IDCM Section 3: Spotted Fever Rickettsiosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Molecular Evidence of Novel Spotted Fever Group Rickettsia
pathogens Article Molecular Evidence of Novel Spotted Fever Group Rickettsia Species in Amblyomma albolimbatum Ticks from the Shingleback Skink (Tiliqua rugosa) in Southern Western Australia Mythili Tadepalli 1, Gemma Vincent 1, Sze Fui Hii 1, Simon Watharow 2, Stephen Graves 1,3 and John Stenos 1,* 1 Australian Rickettsial Reference Laboratory, University Hospital Geelong, Geelong 3220, Australia; [email protected] (M.T.); [email protected] (G.V.); [email protected] (S.F.H.); [email protected] (S.G.) 2 Reptile Victoria Inc., Melbourne 3035, Australia; [email protected] 3 Department of Microbiology and Infectious Diseases, Nepean Hospital, NSW Health Pathology, Penrith 2747, Australia * Correspondence: [email protected] Abstract: Tick-borne infectious diseases caused by obligate intracellular bacteria of the genus Rick- ettsia are a growing global problem to human and animal health. Surveillance of these pathogens at the wildlife interface is critical to informing public health strategies to limit their impact. In Australia, reptile-associated ticks such as Bothriocroton hydrosauri are the reservoirs for Rickettsia honei, the causative agent of Flinders Island spotted fever. In an effort to gain further insight into the potential for reptile-associated ticks to act as reservoirs for rickettsial infection, Rickettsia-specific PCR screening was performed on 64 Ambylomma albolimbatum ticks taken from shingleback skinks (Tiliqua rugosa) lo- cated in southern Western Australia. PCR screening revealed 92% positivity for rickettsial DNA. PCR Citation: Tadepalli, M.; Vincent, G.; amplification and sequencing of phylogenetically informative rickettsial genes (ompA, ompB, gltA, Hii, S.F.; Watharow, S.; Graves, S.; Stenos, J. -

Distribution of Tick-Borne Diseases in China Xian-Bo Wu1, Ren-Hua Na2, Shan-Shan Wei2, Jin-Song Zhu3 and Hong-Juan Peng2*
Wu et al. Parasites & Vectors 2013, 6:119 http://www.parasitesandvectors.com/content/6/1/119 REVIEW Open Access Distribution of tick-borne diseases in China Xian-Bo Wu1, Ren-Hua Na2, Shan-Shan Wei2, Jin-Song Zhu3 and Hong-Juan Peng2* Abstract As an important contributor to vector-borne diseases in China, in recent years, tick-borne diseases have attracted much attention because of their increasing incidence and consequent significant harm to livestock and human health. The most commonly observed human tick-borne diseases in China include Lyme borreliosis (known as Lyme disease in China), tick-borne encephalitis (known as Forest encephalitis in China), Crimean-Congo hemorrhagic fever (known as Xinjiang hemorrhagic fever in China), Q-fever, tularemia and North-Asia tick-borne spotted fever. In recent years, some emerging tick-borne diseases, such as human monocytic ehrlichiosis, human granulocytic anaplasmosis, and a novel bunyavirus infection, have been reported frequently in China. Other tick-borne diseases that are not as frequently reported in China include Colorado fever, oriental spotted fever and piroplasmosis. Detailed information regarding the history, characteristics, and current epidemic status of these human tick-borne diseases in China will be reviewed in this paper. It is clear that greater efforts in government management and research are required for the prevention, control, diagnosis, and treatment of tick-borne diseases, as well as for the control of ticks, in order to decrease the tick-borne disease burden in China. Keywords: Ticks, Tick-borne diseases, Epidemic, China Review (Table 1) [2,4]. Continuous reports of emerging tick-borne Ticks can carry and transmit viruses, bacteria, rickettsia, disease cases in Shandong, Henan, Hebei, Anhui, and spirochetes, protozoans, Chlamydia, Mycoplasma,Bartonia other provinces demonstrate the rise of these diseases bodies, and nematodes [1,2]. -
Vectorborne Zoonoses: Break-Out Session Epidemiology and Laboratory Capacity Workshop – Oct
Texas Department of State Health Services Vectorborne Zoonoses: Break-out Session Epidemiology and Laboratory Capacity Workshop – Oct. 2018 DSHS Zoonosis Control Branch Session Topics Texas Department of State Health Services • NEDSS case investigation tips • Lyme disease • Rickettsial diseases • Arboviral diseases ELC 2018 - Vectorborne Diseases 2 Texas Department of State Health Services Don’t be a Reject! Helpful tips to keep your notification from being rejected ELC breakout session October 3, 2018 Kamesha Owens, MPH Zoonosis Control Branch Texas Department of State Health Services Objectives • Rejection Criteria • How to document in NBS (NEDSS) • How to Report Texas Department of State Health Services 10/3/2018 ELC 2018 - Vectorborne Diseases 4 Rejection Criteria Texas Department of State Health Services Missing/incorrect information: • Incorrect case status or condition selected • Full Name • Date of Birth • Address • County • Missing laboratory data 10/3/2018 ELC 2018 - Vectorborne Diseases 5 Rejection Criteria continued Texas Department of State Health Services • Inconsistent information • e.g. Report date is a week before onset date • Case investigation form not received by ZCB within 14 days of notification • ZCB recommends that notification not be created until the case is closed and the investigation form has been submitted 10/3/2018 ELC 2018 - Vectorborne Diseases 6 Rejection Criteria continued Texas Department of State Health Services • Condition-specific information necessary to report the case is missing: • Travel history for Zika and other non-endemic conditions • Evidence of neurological disease for WNND case • Supporting documentation for Lyme disease case determination 10/3/2018 ELC 2018 - Vectorborne Diseases 7 How to Document in NBS (NEDSS) Do Don’t Add detailed comments in designated Leave us guessing! comments box under case info tab. -

