Introduction to Drug Utilization Research 2003 Introduction to Drug Utilization Research
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Enoxaparin Sodium Solution for Injection, Manufacturer's Standard
PRODUCT MONOGRAPH INCLUDING PATIENT MEDICATION INFORMATION PrLOVENOX® Enoxaparin sodium solution for injection 30 mg in 0.3 mL solution (100 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 40 mg in 0.4 mL solution (100 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 60 mg in 0.6 mL solution (100 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 80 mg in 0.8 mL solution (100 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 100 mg in 1 mL solution (100 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 300 mg in 3 mL solution (100 mg/mL), multidose vials for subcutaneous or intravenous injection PrLOVENOX® HP Enoxaparin sodium (High Potency) solution for injection 120 mg in 0.8 mL solution (150 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 150 mg in 1 mL solution (150 mg/mL), pre-filled syringes for subcutaneous or intravenous injection Manufacturer’s standard Anticoagulant/Antithrombotic Agent ATC Code: B01AB05 Product Monograph – LOVENOX (enoxaparin) Page 1 of 113 sanofi-aventis Canada Inc. Date of Initial Approval: 2905 Place Louis-R.-Renaud February 9, 1993 Laval, Quebec H7V 0A3 Date of Revision September 7, 2021 Submission Control Number: 252514 s-a version 15.0 dated September 7, 2021 Product Monograph – LOVENOX (enoxaparin) Page 2 of 113 TABLE OF CONTENTS Sections or subsections that are not applicable at the time of authorization are not listed. TABLE OF CONTENTS .............................................................................................................. -

The Impact of a Changed Legislation on Reporting of Adverse Drug Reactions in Sweden, with Focus on Nurses Reporting
The impact of a changed legislation on reporting of adverse drug reactions in Sweden, with focus on nurses reporting Sofia A. Karlsson, Ingela Jacobsson, Marit Danell Boman, Katja M. Hakkarainen, Henrik Lövborg, Staffan Hägg and Anna K Jönsson Linköping University Post Print N.B.: When citing this work, cite the original article. The original publication is available at www.springerlink.com: Sofia A. Karlsson, Ingela Jacobsson, Marit Danell Boman, Katja M. Hakkarainen, Henrik Lövborg, Staffan Hägg and Anna K Jönsson, The impact of a changed legislation on reporting of adverse drug reactions in Sweden, with focus on nurses reporting, 2015, European Journal of Clinical Pharmacology, (71), 5, 631-636. http://dx.doi.org/10.1007/s00228-015-1839-6 Copyright: Springer Verlag (Germany) http://www.springerlink.com/?MUD=MP Postprint available at: Linköping University Electronic Press http://urn.kb.se/resolve?urn=urn:nbn:se:liu:diva-118037 The impact of a changed legislation on reporting of adverse drug reactions in Sweden, with focus on nurses’ reporting Sofia A Karlsson1, Ingela Jacobsson2, Marit Danell Boman3, Katja M Hakkarainen4,5, Henrik Lövborg2, Staffan Hägg2,5, Anna K Jönsson2 Affiliations: 1. Department of Public Health and Community Medicine, the Sahlgrenska Academy at University of Gothenburg, Gothenburg, Sweden 2. Department of Clinical Pharmacology and Department of Medical and Health Sciences, Linköping University, Linköping, Sweden 3. Division of Clinical Pharmacology, University Hospital of Umeå, Umeå, Sweden 4. Nordic School of -

Assessing the Availability, Service Quality, and Price of Essential Medicines In
