Update on the Genetics of Autoinflammatory Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

TRNT1 Gene Trna Nucleotidyl Transferase 1
TRNT1 gene tRNA nucleotidyl transferase 1 Normal Function The TRNT1 gene provides instructions for making a protein involved in the production ( synthesis) of other proteins. During protein synthesis, a molecule called transfer RNA ( tRNA) helps assemble protein building blocks (amino acids) into a chain that forms the protein. Each tRNA carries a specific amino acid to the growing chain. The TRNT1 protein modifies tRNAs by adding a series of three DNA building blocks (nucleotides), called a CCA trinucleotide, to the molecule. This modification is essential for the correct amino acid to be attached to each tRNA. While most protein synthesis occurs in the fluid surrounding the nucleus (cytoplasm), some proteins are synthesized in cell structures called mitochondria, which are the energy-producing centers in cells. Many mitochondrial proteins form groups (complexes) that carry out the reactions that produce energy. Separate tRNA molecules are used to build proteins in the cytoplasm and mitochondria. The TRNT1 protein attaches the CCA trinucleotide to both cytoplasmic and mitochondrial tRNA molecules. Health Conditions Related to Genetic Changes TRNT1 deficiency More than 20 TRNT1 gene mutations have been found to cause TRNT1 deficiency, a condition with a range of signs and symptoms that affect many body systems. Features can include a blood disorder called sideroblastic anemia, recurrent fevers, a shortage of immune cells called B cells that leads to impairment of the immune system ( immunodeficiency), delayed development of speech and motor skills, and eye abnormalities that cause vision problems. The severity of the condition varies among affected individuals. The TRNT1 gene mutations that cause TRNT1 deficiency lead to a shortage (deficiency) of functional TRNT1 protein. -

