broadmoor celebrating holidays inside this Echo, it So it is true for our ancestors. -

Transport for the South East – Consent for Submission of Proposal to Government
CABINET 7 APRIL 2020 TRANSPORT FOR THE SOUTH EAST – CONSENT FOR SUBMISSION OF PROPOSAL TO GOVERNMENT Portfolio Holder: Councillor Phil Filmer, Portfolio Holder for Front Line Services Report from: Richard Hicks, Director of Place and Deputy Chief Executive Author: Michael Edwards, Head of Integrated Transport Summary This report seeks Cabinet support for the creation of a Sub-National Transport Body for the South East, confirmation of Medway’s position as a constituent authority, and consent for the submission of a Proposal to Government for statutory status. 1. Budget and Policy Framework 1.1 Medway Council does not have a stated policy position on Sub-National Transport Bodies. It is possible, however, to align the principles behind its creation with the Council’s priority of maximising regeneration and economic growth. 2. Background 2.1 Transport for the South East (TfSE) formed as a shadow Sub-National Transport Body (STB) in June 2017, and brings together sixteen local transport authorities: Bracknell Forest, Brighton and Hove, East Sussex, Hampshire, Isle of Wight, Medway, Kent, Portsmouth, Reading, Slough, Southampton, Surrey, West Berkshire, West Sussex, Windsor and Maidenhead and Wokingham. The Shadow Partnership Board also includes arrangements for involving five Local Enterprise Partnerships in its governance process, along with two National Park Authorities, forty-four Boroughs and Districts in East Sussex, Hampshire, Kent, Surrey and West Sussex, and representatives from the transport industry. 2.2 TfSE’s aim, as set out in its vision statement, is to grow the South East’s economy by delivering a safe, sustainable, and integrated transport system that makes the South East area more productive and competitive, improves the quality of life for all residents, and protects and enhances its natural and built environment. -

HEAP for Isle of Wight Rural Settlement
Isle of Wight Parks, Gardens & Other Designed Landscapes Historic Environment Action Plan Isle of Wight Gardens Trust: March 2015 2 Foreword The Isle of Wight landscape is recognised as a source of inspiration for the picturesque movement in tourism, art, literature and taste from the late 18th century but the particular significance of designed landscapes (parks and gardens) in this cultural movement is perhaps less widely appreciated. Evidence for ‘picturesque gardens’ still survives on the ground, particularly in the Undercliff. There is also evidence for many other types of designed landscapes including early gardens, landscape parks, 19th century town and suburban gardens and gardens of more recent date. In the 19th century the variety of the Island’s topography and the richness of its scenery, ranging from gentle cultivated landscapes to the picturesque and the sublime with views over both land and sea, resulted in the Isle of Wight being referred to as the ‘Garden of England’ or ‘Garden Isle’. Designed landscapes of all types have played a significant part in shaping the Island’s overall landscape character to the present day even where surviving design elements are fragmentary. Equally, it can be seen that various natural components of the Island’s landscape, in particular downland and coastal scenery, have been key influences on many of the designed landscapes which will be explored in this Historic Environment Action Plan (HEAP). It is therefore fitting that the HEAP is being prepared by the Isle of Wight Gardens Trust as part of the East Wight Landscape Partnership’s Down to the Coast Project, particularly since well over half of all the designed landscapes recorded on the Gardens Trust database fall within or adjacent to the project area. -