Assessing the Availability, Service Quality, and Price of Essential Medicines in Private Pharmacies in Afghanistan Norio Kasahara A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Washington 2015 Reading Committee: Louis P. Garrison, Jr., Chair Joseph B. Babigumira Andy Stergachis Program Authorized to Offer Degree: Pharmaceutical Outcomes Research and Policy ©Copyright 2015 Norio Kasahara ii Table of Contents Abstract ................................................................................................................................................................................... ................................................................................................ ................................................................................................ .................................................................................. ............... vvv Acknowledgements ................................................................................................................................................................................... ................................................................................................ ................................................................................. ............ viiviivii Summary ................................................................................................................................................................................... ............................................................................................... -

Reseptregisteret 2013–2017 the Norwegian Prescription Database
LEGEMIDDELSTATISTIKK 2018:2 Reseptregisteret 2013–2017 Tema: Legemidler og eldre The Norwegian Prescription Database 2013–2017 Topic: Drug use in the elderly Reseptregisteret 2013–2017 Tema: Legemidler og eldre The Norwegian Prescription Database 2013–2017 Topic: Drug use in the elderly Christian Berg Hege Salvesen Blix Olaug Fenne Kari Furu Vidar Hjellvik Kari Jansdotter Husabø Irene Litleskare Marit Rønning Solveig Sakshaug Randi Selmer Anne-Johanne Søgaard Sissel Torheim Utgitt av Folkehelseinstituttet/Published by Norwegian Institute of Public Health Område for Helsedata og digitalisering Avdeling for Legemiddelstatistikk Juni 2018 Tittel/Title: Legemiddelstatistikk 2018:2 Reseptregisteret 2013–2017 / The Norwegian Prescription Database 2013–2017 Forfattere/Authors: Christian Berg, redaktør/editor Hege Salvesen Blix Olaug Fenne Kari Furu Vidar Hjellvik Kari Jansdotter Husabø Irene Litleskare Marit Rønning Solveig Sakshaug Randi Selmer Anne-Johanne Søgaard Sissel Torheim Acknowledgement: Julie D. W. Johansen (English text) Bestilling/Order: Rapporten kan lastes ned som pdf på Folkehelseinstituttets nettsider: www.fhi.no The report can be downloaded from www.fhi.no Grafisk design omslag: Fete Typer Ombrekking: Houston911 Kontaktinformasjon/Contact information: Folkehelseinstituttet/Norwegian Institute of Public Health Postboks 222 Skøyen N-0213 Oslo Tel: +47 21 07 70 00 ISSN: 1890-9647 ISBN: 978-82-8082-926-9 Sitering/Citation: Berg, C (red), Reseptregisteret 2013–2017 [The Norwegian Prescription Database 2013–2017] Legemiddelstatistikk 2018:2, Oslo, Norge: Folkehelseinstituttet, 2018. Tidligere utgaver / Previous editions: 2008: Reseptregisteret 2004–2007 / The Norwegian Prescription Database 2004–2007 2009: Legemiddelstatistikk 2009:2: Reseptregisteret 2004–2008 / The Norwegian Prescription Database 2004–2008 2010: Legemiddelstatistikk 2010:2: Reseptregisteret 2005–2009. Tema: Vanedannende legemidler / The Norwegian Prescription Database 2005–2009. -

Rtpa) for the Treatment of Hepatic Veno-Occlusive Disease (VOD