Table 2. Significant
Table 2. Significant (Q < 0.05 and |d | > 0.5) transcripts from the meta-analysis Gene Chr Mb Gene Name Affy ProbeSet cDNA_IDs d HAP/LAP d HAP/LAP d d IS Average d Ztest P values Q-value Symbol ID (study #5) 1 2 STS B2m 2 122 beta-2 microglobulin 1452428_a_at AI848245 1.75334941 4 3.2 4 3.2316485 1.07398E-09 5.69E-08 Man2b1 8 84.4 mannosidase 2, alpha B1 1416340_a_at H4049B01 3.75722111 3.87309653 2.1 1.6 2.84852656 5.32443E-07 1.58E-05 1110032A03Rik 9 50.9 RIKEN cDNA 1110032A03 gene 1417211_a_at H4035E05 4 1.66015788 4 1.7 2.82772795 2.94266E-05 0.000527 NA 9 48.5 --- 1456111_at 3.43701477 1.85785922 4 2 2.8237185 9.97969E-08 3.48E-06 Scn4b 9 45.3 Sodium channel, type IV, beta 1434008_at AI844796 3.79536664 1.63774235 3.3 2.3 2.75319499 1.48057E-08 6.21E-07 polypeptide Gadd45gip1 8 84.1 RIKEN cDNA 2310040G17 gene 1417619_at 4 3.38875643 1.4 2 2.69163229 8.84279E-06 0.0001904 BC056474 15 12.1 Mus musculus cDNA clone 1424117_at H3030A06 3.95752801 2.42838452 1.9 2.2 2.62132809 1.3344E-08 5.66E-07 MGC:67360 IMAGE:6823629, complete cds NA 4 153 guanine nucleotide binding protein, 1454696_at -3.46081884 -4 -1.3 -1.6 -2.6026947 8.58458E-05 0.0012617 beta 1 Gnb1 4 153 guanine nucleotide binding protein, 1417432_a_at H3094D02 -3.13334396 -4 -1.6 -1.7 -2.5946297 1.04542E-05 0.0002202 beta 1 Gadd45gip1 8 84.1 RAD23a homolog (S. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -
Supplementary File 2A Revised
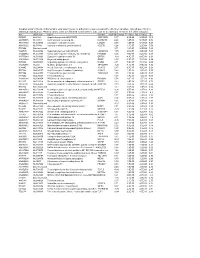
Supplementary file 2A. Differentially expressed genes in aldosteronomas compared to all other samples, ranked according to statistical significance. Missing values were not allowed in aldosteronomas, but to a maximum of five in the other samples. Acc UGCluster Name Symbol log Fold Change P - Value Adj. P-Value B R99527 Hs.8162 Hypothetical protein MGC39372 MGC39372 2,17 6,3E-09 5,1E-05 10,2 AA398335 Hs.10414 Kelch domain containing 8A KLHDC8A 2,26 1,2E-08 5,1E-05 9,56 AA441933 Hs.519075 Leiomodin 1 (smooth muscle) LMOD1 2,33 1,3E-08 5,1E-05 9,54 AA630120 Hs.78781 Vascular endothelial growth factor B VEGFB 1,24 1,1E-07 2,9E-04 7,59 R07846 Data not found 3,71 1,2E-07 2,9E-04 7,49 W92795 Hs.434386 Hypothetical protein LOC201229 LOC201229 1,55 2,0E-07 4,0E-04 7,03 AA454564 Hs.323396 Family with sequence similarity 54, member B FAM54B 1,25 3,0E-07 5,2E-04 6,65 AA775249 Hs.513633 G protein-coupled receptor 56 GPR56 -1,63 4,3E-07 6,4E-04 6,33 AA012822 Hs.713814 Oxysterol bining protein OSBP 1,35 5,3E-07 7,1E-04 6,14 R45592 Hs.655271 Regulating synaptic membrane exocytosis 2 RIMS2 2,51 5,9E-07 7,1E-04 6,04 AA282936 Hs.240 M-phase phosphoprotein 1 MPHOSPH -1,40 8,1E-07 8,9E-04 5,74 N34945 Hs.234898 Acetyl-Coenzyme A carboxylase beta ACACB 0,87 9,7E-07 9,8E-04 5,58 R07322 Hs.464137 Acyl-Coenzyme A oxidase 1, palmitoyl ACOX1 0,82 1,3E-06 1,2E-03 5,35 R77144 Hs.488835 Transmembrane protein 120A TMEM120A 1,55 1,7E-06 1,4E-03 5,07 H68542 Hs.420009 Transcribed locus 1,07 1,7E-06 1,4E-03 5,06 AA410184 Hs.696454 PBX/knotted 1 homeobox 2 PKNOX2 1,78 2,0E-06 -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

The KMT1A-GATA3-STAT3 Circuit Is a Novel Self-Renewal Signaling of Human Bladder Cancer Stem Cells Zhao Yang1, Luyun He2,3, Kais
The KMT1A-GATA3-STAT3 circuit is a novel self-renewal signaling of human bladder cancer stem cells Zhao Yang1, Luyun He2,3, Kaisu Lin4, Yun Zhang1, Aihua Deng1, Yong Liang1, Chong Li2, 5, & Tingyi Wen1, 6, 1CAS Key Laboratory of Pathogenic Microbiology and Immunology, Institute of Microbiology, Chinese Academy of Sciences, Beijing 100101, China 2Core Facility for Protein Research, Institute of Biophysics, Chinese Academy of Sciences, Beijing 100101, China 3CAS Key Laboratory of Infection and Immunity, Institute of Biophysics, Chinese Academy of Sciences, Beijing 100101, China 4Department of Oncology, the Second Affiliated Hospital of Soochow University, Suzhou 215000, China 5Beijing Jianlan Institute of Medicine, Beijing 100190, China 6Savaid Medical School, University of Chinese Academy of Sciences, Beijing 100049, China Correspondence author: Tingyi Wen, e-mail: [email protected] Chong Li, e-mail: [email protected] Supplementary Figure S1. Isolation of human bladder cancer stem cells. BCMab1 and CD44 were used to isolate bladder cancer stem cells (BCSCs: BCMab1+CD44+) and bladder cancer non-stem cells (BCNSCs: BCMab1-CD44-) from EJ, samples #1 and #2 by flow cytometry. Supplementary Figure S2. Gene ontology analysis of downregulated genes of human BCSCs. (A) Pathway enrichment of 103 downregulated genes in BCSCs. (B) The seven downregulated genes in BCSCs participating in centromeric heterochromatin, mRNA-3’-UTR binding and translation regulator activity signaling pathways were validated by qRT-PCR. Data are presented as mean ± SD. P < 0.05; P < 0.01. Supplementary Figure S3. The expression of KMT1A is higher in human BC than that in peri-tumor tissues. (A) The expression of KMT1A was higher in BC samples than that in peri-tumors as assessed by immunohistochemistry, Scale bar = 50 m. -

