NIH Public Access Author Manuscript Cancer J
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Profiling Data
Compound Name DiscoveRx Gene Symbol Entrez Gene Percent Compound Symbol Control Concentration (nM) JNK-IN-8 AAK1 AAK1 69 1000 JNK-IN-8 ABL1(E255K)-phosphorylated ABL1 100 1000 JNK-IN-8 ABL1(F317I)-nonphosphorylated ABL1 87 1000 JNK-IN-8 ABL1(F317I)-phosphorylated ABL1 100 1000 JNK-IN-8 ABL1(F317L)-nonphosphorylated ABL1 65 1000 JNK-IN-8 ABL1(F317L)-phosphorylated ABL1 61 1000 JNK-IN-8 ABL1(H396P)-nonphosphorylated ABL1 42 1000 JNK-IN-8 ABL1(H396P)-phosphorylated ABL1 60 1000 JNK-IN-8 ABL1(M351T)-phosphorylated ABL1 81 1000 JNK-IN-8 ABL1(Q252H)-nonphosphorylated ABL1 100 1000 JNK-IN-8 ABL1(Q252H)-phosphorylated ABL1 56 1000 JNK-IN-8 ABL1(T315I)-nonphosphorylated ABL1 100 1000 JNK-IN-8 ABL1(T315I)-phosphorylated ABL1 92 1000 JNK-IN-8 ABL1(Y253F)-phosphorylated ABL1 71 1000 JNK-IN-8 ABL1-nonphosphorylated ABL1 97 1000 JNK-IN-8 ABL1-phosphorylated ABL1 100 1000 JNK-IN-8 ABL2 ABL2 97 1000 JNK-IN-8 ACVR1 ACVR1 100 1000 JNK-IN-8 ACVR1B ACVR1B 88 1000 JNK-IN-8 ACVR2A ACVR2A 100 1000 JNK-IN-8 ACVR2B ACVR2B 100 1000 JNK-IN-8 ACVRL1 ACVRL1 96 1000 JNK-IN-8 ADCK3 CABC1 100 1000 JNK-IN-8 ADCK4 ADCK4 93 1000 JNK-IN-8 AKT1 AKT1 100 1000 JNK-IN-8 AKT2 AKT2 100 1000 JNK-IN-8 AKT3 AKT3 100 1000 JNK-IN-8 ALK ALK 85 1000 JNK-IN-8 AMPK-alpha1 PRKAA1 100 1000 JNK-IN-8 AMPK-alpha2 PRKAA2 84 1000 JNK-IN-8 ANKK1 ANKK1 75 1000 JNK-IN-8 ARK5 NUAK1 100 1000 JNK-IN-8 ASK1 MAP3K5 100 1000 JNK-IN-8 ASK2 MAP3K6 93 1000 JNK-IN-8 AURKA AURKA 100 1000 JNK-IN-8 AURKA AURKA 84 1000 JNK-IN-8 AURKB AURKB 83 1000 JNK-IN-8 AURKB AURKB 96 1000 JNK-IN-8 AURKC AURKC 95 1000 JNK-IN-8 -

Protein Kinase D3 Sensitizes RAF Inhibitor RAF265 in Melanoma Cells by Preventing Reactivation of MAPK Signaling
Published OnlineFirst April 28, 2011; DOI: 10.1158/0008-5472.CAN-10-3761 Cancer Tumor and Stem Cell Biology Research Protein Kinase D3 Sensitizes RAF Inhibitor RAF265 in Melanoma Cells by Preventing Reactivation of MAPK Signaling Jian Chen, Qiong Shen, Mark Labow, and L. Alex Gaither Abstract RAS mutations occur in more than 30% of all human cancers but efforts to directly target mutant RAS signaling as a cancer therapy have yet to succeed. As alternative strategies, RAF and MEK inhibitors have been developed to block oncogenic signaling downstream of RAS. As might be expected, studies of these inhibitors have indicated that tumors with RAS or BRAF mutations display resistance RAF or MEK inhibitors. In order to better understand the mechanistic basis for this resistance, we conducted a RNAi-based screen to identify genes that mediated chemoresistance to the RAF kinase inhibitor RAF265 in a BRAF (V600E) mutant melanoma cell line that is resistant to this drug. In this way, we found that knockdown of protein kinase D3 (PRKD3) could enhance cell killing of RAF and MEK inhibitors across multiple melanoma cell lines of various genotypes and sensitivities to RAF265. PRKD3 blockade cooperated with RAF265 to prevent reactivation of the MAPK signaling pathway, interrupt cell cycle progression, trigger apoptosis, and inhibit colony formation growth. Our findings offer initial proof-of-concept that PRKD3 is a valid target to overcome drug resistance being encountered widely in the clinic with RAF or MEK inhibitors. Cancer Res; 71(12); 4280–91. Ó2011 AACR. Introduction are found mutationally activated in 30% of all human cancers, with highest prevalence in pancreas (90%), colon (50%), RAS–RAF mitogen-activated protein kinase (MAPK) signal- thyroid (50%), and lung (30%) cancers (1, 2). -