Appendix 6 Performance Indicator and CIPFA Data Comparisons BVPI Comparisons
Appendix 6 Performance Indicator and CIPFA Data Comparisons BVPI Comparisons Southend-on-Sea vs CPA Environment High Scorers / Nearest Neighbours / Unitaries BV 106: Percentage of new homes built on previously developed land 2001/02 2002/03 2003/04 Southend-on-Sea 100 100 100 CPA 2002 Environment score 3 or 4 in unitary authorities, by indicator 2001/02 2002/03 2003/04 Blackpool 56.8 63 n/a Bournemouth 94 99 n/a Derby 51 63 n/a East Riding of Yorkshire 24.08 16.64 n/a Halton 27.48 49 n/a Hartlepool 40.8 56 n/a Isle of Wight 84 86 n/a Kingston-upon-Hull 40 36 n/a Luton 99 99.01 n/a Middlesbrough 74.3 61 n/a Nottingham 97 99 n/a Peterborough 79.24 93.66 n/a Plymouth 81.3 94.4 n/a South Gloucestershire 41 44.6 n/a Stockton-on-Tees 33 29.34 n/a Stoke-on-Trent 58.4 61 n/a Telford & Wrekin 54 55.35 n/a Torbay 39 58.57 n/a CIPFA 'Nearest Neighbour' Benchmark Group 2001/02 2002/03 2003/04 Blackpool 56.8 63 n/a Bournemouth 94 99 n/a Brighton & Hove 99.7 100 n/a Isle of Wight 84 86 n/a Portsmouth 98.6 100 n/a Torbay 39 58.57 n/a Unitaries 2001/02 2002/03 2003/04 Unitary 75th percentile 94 93.7 n/a Unitary Median 70 65 n/a Unitary 25th percentile 41 52.3 n/a Average 66.3 68.7 n/a Source: ODPM website BV 107: Planning cost per head of population. -

Should There Be Bridge to the Isle of Wight?
Should there be bridge to the Isle of Wight? Wightlink run two car ferry services to the Isle of Wight, one running from Portsmouth to Fishbourne and takes around 45 minutes and The other from Lymington to Yarmouth which is around a 40 minutes journey both ferries take cars, motor homes, bikes and foot passengers. • Many Isle of Wight residents joke that the island has the most expensive ferry crossing in the world. A return trip with car and two adults can come in at over £100 during high season. • "Every other island community in the British Isles which had the feasibility of a bridge has seen one built. Why is there no bridge to the Isle of Wight?" The Isle of Wight Party wants a bridge to the main land. However road bridges are very expensive to build. For example the road bridge to the Isle of Skye which opened in 1995 cost a total of £39 million to build. Some people are cross about the constant cancellations from Wightlink, Red Funnel & Hovertravel and also having to pay expensive prices to travel to and from the island. Some say it is about time the Isle of Wight was connected via a bridge to the mainland of the United Kingdom. The arguments for a fixed link include claims that it would boost the economy by creating more jobs. It would allow more people to go to the island and spend their money there. A bridge would be a faster and cheaper way to get to the island A bridge would be less dependent on weather The arguments against a bridge are Increases in traffic would put stress on the local road network, It is quite simple really - the I.O.W. -

Minutes Template
ADULT SOCIAL CARE, HEALTH AND HOUSING OVERVIEW AND SCRUTINY PANEL 4 FEBRUARY 2019 7.30 - 9.25 PM Present: Councillors Harrison (Chairman), Allen, Mrs Angell, Mrs Mattick, Ms Merry, Peacey, Mrs Temperton, Thompson and Tullett Observer: Executive Members: Councillor D Birch Also Present: Catriona Khetyar, Head of Medicines Optimisation, East Berkshire CCG Melanie O'Rourke, Assistant Director: Adult Social Care Operations, Bracknell Forest Council Mairead Panetta, Head of Service: Safeguarding, Bracknell Forest Council Ellie Eghtedar, Interim Head of Housing, Bracknell Forest Council Tony Dwyer, Interim Assistant Director: Mental Health and Out of Hours, Bracknell Forest Council Jacqui Wilton, Family Safeguarding Model (FSM) Project Officer, Bracknell Forest Borough Council Ollie Lamping, Domestic Abuse Perpetrator Service Worker (DAPS), Bracknell Forest Borough Council Apologies for absence were received from: Councillors Mrs McCracken and Dr Hill Dr David Norman, Co-opted Representative Mark Sanders, Healthwatch Bracknell Forest 45. Minutes and Matters Arising RESOLVED: that the Minutes of the Adult Social Care, Health and Housing Overview and Scrutiny Panel held on 15 January 2019 be approved as a correct record, and signed by the Chairman, subject to Janette Fullwood, Head of Children, Young People’s and Families: East Berkshire Clinical Commissioning Group CCG being recorded as Also Present at this meeting. Arising from the Actions Log, Kirstine Berry, Governance and Scrutiny Co-ordinator advised Members that several items were awaiting a status update due to the short time lapse between this and the previous Panel meeting, but that any outstanding actions would be followed up and reported against at the next Panel meeting. There were no Issues Arising since the last meeting on 15 January 2019. -