Bone Marrow Transplantation, (1999) 23, 803–807 1999 Stockton Press All rights reserved 0268–3369/99 $12.00 http://www.stockton-press.co.uk/bmt Recombinant tissue plasminogen activator (rtPA) for the treatment of hepatic veno-occlusive disease (VOD) S Kulkarni1, M Rodriguez2, A Lafuente2, P Mateos2, J Mehta1, S Singhal1, R Saso3, D Tait4, JG Treleaven3 and RL Powles1 Departments of 1Medical Oncology, 3Haematology and 4Radiotherapy, Royal Marsden NHS Trust, Sutton, Surrey, UK; and 2Haematology Department, Hospital La Paz, Madrid, Spain Summary: clinical syndrome characterized by hyperbilirubinemia, hepatomegaly and fluid retention,2,3 and results from dam- Seventeen patients who developed hepatic veno-occlus- age to structures in zone 3 of the liver acinus.4 In patients ive disease (VOD) following hematopoietic stem cell who have undergone hematopoietic stem cell transplan- transplantation were treated with recombinant tissue tation, chemoradiotherapy-induced endothelial cell damage plasminogen activator (rtPA) with or without heparin. is likely to be responsible for the pathogenesis of vessel rtPA was started a median of 13 days post transplant obstruction.5 (range 4–35). All patients received rtPA at a dose of 10 Treatment of established VOD has primarily been sup- mg/day as a starting dose, and 12 patients also received portive and any specific measures have resulted in little heparin (1500 U bolus; then 100 U/kg/day as a continu- impact on outcome. Based on the available evidence for ous i.v. infusion). The median number of days of rtPA involvement of hemostatic mechanisms and cytokines in therapy was 2.5 (1–12). The median total serum biliru- the pathogenesis of VOD,6–8 anti-thrombotic and anti-cyto- bin level was 116 mmol/l (range 63–194) at the begin- kine agents have been assessed for their role in treatment. -

Supplementary Appendix
Supplementary appendix Sipilä PN, Heikkilä N, Lindbohm JV, Hakulinen C, Vahtera J, Elovainio M, Suominen S, Väänänen A, Koskinen A, Nyberg ST, Pentti J, Strandberg TE, Kivimäki M. Hospital-treated infectious diseases and the risk of incident dementia: multicohort study with replication in the UK Biobank CONTENTS eFigure 1. Selection of participants in the study............................................................................... 2 eMethods 1. Study cohorts and data collection ................................................................................ 3 The Finnish Public Sector study (FPS)......................................................................................... 3 The Health and Social Support study (HeSSup) ........................................................................... 4 The Still Working study (STW) ................................................................................................... 5 The UK Biobank ......................................................................................................................... 5 eMethods 2. Proportionality of hazards ........................................................................................... 7 eFigure 2. Visualisation of hazard ratios over time using exponentiated scaled Schoenfeld residuals ....................................................................................................................................................... 8 eFigure 3. Dementia follow-up ..................................................................................................... -
![Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set](https://docslib.b-cdn.net/cover/8870/ehealth-dsi-ehdsi-v2-2-2-or-ehealth-dsi-master-value-set-1028870.webp)
Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set
MTC eHealth DSI [eHDSI v2.2.2-OR] eHealth DSI – Master Value Set Catalogue Responsible : eHDSI Solution Provider PublishDate : Wed Nov 08 16:16:10 CET 2017 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 1 of 490 MTC Table of Contents epSOSActiveIngredient 4 epSOSAdministrativeGender 148 epSOSAdverseEventType 149 epSOSAllergenNoDrugs 150 epSOSBloodGroup 155 epSOSBloodPressure 156 epSOSCodeNoMedication 157 epSOSCodeProb 158 epSOSConfidentiality 159 epSOSCountry 160 epSOSDisplayLabel 167 epSOSDocumentCode 170 epSOSDoseForm 171 epSOSHealthcareProfessionalRoles 184 epSOSIllnessesandDisorders 186 epSOSLanguage 