Parinaud's Oculoglandular Syndrome
Tropical Medicine and Infectious Disease Case Report Parinaud’s Oculoglandular Syndrome: A Case in an Adult with Flea-Borne Typhus and a Review M. Kevin Dixon 1, Christopher L. Dayton 2 and Gregory M. Anstead 3,4,* 1 Baylor Scott & White Clinic, 800 Scott & White Drive, College Station, TX 77845, USA; [email protected] 2 Division of Critical Care, Department of Medicine, University of Texas Health, San Antonio, 7703 Floyd Curl Drive, San Antonio, TX 78229, USA; [email protected] 3 Medical Service, South Texas Veterans Health Care System, San Antonio, TX 78229, USA 4 Division of Infectious Diseases, Department of Medicine, University of Texas Health, San Antonio, 7703 Floyd Curl Drive, San Antonio, TX 78229, USA * Correspondence: [email protected]; Tel.: +1-210-567-4666; Fax: +1-210-567-4670 Received: 7 June 2020; Accepted: 24 July 2020; Published: 29 July 2020 Abstract: Parinaud’s oculoglandular syndrome (POGS) is defined as unilateral granulomatous conjunctivitis and facial lymphadenopathy. The aims of the current study are to describe a case of POGS with uveitis due to flea-borne typhus (FBT) and to present a diagnostic and therapeutic approach to POGS. The patient, a 38-year old man, presented with persistent unilateral eye pain, fever, rash, preauricular and submandibular lymphadenopathy, and laboratory findings of FBT: hyponatremia, elevated transaminase and lactate dehydrogenase levels, thrombocytopenia, and hypoalbuminemia. His condition rapidly improved after starting doxycycline. Soon after hospitalization, he was diagnosed with uveitis, which responded to topical prednisolone. To derive a diagnostic and empiric therapeutic approach to POGS, we reviewed the cases of POGS from its various causes since 1976 to discern epidemiologic clues and determine successful diagnostic techniques and therapies; we found multiple cases due to cat scratch disease (CSD; due to Bartonella henselae) (twelve), tularemia (ten), sporotrichosis (three), Rickettsia conorii (three), R. -

Recognizing and Treating New and Emerging Infections Encountered in Everyday Practice
Recognizing and treating new and emerging infections encountered in everyday practice STEVEN M. GORDON, MD NFECTIOUS DISEASES, pre- MiikWirj:« Although infectious diseases were once considered a dicted earlier in this cen- diminishing threat, new pathogens are constantly challenging tury to be eliminated as a the health care system. This article reviews the clinical presen- public health problem, re- tation, diagnosis, and treatment of seven emerging infections I main the chief cause of death that primary care physicians are likely to encounter. worldwide and a significant cause of death and morbidity in i Parvovirus B19 attacks erythrocyte precursors; the United States.1 Challenging infection is usually benign and self-limiting but can cause the US public health system are aplastic crises in patients with chronic hemolytic disorders. several newly identified patho- Hemorrhagic colitis due to Escherichia coli 0157:H7 infection gens (eg, human immunodefi- can lead to the hemolytic-uremic syndrome, especially in chil- ciency virus [HIV], Escherichia dren; it also can cause thrombotic thrombocytopenia purpura. coli 0157:H7, hepatitis C) and a Chlamydia pneumoniae causes a mild pneumonia that resem- resurgence of old diseases pre- bles mycoplasmal pneumonia. Bacillary angiomatosis primar- sumed to be under control (eg, ily affects immunocompromised patients, especially those tuberculosis, syphilis). Further, infected with human immunodeficiency virus (HIV). At least multiple-drug resistance in two organisms can cause bacillary angiomatosis: Bartonella hense- strains of pneumococci, gono- lae and Bartonella quintana. Hantavirus pulmonary syndrome cocci, enterococci, staphylo- is spread by exposure to the droppings of infected rodents. cocci, salmonella, and mycobac- Contrary to previous thought, HIV continues to replicate teria undermines efforts to throughout the course of the illness and does not have a latency control the diseases they cause.2 phase. -