Supplementary Table 1. in Vitro Side Effect Profiling Study for LDN/OSU-0212320. Neurotransmitter Related Steroids
Supplementary Table 1. In vitro side effect profiling study for LDN/OSU-0212320. Percent Inhibition Receptor 10 µM Neurotransmitter Related Adenosine, Non-selective 7.29% Adrenergic, Alpha 1, Non-selective 24.98% Adrenergic, Alpha 2, Non-selective 27.18% Adrenergic, Beta, Non-selective -20.94% Dopamine Transporter 8.69% Dopamine, D1 (h) 8.48% Dopamine, D2s (h) 4.06% GABA A, Agonist Site -16.15% GABA A, BDZ, alpha 1 site 12.73% GABA-B 13.60% Glutamate, AMPA Site (Ionotropic) 12.06% Glutamate, Kainate Site (Ionotropic) -1.03% Glutamate, NMDA Agonist Site (Ionotropic) 0.12% Glutamate, NMDA, Glycine (Stry-insens Site) 9.84% (Ionotropic) Glycine, Strychnine-sensitive 0.99% Histamine, H1 -5.54% Histamine, H2 16.54% Histamine, H3 4.80% Melatonin, Non-selective -5.54% Muscarinic, M1 (hr) -1.88% Muscarinic, M2 (h) 0.82% Muscarinic, Non-selective, Central 29.04% Muscarinic, Non-selective, Peripheral 0.29% Nicotinic, Neuronal (-BnTx insensitive) 7.85% Norepinephrine Transporter 2.87% Opioid, Non-selective -0.09% Opioid, Orphanin, ORL1 (h) 11.55% Serotonin Transporter -3.02% Serotonin, Non-selective 26.33% Sigma, Non-Selective 10.19% Steroids Estrogen 11.16% 1 Percent Inhibition Receptor 10 µM Testosterone (cytosolic) (h) 12.50% Ion Channels Calcium Channel, Type L (Dihydropyridine Site) 43.18% Calcium Channel, Type N 4.15% Potassium Channel, ATP-Sensitive -4.05% Potassium Channel, Ca2+ Act., VI 17.80% Potassium Channel, I(Kr) (hERG) (h) -6.44% Sodium, Site 2 -0.39% Second Messengers Nitric Oxide, NOS (Neuronal-Binding) -17.09% Prostaglandins Leukotriene, -
Endometrial Gene Expression in the Early Luteal Phase Is Impacted By
Human Reproduction, Vol.27, No.11 pp. 3259–3272, 2012 Advanced Access publication on August 28, 2012 doi:10.1093/humrep/des279 ORIGINAL ARTICLE Reproductive biology Endometrial gene expression in the early luteal phase is impacted by mode of triggering final oocyte maturation in recFSH stimulated and GnRH antagonist co-treated IVF cycles P. Humaidan1,*, I. Van Vaerenbergh2, C. Bourgain2, B. Alsbjerg3, Downloaded from C. Blockeel4, F. Schuit5, L. Van Lommel5, P. Devroey4, and H. Fatemi4 1The Fertility Clinic, Department D, Odense University Hospital, OHU, Entrance 55, Odense C 5000, Denmark 2Reproductive Immunology and Implantation Unit, Dutch-speaking Free University of Brussels, Brussels, Belgium 3The Fertility Clinic, Skive Regional Hospital, Skive, Denmark 4Centre for Reproductive Medicine, Dutch-speaking Free University of Brussels, Brussels, Belgium 5Gene Expression Unit, KU Leuven, Leuven, Belgium http://humrep.oxfordjournals.org/ *Correspondence address. Tel: +45-20-34-26-87; E-mail: [email protected] Submitted on March 9, 2012; resubmitted on June 3, 2012; accepted on June 22, 2012 study question: Do differences in endometrial gene expression exist after ovarian stimulation with four different regimens of triggering final oocyte maturation and luteal phase support in the same patient? summary answer: Significant differences in the expression of genes involved in receptivity and early implantation were seen between by greta verheyen on June 5, 2013 the four protocols. what is known already: GnRH agonist triggering -

TGF-Beta/Smad