Bounded by Heritage and the Tamar: Cornwall As 'Almost an Island'
Island Studies Journal, 15(1), 2020, 223-236 Bounded by heritage and the Tamar: Cornwall as ‘almost an island’ Philip Hayward University of Technology Sydney, Australia [email protected] (corresponding author) Christian Fleury University of Caen Normandy, France [email protected] Abstract: This article considers the manner in which the English county of Cornwall has been imagined and represented as an island in various contemporary contexts, drawing on the particular geographical insularity of the peninsular county and distinct aspects of its cultural heritage. It outlines the manner in which this rhetorical islandness has been deployed for tourism promotion and political purposes, discusses the value of such imagination for agencies promoting Cornwall as a distinct entity and deploys these discussions to a consideration of ‘almost- islandness’ within the framework of an expanded Island Studies field. Keywords: almost islands, Cornwall, Devon, islands, Lizard Peninsula, Tamar https://doi.org/10.24043/isj.98 • Received May 2019, accepted July 2019 © 2020—Institute of Island Studies, University of Prince Edward Island, Canada. Introduction Over the last decade Island Studies has both consolidated and diversified. Island Studies Journal, in particular, has increasingly focussed on islands as complex socio-cultural-economic entities within a global landscape increasingly affected by factors such as tourism, migration, demographic change and the all-encompassing impact of the Anthropocene. Islands, in this context, are increasingly perceived and analysed as nexuses (rather than as isolates). Other work in the field has broadened the focus from archetypal islands—i.e., parcels of land entirely surrounded by water—to a broad range of locales and phenomena that have island-like attributes. -