Lyme Disease Weather Also Means That Ticks Become More Active and This Can Agent by Feeding As Larvae on Certain Rodent Species
Spring and summer bring warm temperatures, just right for small and medium sized animals, but will also feed on people. walking in the woods and other outdoor activities. Warm These ticks typically become infected with the Lyme disease weather also means that ticks become more active and this can agent by feeding as larvae on certain rodent species. increase the risk of a tick-borne disease. The tick-borne dis- In the fall, the nymphs become adults and infected nymphs eases that occur most often in Virginia are Lyme disease, become infected adults. Adult blacklegged ticks prefer to feed Rocky Mountain spotted fever, and ehrlichiosis. on deer. However, adult ticks will occasionally bite people on warm days of the fall and winter and can transmit Lyme disease Lyme Disease at that time. Lyme disease is caused by infection with a bacterium called Borrelia burgdorferi. The number of Lyme disease cases Transmission of Lyme disease by the nymph or adult ticks reported in Virginia has increased substantially in recent years. does not occur until the tick has been attached and feeding on a human or animal host for at least 36 hours. The Tick The blacklegged tick (Ixodes scapularis), formerly known as The Symptoms the deer tick, is the only carrier of Lyme disease in the Eastern Between three days to several weeks after being bitten by an U.S. The blacklegged tick's name comes from it being the only infected tick, 70-90% of people develop a circular or oval rash, tick in the Eastern U.S. that bites humans and has legs that are called erythema migrans (or EM), at the site of the bite. -

Babela Massiliensis, a Representative of a Widespread Bacterial
Babela massiliensis, a representative of a widespread bacterial phylum with unusual adaptations to parasitism in amoebae Isabelle Pagnier, Natalya Yutin, Olivier Croce, Kira S Makarova, Yuri I Wolf, Samia Benamar, Didier Raoult, Eugene V. Koonin, Bernard La Scola To cite this version: Isabelle Pagnier, Natalya Yutin, Olivier Croce, Kira S Makarova, Yuri I Wolf, et al.. Babela mas- siliensis, a representative of a widespread bacterial phylum with unusual adaptations to parasitism in amoebae. Biology Direct, BioMed Central, 2015, 10 (13), 10.1186/s13062-015-0043-z. hal-01217089 HAL Id: hal-01217089 https://hal-amu.archives-ouvertes.fr/hal-01217089 Submitted on 19 Oct 2015 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Pagnier et al. Biology Direct (2015) 10:13 DOI 10.1186/s13062-015-0043-z RESEARCH Open Access Babela massiliensis, a representative of a widespread bacterial phylum with unusual adaptations to parasitism in amoebae Isabelle Pagnier1, Natalya Yutin2, Olivier Croce1, Kira S Makarova2, Yuri I Wolf2, Samia Benamar1, Didier Raoult1, Eugene V Koonin2 and Bernard La Scola1* Abstract Background: Only a small fraction of bacteria and archaea that are identifiable by metagenomics can be grown on standard media. -