Inhibitors, Agonists, Screening Libraries www.MedChemExpress.com TGF-beta/Smad The TGF-β superfamily comprises TGF-βs, bone morphogenetic proteins (BMPs), activins and related proteins. These proteins were identified mainly through their roles in development; they regulate the establishment of the body plan and tissue differentiation through their effects on cell proliferation, differentiation and migration. There are eight vertebrate Smads: Smad1 to Smad8. Smad2 and Smad3 are activated through carboxy-terminal phosphorylation by the TGF-b and activin receptors TbRI and ActRIB, whereas Smad1, Smad5 and Smad8 are activated by ALK-1, ALK-2, BMP-RIA/ALK-3 and BMP-RIB/ALK-6 in response to BMP1–4 or other ligands. TGF-β binds two receptor types, the TGF-β type I and type II receptors (TβRI and TβRII, respectively) to form the active signaling complex. The TβRII activates TβRI kinase activity by phosphorylating the TβRI, which then transmits the signal intracellularly by phosphorylating the Smad transcription factors. The Smads constitutively shuttle between the cytoplasm and nucleus, but signaling causes the Smads to accumulate predominantly in the nucleus where they bind DNA and other transcriptional machinery to regulate the expression of target genes. TGF-β also involves in the regulations of PI3K and MAPK signaling pathways. Abnormalities of the TGF-beta receptors and SMADs have been detected in various tumors, including colorectal cancers and pancreatic cancers. In addition, TGF-β/BMP signaling is also involved in osteoblast differentiation, chondrocyte differentiation, skeletal development, cartilage formation, bone formation, bone homeostasis, and related human bone diseases caused by the disruption ofTGF-β/BMP signaling. -
The Oncogenic Role of Protein Kinase D3 in Cancer Yan Liu1,2#, Hang Song4#, Yehui Zhou3#, Xinxing Ma3, Jing Xu4, Zhenghong Yu5 and Liming Chen2
Journal of Cancer 2021, Vol. 12 735 Ivyspring International Publisher Journal of Cancer 2021; 12(3): 735-739. doi: 10.7150/jca.50899 Review The oncogenic role of protein kinase D3 in cancer Yan Liu1,2#, Hang Song4#, Yehui Zhou3#, Xinxing Ma3, Jing Xu4, Zhenghong Yu5 and Liming Chen2 1. The Key Laboratory of Bio-Medical Diagnostics, Suzhou Institute of Biomedical Engineering and Technology, Chinese Academy of Sciences, Suzhou 215163, P. R. China. 2. Jiangsu Key Laboratory for Molecular and Medical Biotechnology, Institute of cancer, Department of biochemistry, College of Life Science, Nanjing Normal University, Nanjing 210023, P. R. China. 3. The First Affiliated Hospital of Soochow University, Soochow University, Suzhou 215006, P. R. China. 4. School of Integrated Chinese and Western Medicine, Anhui University of Chinese Medicine, Hefei 230012, P. R.China. 5. Department of Rheumatology and Immunology, Jinling Hospital, Medical School of Nanjing University, Nanjing 210002, P. R.China. #These authors contributed equally to this work. Corresponding authors: Liming Chen, E-mail:[email protected]; Zhenghong Yu, E-mail:[email protected]. © The author(s). This is an open access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/). See http://ivyspring.com/terms for full terms and conditions. Received: 2020.07.20; Accepted: 2020.10.30; Published: 2021.01.01 Abstract Protein kinase D3 (PRKD3), a serine/threonine kinase, belongs to protein kinase D family, which contains three members: PRKD1, PRKD2, and PRKD3. PRKD3 is activated by many stimuli including phorbol esters, and G-protein-coupled receptor agonists. -
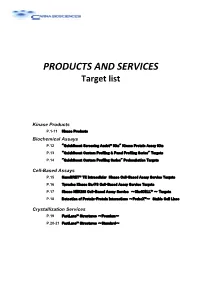
PRODUCTS and SERVICES Target List