448 epSOSMedicalDevices 458 epSOSNullFavor 461 epSOSPackage 462 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 2 of 490 MTC epSOSPersonalRelationship 464 epSOSPregnancyInformation 466 epSOSProcedures 467 epSOSReactionAllergy 470 epSOSResolutionOutcome 472 epSOSRoleClass 473 epSOSRouteofAdministration 474 epSOSSections 477 epSOSSeverity 478 epSOSSocialHistory 479 epSOSStatusCode 480 epSOSSubstitutionCode 481 epSOSTelecomAddress 482 epSOSTimingEvent 483 epSOSUnits 484 epSOSUnknownInformation 487 epSOSVaccine 488 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 3 of 490 MTC epSOSActiveIngredient epSOSActiveIngredient Value Set ID 1.3.6.1.4.1.12559.11.10.1.3.1.42.24 TRANSLATIONS Code System ID Code System Version Concept Code Description (FSN) 2.16.840.1.113883.6.73 2017-01 A ALIMENTARY TRACT AND METABOLISM 2.16.840.1.113883.6.73 2017-01 -

Transition of Anticoagulants 2019
Transition of Anticoagulants 2019 Van Hellerslia, PharmD, BCPS, CACP, Brand Generic Clinical Assistant Professor of Pharmacy Practice, Angiomax bivalirudin Temple University School of Pharmacy, Philadelphia, PA Arixtra fondaparinux Bevyxxa betrixaban Pallav Mehta, MD, Assistant Professor of Medicine, Coumadin warfarin Division of Hematology/Oncology, Eliquis apixaban MD Anderson Cancer Center at Cooper, Camden, NJ Fragmin dalteparin Lovenox enoxaparin Reviewer: Kelly Rudd, PharmD, BCPS, CACP, Pradaxa dabigatran Clinical Specialist, Anticoagulation, Bassett Medical Center, Savaysa edoxaban Cooperstown, NY Xarelto rivaroxaban From To Action Apixaban Argatroban/ Wait 12 hours after last dose of apixaban to initiate parenteral anticoagulant. In cases of Bivalirudin/ high bleeding risk, consider omitting initial bolus when transitioning to heparin infusion. Enoxaparin/ Dalteparin/ Fondaparinux/ Heparin Apixaban Warfarin When going from apixaban to warfarin, consider the use of parenteral anticoagulation as a bridge (eg, start heparin infusion or therapeutic enoxaparin AND warfarin 12 hours after last dose of apixaban and discontinue parenteral anticoagulant when INR is therapeutic). Apixaban affects INR so that initial INR measurements during the transition may not be useful for determining the appropriate dose of warfarin. Apixaban Betrixaban, Wait 12 hours from last dose of apixaban to initiate betrixaban, dabigatran, edoxaban, or Dabigatran, rivaroxaban. Edoxaban, or Rivaroxaban Argatroban Apixaban, Start apixaban, betrixaban, dabigatran, -

(Dipotassium Salt) and Heparin on the Estimation of Packed Cell Volume
J Clin Pathol: first published as 10.1136/jcp.19.2.196 on 1 March 1966. Downloaded from J. clin. Path. (1966), 19, 196 Effect of ethylene-diamine-tetra-acetic acid (dipotassium salt) and heparin on the estimation of packed cell volume C. A. PENNOCK AND K. W. JONES From the Department of Haematology, Gibson Laboratories, Radcliffe Infirmary, Oxford SYNOPSIS The effect of varying concentrations of ethylene-diamine-tetra-acetic acid (E.D.T.A.) (dipotassium salt) and heparin on the estimation of packed cell volume has been studied using a microhaematocrit method. Varying concentrations of E.D.T.A. can produce serious errors in estimation of packed cell volume (P.C.V.) and reliable results are only obtained within the range of 1 to 2 mg./ml. Heparin is a more suitable anticoagulant for this investigation as varying the con- centration has little effect. Storage with either anticoagulant at suitable concentrations for 24 hours at room temperature has little influence on the results. The estimation ofthe packed cell volume (P.C.V.) is bottles are often returned to this laboratory contain- regarded as a reliable investigation in the diagnosis ing less than the recommended amount of blood.copyright. of anaemia, and errors in the estimation of mean Ethylene-diamine-tetra-acetic acid is known to corpuscular haemoglobin concentration (M.C.H.C.) cause distortion and shrinkage of red cells and are thought to be due more often to errors in the to affect the estimation of P.C.V. by conventional estimation of haemoglobin than of the P.C.V. -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -
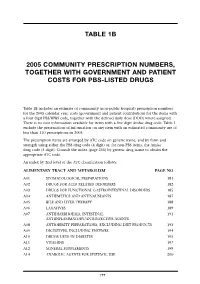
Table 1B 2005 Community Prescription Numbers, Together with Government
TABLE 1B 2005 COMMUNITY PRESCRIPTION NUMBERS, TOGETHER WITH GOVERNMENT AND PATIENT COSTS FOR PBS-LISTED DRUGS Table 1B includes an estimate of community (non-public hospital) prescription numbers for the 2005 calendar year, costs (government and patient contribution) for the items with a four digit PBS/RPBS code, together with the defined daily dose (DDD) where assigned. There is no cost information available for items with a five digit Amfac drug code. Table 1 exclude the presentation of information on any item with an estimated community use of less than 110 prescriptions in 2005. The prescription items are arranged by ATC code on generic name, and by form and strength using either the PBS drug code (4 digit) or, for non-PBS items, the Amfac drug code (5 digit). Consult the index (page 255) by generic drug name to obtain the appropriate ATC code. An index by 2nd level of the ATC classification follows: ALIMENTARY TRACT AND METABOLISM PAGE NO A01 STOMATOLOGICAL PREPARATIONS 181 A02 DRUGS FOR ACID RELATED DISORDERS 182 A03 DRUGS FOR FUNCTIONAL GASTROINTESTINAL DISORDERS 185 A04 ANTIEMETICS AND ANTINAUSEANTS 187 A05 BILE AND LIVER THERAPY 188 A06 LAXATIVES 189 A07 ANTIDIARRHOEALS, INTESTINAL 191 ANTIINFLAMMATORY/ANTIINFECTIVE AGENTS A08 ANTIOBESITY PREPARATIONS, EXCLUDING DIET PRODUCTS 193 A09 DIGESTIVES, INCLUDING ENZYMES 194 A10 DRUGS USED IN DIABETES 195 A11 VITAMINS 197 A12 MINERAL SUPPLEMENTS 199 A14 ANABOLIC AGENTS FOR SYSTEMIC USE 200 177 BLOOD AND BLOOD FORMING ORGANS B01 ANTITHROMBOTIC AGENTS 201 B02 ANTIHAEMORRHAGICS 203 B03 -

Direct Versus Indirect Thrombin Inhibition in Percutaneous Coronary Intervention
Direct Versus Indirect Thrombin Inhibition in Percutaneous Coronary Intervention Jonathan D. Marmur, MD, FACC Heparin rally occurring but slow thrombin inhibitor. The heparin:AT interaction produces conformational Heparin has been used to prevent intravascular changes in AT and accelerates its inhibition of throm- thrombosis and clotting on the surface of equipment bin, factor Xa, and factor IXa.10 used during percutaneous coronary interventions (PCI) Heparin catalysis of factor Xa inhibition does not since Andreas Gruentzig performed the first require bridging between factor Xa and AT. Since almost angioplasty.1 In fact, the development of coronary all the heparin chains are at least 18 units long, heparin angioplasty and of coronary artery bypass surgery would has equivalent inhibitory activity against thrombin and probably not have been possible without heparin. How- factor Xa.3 However, when thrombin is bound to fibrin, ever, with the availability of low molecular weight the heparin:AT complex is less able to access and inhibit heparin (LMWH) and the approval of bivalirudin, a thrombin.9 Furthermore, with respect to anti Xa activity, direct thrombin inhibitor for use during PCI, the ques- the heparin:AT complex is unable to inhibit factor Xa tion is more and more frequently asked whether heparin bound to the surface of activated platelets.11 should be replaced in PCI. The purpose of this paper is to critically review the evidence for the use of heparins Pharmacokinetics/pharmacodynamics. Heparin (indirect thrombin inhibitors) and direct thrombin must be given by injection since it is not absorbed when inhibitors during PCI. administered orally.10 Heparin is cleared via a biphasic process combining rapid saturable and slower first- Structure and mechanism of action of heparin.