Human Induced Pluripotent Stem Cell–Derived Podocytes Mature Into Vascularized Glomeruli Upon Experimental Transplantation
BASIC RESEARCH www.jasn.org Human Induced Pluripotent Stem Cell–Derived Podocytes Mature into Vascularized Glomeruli upon Experimental Transplantation † Sazia Sharmin,* Atsuhiro Taguchi,* Yusuke Kaku,* Yasuhiro Yoshimura,* Tomoko Ohmori,* ‡ † ‡ Tetsushi Sakuma, Masashi Mukoyama, Takashi Yamamoto, Hidetake Kurihara,§ and | Ryuichi Nishinakamura* *Department of Kidney Development, Institute of Molecular Embryology and Genetics, and †Department of Nephrology, Faculty of Life Sciences, Kumamoto University, Kumamoto, Japan; ‡Department of Mathematical and Life Sciences, Graduate School of Science, Hiroshima University, Hiroshima, Japan; §Division of Anatomy, Juntendo University School of Medicine, Tokyo, Japan; and |Japan Science and Technology Agency, CREST, Kumamoto, Japan ABSTRACT Glomerular podocytes express proteins, such as nephrin, that constitute the slit diaphragm, thereby contributing to the filtration process in the kidney. Glomerular development has been analyzed mainly in mice, whereas analysis of human kidney development has been minimal because of limited access to embryonic kidneys. We previously reported the induction of three-dimensional primordial glomeruli from human induced pluripotent stem (iPS) cells. Here, using transcription activator–like effector nuclease-mediated homologous recombination, we generated human iPS cell lines that express green fluorescent protein (GFP) in the NPHS1 locus, which encodes nephrin, and we show that GFP expression facilitated accurate visualization of nephrin-positive podocyte formation in -

Protein Symbol Protein Name Rank Metric Score 4F2 4F2 Cell-Surface
Supplementary Table 2 Supplementary Table 2. Ranked list of proteins present in anti-Sema4D treated macrophage conditioned media obtained in the GSEA analysis of the proteomic data. Proteins are listed according to their rank metric score, which is the score used to position the gene in the ranked list of genes of the GSEA. Values are obtained from comparing Sema4D treated RAW conditioned media versus REST, which includes untreated, IgG treated and anti-Sema4D added RAW conditioned media. GSEA analysis was performed under standard conditions in November 2015. Protein Rank metric symbol Protein name score 4F2 4F2 cell-surface antigen heavy chain 2.5000 PLOD3 Procollagen-lysine,2-oxoglutarate 5-dioxygenase 3 1.4815 ELOB Transcription elongation factor B polypeptide 2 1.4350 ARPC5 Actin-related protein 2/3 complex subunit 5 1.2603 OSTF1 teoclast-stimulating factor 1 1.2500 RL5 60S ribomal protein L5 1.2135 SYK Lysine--tRNA ligase 1.2135 RL10A 60S ribomal protein L10a 1.2135 TXNL1 Thioredoxin-like protein 1 1.1716 LIS1 Platelet-activating factor acetylhydrolase IB subunit alpha 1.1067 A4 Amyloid beta A4 protein 1.0911 H2B1M Histone H2B type 1-M 1.0514 UB2V2 Ubiquitin-conjugating enzyme E2 variant 2 1.0381 PDCD5 Programmed cell death protein 5 1.0373 UCHL3 Ubiquitin carboxyl-terminal hydrolase isozyme L3 1.0061 PLEC Plectin 1.0061 ITPA Inine triphphate pyrophphatase 0.9524 IF5A1 Eukaryotic translation initiation factor 5A-1 0.9314 ARP2 Actin-related protein 2 0.8618 HNRPL Heterogeneous nuclear ribonucleoprotein L 0.8576 DNJA3 DnaJ homolog subfamily -