PRODUCTS AND SERVICES Target list Kinase Products P.1-11 Kinase Products Biochemical Assays P.12 "QuickScout Screening Assist™ Kits" Kinase Protein Assay Kits P.13 "QuickScout Custom Profiling & Panel Profiling Series" Targets P.14 "QuickScout Custom Profiling Series" Preincubation Targets Cell-Based Assays P.15 NanoBRET™ TE Intracellular Kinase Cell-Based Assay Service Targets P.16 Tyrosine Kinase Ba/F3 Cell-Based Assay Service Targets P.17 Kinase HEK293 Cell-Based Assay Service ~ClariCELL™ ~ Targets P.18 Detection of Protein-Protein Interactions ~ProbeX™~ Stable Cell Lines Crystallization Services P.19 FastLane™ Structures ~Premium~ P.20-21 FastLane™ Structures ~Standard~ Kinase Products For details of products, please see "PRODUCTS AND SERVICES" on page 1~3. Tyrosine Kinases Note: Please contact us for availability or further information. Information may be changed without notice. Expression Protein Kinase Tag Carna Product Name Catalog No. Construct Sequence Accession Number Tag Location System HIS ABL(ABL1) 08-001 Full-length 2-1130 NP_005148.2 N-terminal His Insect (sf21) ABL(ABL1) BTN BTN-ABL(ABL1) 08-401-20N Full-length 2-1130 NP_005148.2 N-terminal DYKDDDDK Insect (sf21) ABL(ABL1) [E255K] HIS ABL(ABL1)[E255K] 08-094 Full-length 2-1130 NP_005148.2 N-terminal His Insect (sf21) HIS ABL(ABL1)[T315I] 08-093 Full-length 2-1130 NP_005148.2 N-terminal His Insect (sf21) ABL(ABL1) [T315I] BTN BTN-ABL(ABL1)[T315I] 08-493-20N Full-length 2-1130 NP_005148.2 N-terminal DYKDDDDK Insect (sf21) ACK(TNK2) GST ACK(TNK2) 08-196 Catalytic domain -
Customer Information Package Compound Profiling
COMPOUND PROFILING SERVICE CUSTOMER INFORMATION PACKAGE OUR CUSTOM KINASE INHIBITOR COMPOUND PROFILING SERVICE PERMIT CLIENTS TO HAVE THEIR CANDIDATE COMPOUNDS TESTED IN VITRO FOR INHIBITORY ACTIVITY TOWARDS MORE THAN 200 DIFFERENT HUMAN PROTEIN KINASES. THIS SERVICE IS IDEAL FOR ESTABLISHING THE SPECIFICITY OF A PROMISING THERAPEUTIC COMPOUND AGAINST A WIDE RANGE OF PROTEIN KINASES. THIS SERVICE INVOLVES THE MEASUREMENT OF ENZYMATIC ACTIVITIES OF PURIFIED RECOMBINANT PROTEIN KINASES IN [γ-32P or γ-33P] ATP-BASED ASSAYS. EGF Receptor with the inhibitor Erlotinib This information Package has been designed to assist you in using our Kinase Inhibitor Compound Profiling Service. We will endeavor to provide you with your results within three weeks of receipt of your compounds for testing. If after reviewing this information you have any questions about this service, please contact our Technical Service Represent- atives by calling toll free in North America 1-866-KINEXUS or (604) 323-2547 or by e-mail at "[email protected]". This information is regularly updated and available from our website at "www.kinexus.ca". Version 8NO3 TABLE OF CONTENTS Sample Preparation PDF Page No. 1. Introduction ………………………………………………………………………………….…………. 3 2. Quantity of compound required …………………………………………………………………… 5 3. Kinase assay conditions ……………………………………………………………………..………. 5 Shipping & Pricing 4. Shipping information ………………………………………………………………………………….. 5 5. Pricing information ……………………………………………………………………………………. 6 Description of Follow Up Services 6. Follow up services ……………………………………………………………………………………. 6 7. Forms to be completed ………………………………………………………………………………. 8 KinexTM Antibody Microarray Screening Services 8. Appendix A – List of available active protein kinases for compound profiling ……………….. 12 Forms to Complete and Return with your Samples 9. Service Order Form (KICP-SOF-01) ………………………………………………………………... 29 10. Service Identification Forms (KICP-SIF-01A and KICP-SIF-01B) ……………….…………...… 30 11. -

Gene Symbol Accession Alias/Prev Symbol Official Full Name AAK1 NM 014911.2 KIAA1048, Dkfzp686k16132 AP2 Associated Kinase 1