Isle of Wight Settlement Coalescence Study Report.Docm Last Saved: 26/04/2018 17:02
Isle of Wight Settlement Coalescence Study Prepared by LUC April 2018 Project Title: Isle of Wight Settlement Coalescence Study Client: Isle of Wight Council Version Date Version Details Prepared by Checked by Approved by 4.0 26/4/2018 Final Jon Pearson Jon Pearson Philip Smith Richard Swann Ben Gurney Calum McCulloch Victoria Goosen Isle of Wight Settlement Coalescence Study Report.docm Last saved: 26/04/2018 17:02 Isle of Wight Settlement Coalescence Study Prepared by LUC April 2018 Planning & EIA LUC LONDON Offices also in: Land Use Consultants Ltd Registered in England Design 43 Chalton Street Bristol Registered number: 2549296 Landscape Planning London Edinburgh Registered Office: Landscape Management NW1 1JD Glasgow 43 Chalton Street Ecology T +44 (0)20 7383 5784 Lancaster London NW1 1JD FS 566056 EMS 566057 LUC uses 100% recycled paper GIS & Visualisation [email protected] Manchester Contents 1 Introduction 1 Context and key issues 1 Purpose of study 1 2 Methodology 3 Overview 3 Tasks undertaken 3 3 Results - nature of gaps and guidelines for maintenance 5 West Wight area 6 Cowes–Newport area 13 Ryde area 26 ‘The Bay’ area 39 4 Policy review and recommendations 46 Policy review 46 Recommended policy approach to avoiding settlement coalescence 53 1 Introduction Context and key issues 1.1 The Isle of Wight has a unique identity characterised by a predominantly rural landscape. Almost half of its coastline is designated as Heritage Coast and over half of the Island is a designated Area of Outstanding Natural Beauty. The majority of residents live in the Island’s larger settlements, in particular the main towns of Newport, Cowes, East Cowes, Ryde, Sandown and Shanklin. -
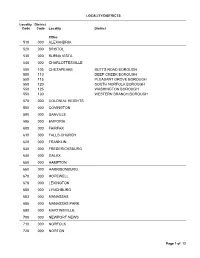
List of PST Locality District Codes (PDF)
LOCALITY/DISTRICTS Locality District Code Code Locality District Cities 510 000 ALEXANDRIA 520 000 BRISTOL 530 000 BUENA VISTA 540 000 CHARLOTTESVILLE 550 105 CHESAPEAKE BUTTS ROAD BOROUGH 550 110 DEEP CREEK BOROUGH 550 115 PLEASANT GROVE BOROUGH 550 120 SOUTH NORFOLK BOROUGH 550 125 WASHINGTON BOROUGH 550 130 WESTERN BRANCH BOROUGH 570 000 COLONIAL HEIGHTS 580 000 COVINGTON 590 000 DANVILLE 595 000 EMPORIA 600 000 FAIRFAX 610 000 FALLS CHURCH 620 000 FRANKLIN 630 000 FREDERICKSBURG 640 000 GALAX 650 000 HAMPTON 660 000 HARRISONBURG 670 000 HOPEWELL 678 000 LEXINGTON 680 000 LYNCHBURG 683 000 MANASSAS 685 000 MANASSAS PARK 690 000 MARTINSVILLE 700 000 NEWPORT NEWS 710 000 NORFOLK 720 000 NORTON Page 1 of 12 LOCALITY/DISTRICTS Locality District Code Code Locality District Cities 730 000 PETERSBURG 735 000 POQUOSON 740 000 PORTSMOUTH 750 000 RADFORD 760 000 RICHMOND 770 000 ROANOKE 775 000 SALEM 790 000 STAUNTON 800 105 SUFFOLK CHUCKATUCK BOROUGH 800 110 CYPRESS BOROUGH 800 115 HOLY NECK BOROUGH 800 120 SLEEPY HOLE BOROUGH 800 125 SUFFOLK BOROUGH 800 130 WHALEYVILLE BOROUGH 810 105 VIRGINIA BEACH (EXCL. SANDBRIDGE SPECIAL SERV. DIST.) 810 110 SANDBRIDGE SPECIAL SERVICE DISTRICT 820 000 WAYNESBORO 830 000 WILLIAMSBURG 840 000 WINCHESTER Page 2 of 12 LOCALITY/DISTRICTS Locality District Code Code Locality District Counties 001 005 ACCOMACK ATLANTIC DISTRICT 001 010 ISLAND DISTRICT 001 015 LEE DISTRICT 001 020 METOMPKIN DISTRICT 001 025 PUNGOTEAGUE DISTRICT 001 702 ACCOMAC, TOWN OF 001 709 BELLE HAVEN, TOWN OF 001 715 BLOXOM, TOWN OF 001 741 -

Shoreline Flora of the Blackwater River in Southampton and Isle of Wight Counties, Virginia
44 Banisteria, Number 8, .1996 © 1996 by the Virginia Natural History Society Shoreline Flora of the Blackwater River in Southampton and Isle of Wight Counties, Virginia. J. Christopher Ludwig Virginia Department of Conservation and Recreation, Division of Natural Heritage 1500 E. Main Street, Suite 312, Richmond, VA 23219 During his extensive botanical research in (Vahl.) Pax., Justicia ovata, Micranthemum umbrosum, southeastern Virginia, Merritt Lyndon Fernald (1937, Mitreola petiolata, and Oldenlandia boscii (DC.) Chapman. 1938, 1941, 1942, 1943) collected many plant specimens Furthermore, the discovery of Eupatorium comPositifolium from exposed shorelines of the region's rivers, creeks, and Walt. is noteworthy. A discussion of these species follows. large millponds. His collections along the Blackwater Voucher specimens with collection numbers and River included Justicia ovata (Walt.) Lindau, Micranthemum repositories are noted. umbrosum (J.F. Gmel.) Blake, and Mitreola petiolata (J.F. The most abundant of the rare species was Justicia Gmel.) Torr. & Gray, plant species now considered rare ovata which thrived on open shores of the river and was in Virginia (Ludwig, 1996). On 14 and 28 September also abundant in the densely shaded bottomland forests. 1993 and 12 September 1995, I collected and recorded I collected a specimen on 12 September 1995 vascular plant species along the Blackwater River shores to approxirriately 1.1 km south of the State Route 603 bridge determine the status of the rare species. My work was in Isle of Wight County (2596,VPI). All collections of this conducted from Zuni to Franklin in Isle of Wight and species within Virginia are limited to bottomlands of the Southampton Counties, a distance of ca. -