Set2-Mediated Alternative Splicing of Srsf11 Regulates Cocaine Reward Behavior
bioRxiv preprint doi: https://doi.org/10.1101/798009; this version posted October 8, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Graphic Legend: Epigenetic editing enriches H3K36me3 at the gene for Srsf11, a splice factor. Enrichment of H3K36me3 causes alternative splicing of Srsf11, in the form of increased intron retention. After this manipulation in a brain reward region, mice show greater preference for a cocaine reward. bioRxiv preprint doi: https://doi.org/10.1101/798009; this version posted October 8, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Summary Alternative splicing is a key mechanism for neuronal gene regulation, and is grossly altered in mouse brain reward regions following investigator-administered cocaine. It is well established that cocaine epigenetically regulates transcription, yet mechanism(s) by which cocaine-induced epigenetic modifications regulate alternative splicing is largely unexplored. Our group and others have previously identified the histone modification, H3K36me3, as a putative splicing regulator. However, it has not yet been possible to establish the direct causal relevance of this modification to alternative splicing in brain or any other context. We found that mouse cocaine self-administration caused widespread alternative splicing, concomitant with enrichment of H3K36me3 at splice junctions. -

Supplementary Figure and Tables
USP24-GSDMB complex promotes bladder cancer proliferation via activation of the STAT3 pathway Haiqing He, Lu Yi, Bin Zhang, Bin Yan, Ming Xiao, Jiannan Ren, Dong Zi, Liang Zhu, Zhaohui Zhong, Xiaokun Zhao, Xin Jin, Wei Xiong Supplementary figure 1. A and B, T24 and 5637 cells were infected with indicated constructs for 48 h. The cells were harvested for cell cycle assay (A) and transwell invasion assay (B). Data presented as three replicates. ns, not significant; *, P < 0.05; ***, P < 0.001. Table S1: Sequences of RT-qPCR primers Species Gene Forward (5’-3’) Reverse (5’-3’) Human GAPDH CCAGAACATCATCCCTGCCT CCTGCTTCACCACCTTCTTG Human HK2 TCTATGCCATCCCTGAGGAC TCTCTGCCTTCCACTCCACT Human LDHA GGCCTGTGCCATCAGTATCT CGCTTCCAATAACACGGTTT Human ENO2 GAAGAAAAGGCCTGCAACTG CCAGGTCAGCAATGAATGTG Human GSDMB AGTCTTTGGGTTCGGAGGAT CTTGTCTGGGTCCTCCATGT Human IGFBP3 CCTGCCGTAGAGAAATGGAA AGGCTGCCCATACTTATCCA Table S2: Sequences of ChIP-qPCR primers Species Gene Forward (5’-3’) Reverse (5’-3’) Human IGFBP3 CCCCTGGGGATATAAACAGC GCATTCGTGTGTACCTCGTG Table S3: Sequences of gene-specific shRNAs shGSDMB-1 5′- CCGGGCCTTGTTGATGCTGATAGATCTCGAGATCTATCAGCATCAACAAGGCTTTTTT G-3′ shGSDMB-2 5′- CCGGGCTGTATGTTGTTGTCTCTATCTCGAGATAGAGACAACAACATACAGCTTT TTTG-3′ shSTAT3 5′- CCGGGCACAATCTACGAAGAATCAACTCGAGTTGATTCTTCGTAGATTGTGCTTTTTG -3′ shUSP24-1 5′- CCGGCTCTCGTATGTAACGTATTTGCTCGAGCAAATACGTTACATACGAGAGTTTTTG TG-3′ shUSP24-2 5′- CCGGACAATACTGTGACCGTATAAACTCGAGTTTATACGGTCACAGTATTGTTTTTTG -3′ gene_id si-GSDMB si-NC log2FoldChangepvalue padj gene_namegene_chr gene_start ENSG0000014667410533.42 -