Gene Symbol Accession Alias/Prev Symbol Official Full Name AAK1 NM_014911.2 KIAA1048, DKFZp686K16132 AP2 associated kinase 1 (AAK1) AATK NM_001080395.2 AATYK, AATYK1, KIAA0641, LMR1, LMTK1, p35BP apoptosis-associated tyrosine kinase (AATK) ABL1 NM_007313.2 ABL, JTK7, c-ABL, p150 v-abl Abelson murine leukemia viral oncogene homolog 1 (ABL1) ABL2 NM_007314.3 ABLL, ARG v-abl Abelson murine leukemia viral oncogene homolog 2 (arg, Abelson-related gene) (ABL2) ACVR1 NM_001105.2 ACVRLK2, SKR1, ALK2, ACVR1A activin A receptor ACVR1B NM_004302.3 ACVRLK4, ALK4, SKR2, ActRIB activin A receptor, type IB (ACVR1B) ACVR1C NM_145259.2 ACVRLK7, ALK7 activin A receptor, type IC (ACVR1C) ACVR2A NM_001616.3 ACVR2, ACTRII activin A receptor ACVR2B NM_001106.2 ActR-IIB activin A receptor ACVRL1 NM_000020.1 ACVRLK1, ORW2, HHT2, ALK1, HHT activin A receptor type II-like 1 (ACVRL1) ADCK1 NM_020421.2 FLJ39600 aarF domain containing kinase 1 (ADCK1) ADCK2 NM_052853.3 MGC20727 aarF domain containing kinase 2 (ADCK2) ADCK3 NM_020247.3 CABC1, COQ8, SCAR9 chaperone, ABC1 activity of bc1 complex like (S. pombe) (CABC1) ADCK4 NM_024876.3 aarF domain containing kinase 4 (ADCK4) ADCK5 NM_174922.3 FLJ35454 aarF domain containing kinase 5 (ADCK5) ADRBK1 NM_001619.2 GRK2, BARK1 adrenergic, beta, receptor kinase 1 (ADRBK1) ADRBK2 NM_005160.2 GRK3, BARK2 adrenergic, beta, receptor kinase 2 (ADRBK2) AKT1 NM_001014431.1 RAC, PKB, PRKBA, AKT v-akt murine thymoma viral oncogene homolog 1 (AKT1) AKT2 NM_001626.2 v-akt murine thymoma viral oncogene homolog 2 (AKT2) AKT3 NM_181690.1 -
Macaca Mulatta) Exposed to Total‑Body Irradiation Yaoxiang Li1,6, Jatinder Singh2,3,6, Rency Varghese1, Yubo Zhang4, Oluseyi O
www.nature.com/scientificreports OPEN Transcriptome of rhesus macaque (Macaca mulatta) exposed to total‑body irradiation Yaoxiang Li1,6, Jatinder Singh2,3,6, Rency Varghese1, Yubo Zhang4, Oluseyi O. Fatanmi2,3, Amrita K. Cheema1,5 & Vijay K. Singh2,3* The feld of biodosimetry has seen a paradigm shift towards an increased use of molecular phenotyping technologies including omics and miRNA, in addition to conventional cytogenetic techniques. Here, we have used a nonhuman primate (NHP) model to study the impact of gamma‑ irradiation on alterations in blood‑based gene expression. With a goal to delineate radiation induced changes in gene expression, we followed eight NHPs for 60 days after exposure to 6.5 Gy gamma‑ radiation for survival outcomes. Analysis of diferential gene expression in response to radiation exposure yielded 26,944 dysregulated genes that were not signifcantly impacted by sex. Further analysis showed an increased association of several pathways including IL‑3 signaling, ephrin receptor signaling, ErbB signaling, nitric oxide signaling in the cardiovascular system, Wnt/β‑catenin signaling, and infammasome pathway, which were associated with positive survival outcomes in NHPs after acute exposure to radiation. This study provides novel insights into major pathways and networks involved in radiation‑induced injuries that may identify biomarkers for radiation injury. Te possible detonation of a radiological dispersal device or improvised nuclear device, accidental exposure to a radiation source, or nuclear accidents have led to the urgent need to develop essential analytic tools to assess such radiation exposures, especially radiation doses to exposed individuals. Biomarkers are important to assess the absorbed dose of radiation afer a radiological or nuclear accident, or afer the deliberate use of a radiation source to expose individuals 1–4. -

PRKD3 Promotes Malignant Progression of OSCC by Downregulating KLF16 Expression