Roman Isle of Wight
ROMAN WIGHT By Malcolm Lyne September 2006 1. A history of previous research Most of the early antiquarian research into Roman Wight, as in other parts of Britain, related to the excavation of villa houses. The earliest such excavation was that at Rock,Brighstone in 1831 (Kell 1856), followed by those at Carisbrooke (Spickernell 1859), Gurnard (Kell 1866) and Brading during the 1880s (Price and Price 1881 and 1900). Other villa sites were noted at Combley and Clatterford during the same period (Kell 1856). The published accounts of most of these excavations are somewhat deficient but, in the case of Gurnard, are supplemented by unpublished manuscript notes of further excavations carried out after publication of the earlier work in 1866. Just a few of the artefacts found at Carisbrooke and Gurnard still survive. The one exception to this sorry tale is Brading: the published accounts of the excavations carried out by Captain Thorp and the Price brothers is more informative than most for this period and most of the pottery and other finds are still extant. Other 19 th c. observations on the Island’s Roman archaeology are largely restricted to brief accounts of coin hoards from Farringford, Wroxall and Cliff Copse, Shanklin written up by Kell (1863). A further hoard found at Wootton in 1833 had to wait for more than 100 years before a reasonably-detailed account was produced (Sydenham 1943). The early years of the 20 th century saw little improvement in the quality of atchaeological activity relating to Roman Wight. Poorly-recorded excavations at Combley villa in 1910 (Sydenham 1945, 426-29) were, however, soon followed by the activities of Ambrose Sherwin as curator of Carisbrooke Castle museum during the 1920s and 30s. -

The Isle of Wight in the English Landscape
THE ISLE OF WIGHT IN THE ENGLISH LANDSCAPE: MEDIEVAL AND POST-MEDIEVAL RURAL SETTLEMENT AND LAND USE ON THE ISLE OF WIGHT HELEN VICTORIA BASFORD A study in two volumes Volume 1: Text and References Thesis submitted in partial fulfilment of the requirements of Bournemouth University for the degree of Doctor of Philosophy January 2013 2 Copyright Statement This copy of the thesis has been supplied on condition that anyone who consults it is understood to recognise that its copyright rests with its author and due acknowledgement must always be made of the use of any material contained in, or derived from, this thesis. 3 4 Helen Victoria Basford The Isle of Wight in the English Landscape: Medieval and Post-Medieval Rural Settlement and Land Use Abstract The thesis is a local-scale study which aims to place the Isle of Wight in the English landscape. It examines the much discussed but problematic concept of ‘islandness’, identifying distinctive insular characteristics and determining their significance but also investigating internal landscape diversity. This is the first detailed academic study of Isle of Wight land use and settlement from the early medieval period to the nineteenth century and is fully referenced to national frameworks. The thesis utilises documentary, cartographic and archaeological evidence. It employs the techniques of historic landscape characterisation (HLC), using synoptic maps created by the author and others as tools of graphic analysis. An analysis of the Isle of Wight’s physical character and cultural roots is followed by an investigation of problems and questions associated with models of settlement and land use at various scales.