Transcriptomic and Proteomic Landscape of Mitochondrial
TOOLS AND RESOURCES Transcriptomic and proteomic landscape of mitochondrial dysfunction reveals secondary coenzyme Q deficiency in mammals Inge Ku¨ hl1,2†*, Maria Miranda1†, Ilian Atanassov3, Irina Kuznetsova4,5, Yvonne Hinze3, Arnaud Mourier6, Aleksandra Filipovska4,5, Nils-Go¨ ran Larsson1,7* 1Department of Mitochondrial Biology, Max Planck Institute for Biology of Ageing, Cologne, Germany; 2Department of Cell Biology, Institute of Integrative Biology of the Cell (I2BC) UMR9198, CEA, CNRS, Univ. Paris-Sud, Universite´ Paris-Saclay, Gif- sur-Yvette, France; 3Proteomics Core Facility, Max Planck Institute for Biology of Ageing, Cologne, Germany; 4Harry Perkins Institute of Medical Research, The University of Western Australia, Nedlands, Australia; 5School of Molecular Sciences, The University of Western Australia, Crawley, Australia; 6The Centre National de la Recherche Scientifique, Institut de Biochimie et Ge´ne´tique Cellulaires, Universite´ de Bordeaux, Bordeaux, France; 7Department of Medical Biochemistry and Biophysics, Karolinska Institutet, Stockholm, Sweden Abstract Dysfunction of the oxidative phosphorylation (OXPHOS) system is a major cause of human disease and the cellular consequences are highly complex. Here, we present comparative *For correspondence: analyses of mitochondrial proteomes, cellular transcriptomes and targeted metabolomics of five [email protected] knockout mouse strains deficient in essential factors required for mitochondrial DNA gene (IKu¨ ); expression, leading to OXPHOS dysfunction. Moreover, -

Mitochondrial DNA Transcription and Translation: Clinical Syndromes
Essays in Biochemistry (2018) EBC20170103 https://doi.org/10.1042/EBC20170103 Review Article Mitochondrial DNA transcription and translation: clinical syndromes Veronika Boczonadi1,*, Giulia Ricci1,2,* and Rita Horvath1 1Wellcome Centre for Mitochondrial Research, Institute of Genetic Medicine, Newcastle University, Central Parkway, Newcastle upon Tyne NE1 3BZ, U.K.; 2Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy Correspondence: Rita Horvath ([email protected]) Diagnosing primary mitochondrial diseases is challenging in clinical practice. Although, de- fective oxidative phosphorylation (OXPHOS) is the common final pathway, it is unknown why different mtDNA or nuclear mutations result in largely heterogeneous and often tis- sue -specific clinical presentations. Mitochondrial tRNA (mt-tRNA) mutations are frequent causes of mitochondrial diseases both in children and adults. However numerous nu- clear mutations involved in mitochondrial protein synthesis affecting ubiquitously expressed genes have been reported in association with very tissue specific clinical manifestations suggesting that there are so far unknown factors determining the tissue specificity in mi- tochondrial translation. Most of these gene defects result in histological abnormalities and multiple respiratory chain defects in the affected organs. The clinical phenotypes are usu- ally early-onset, severe, and often fatal, implying the importance of mitochondrial transla- tion from birth. However, some rare, reversible infantile mitochondrial diseases are caused by very specific defects of mitochondrial translation. An unbiased genetic approach (whole exome sequencing, RNA sequencing) combined with proteomics and functional studies re- vealed novel factors involved in mitochondrial translation which contribute to the clinical manifestation and recovery in these rare reversible mitochondrial conditions. Introduction All eukaryotic cells contain both genomic and mtDNA and two separate protein synthesis machineries [1].