European Review for Medical and Pharmacological Sciences 2020; 24: 12709-12716 PRKD3 promotes malignant progression of OSCC by downregulating KLF16 expression Z. CHEN1, Q. HUANG2, W. XU1, H. WANG1, J. YANG1, L.-J. ZHANG1 1Department of Oral and Maxillofacial Surgery, The First People’s Hospital of Lianyungang, Lianyungang, China 2Department of Oral and Maxillofacial Head and Neck Surgery, The Second People’s Hospital of Hefei, Hefei, China Abstract. – OBJECTIVE: We aimed to clari- Key Words: fy the molecular mechanism of how PRKD3 pro- PRKD3, KLF16, Oral squamous cell carcinoma, Ma- motes the malignant progression of oral squa- lignant progression. mous cell carcinoma (OSCC). PATIENTS AND METHODS: 62 cases of OS- CC tissues and normal adjacent ones which Introduction were further confirmed by a qualified pathol- ogist were collected from patients in the De- partment of Pathology and Stomatology of our Oral squamous cell carcinoma (OSCC), one hospital. PRKD3 expression in the above tis- of the major diseases endangering human health, sue samples was studied by quantitative re- refers to the squamous cell carcinoma of the oral al-time polymerase chain reaction (qRT-PCR) mucosa. It is the most common malignant tumor analysis, and its relationship with clinicopath- of the oral cavity, accounting for about 90% of the ological characteristics of these OSCC patients malignant tumors of the oral cavity1-3. Worldwide, was analyzed. Meanwhile, a PRKD3 knockdown there are about 405,000 new cases of OSCC and expression model was constructed in OSCC cell lines for cell functional experiments. The rela- about 211,000 deaths every year, and the 5-year 1,2 tionship between PRKD3 and KLF16 was eluci- survival rate is less than 60% . -

Targeting CDK4 Overcomes EMT-Mediated Tumor Heterogeneity and Therapeutic Resistance in KRAS Mutant Lung Cancer
Targeting CDK4 overcomes EMT-mediated tumor heterogeneity and therapeutic resistance in KRAS mutant lung cancer Aparna Padhye1,2, Jessica M. Konen1, B. Leticia Rodriguez1, Jared J. Fradette1, Joshua K. Ochieng1, Lixia Diao3, Jing Wang3, Wei Lu4, Luisa S. Solis4, Harsh Batra4, Maria G. Raso4, Michael D. Peoples5, Rosalba Minelli5, Alessandro Carugo5, Christopher A. Bristow5, Don L. Gibbons1,6* 1. Department of Thoracic/Head and Neck Medical Oncology, University of Texas MD Anderson Cancer Center, Houston, TX 77030, USA. 2. University of Texas Graduate School of Biomedical Sciences, Houston, TX 77030, USA. 3. Department of Bioinformatics and Computational Biology, University of Texas MD Anderson Cancer Center, Houston, TX 77030, USA. 4. Department of Translational Molecular Pathology, University of Texas MD Anderson Cancer Center, Houston, TX 77030, USA 5. TRACTION Platform, Division of Therapeutics Development, University of Texas MD Anderson Cancer Center, Houston, TX 77030, USA. 6. Department of Molecular and Cellular Oncology, University of Texas MD Anderson Cancer Center, Houston, TX 77030, USA. *Corresponding author. Email: [email protected] Supplemental Methods Plasmids, Transfections, and Lentiviral Generation and Transduction Transfections of si-RNAs werr performed using the Lipofectamine 2000 Transfection Reagent (Thermo Fisher Scientific). Constitutive Cdkn1a overexpression cell lines were generated by using Cdkn1a mouse Tagged ORF Clone (Origene (NM_007669)). Cdkn1a ORF was also subcloned into dox-inducible pTRIPZ-GFP vector to generate doxycycline inducible cell lines using EcoRI and AgeI restriction cut sites. Constitutive Cdkn1a shRNAs were purchased from Milipore sigma. The sequences used in the experiments are listed in table S11. Dox- inducible shRNAs were expressed in Tet-pLKO-puro vector with a scramble sequence as the non-targeting control.