Diagnostic Code Descriptions (ICD9)
INFECTIONS AND PARASITIC DISEASES INTESTINAL AND INFECTIOUS DISEASES (001 – 009.3) 001 CHOLERA 001.0 DUE TO VIBRIO CHOLERAE 001.1 DUE TO VIBRIO CHOLERAE EL TOR 001.9 UNSPECIFIED 002 TYPHOID AND PARATYPHOID FEVERS 002.0 TYPHOID FEVER 002.1 PARATYPHOID FEVER 'A' 002.2 PARATYPHOID FEVER 'B' 002.3 PARATYPHOID FEVER 'C' 002.9 PARATYPHOID FEVER, UNSPECIFIED 003 OTHER SALMONELLA INFECTIONS 003.0 SALMONELLA GASTROENTERITIS 003.1 SALMONELLA SEPTICAEMIA 003.2 LOCALIZED SALMONELLA INFECTIONS 003.8 OTHER 003.9 UNSPECIFIED 004 SHIGELLOSIS 004.0 SHIGELLA DYSENTERIAE 004.1 SHIGELLA FLEXNERI 004.2 SHIGELLA BOYDII 004.3 SHIGELLA SONNEI 004.8 OTHER 004.9 UNSPECIFIED 005 OTHER FOOD POISONING (BACTERIAL) 005.0 STAPHYLOCOCCAL FOOD POISONING 005.1 BOTULISM 005.2 FOOD POISONING DUE TO CLOSTRIDIUM PERFRINGENS (CL.WELCHII) 005.3 FOOD POISONING DUE TO OTHER CLOSTRIDIA 005.4 FOOD POISONING DUE TO VIBRIO PARAHAEMOLYTICUS 005.8 OTHER BACTERIAL FOOD POISONING 005.9 FOOD POISONING, UNSPECIFIED 006 AMOEBIASIS 006.0 ACUTE AMOEBIC DYSENTERY WITHOUT MENTION OF ABSCESS 006.1 CHRONIC INTESTINAL AMOEBIASIS WITHOUT MENTION OF ABSCESS 006.2 AMOEBIC NONDYSENTERIC COLITIS 006.3 AMOEBIC LIVER ABSCESS 006.4 AMOEBIC LUNG ABSCESS 006.5 AMOEBIC BRAIN ABSCESS 006.6 AMOEBIC SKIN ULCERATION 006.8 AMOEBIC INFECTION OF OTHER SITES 006.9 AMOEBIASIS, UNSPECIFIED 007 OTHER PROTOZOAL INTESTINAL DISEASES 007.0 BALANTIDIASIS 007.1 GIARDIASIS 007.2 COCCIDIOSIS 007.3 INTESTINAL TRICHOMONIASIS 007.8 OTHER PROTOZOAL INTESTINAL DISEASES 007.9 UNSPECIFIED 008 INTESTINAL INFECTIONS DUE TO OTHER ORGANISMS -

Phenotypic and Genomic Analyses of Burkholderia Stabilis Clinical Contamination, Switzerland Helena M.B
RESEARCH Phenotypic and Genomic Analyses of Burkholderia stabilis Clinical Contamination, Switzerland Helena M.B. Seth-Smith, Carlo Casanova, Rami Sommerstein, Dominik M. Meinel,1 Mohamed M.H. Abdelbary,2 Dominique S. Blanc, Sara Droz, Urs Führer, Reto Lienhard, Claudia Lang, Olivier Dubuis, Matthias Schlegel, Andreas Widmer, Peter M. Keller,3 Jonas Marschall, Adrian Egli A recent hospital outbreak related to premoistened gloves pathogens that generally fall within the B. cepacia com- used to wash patients exposed the difficulties of defining plex (Bcc) (1). Burkholderia bacteria have large, flexible, Burkholderia species in clinical settings. The outbreak strain multi-replicon genomes, a large metabolic repertoire, vari- displayed key B. stabilis phenotypes, including the inabil- ous virulence factors, and inherent resistance to many anti- ity to grow at 42°C; we used whole-genome sequencing to microbial drugs (2,3). confirm the pathogen was B. stabilis. The outbreak strain An outbreak of B. stabilis was identified among hos- genome comprises 3 chromosomes and a plasmid, shar- ing an average nucleotide identity of 98.4% with B. stabilis pitalized patients across several cantons in Switzerland ATCC27515 BAA-67, but with 13% novel coding sequenc- during 2015–2016 (4). The bacterium caused bloodstream es. The genome lacks identifiable virulence factors and has infections, noninvasive infections, and wound contamina- no apparent increase in encoded antimicrobial drug resis- tions. The source of the infection was traced to contaminat- tance, few insertion sequences, and few pseudogenes, ed commercially available, premoistened washing gloves suggesting this outbreak was an opportunistic infection by used for bedridden patients. After hospitals discontinued an environmental strain not adapted to human pathogenic- use of these gloves, the outbreak resolved. -

WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/05 (2006.01) A61P 31/02 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/CA20 14/000 174 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 4 March 2014 (04.03.2014) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: ZW. 13/790,91 1 8 March 2013 (08.03.2013) US (84) Designated States (unless otherwise indicated, for every (71) Applicant: LABORATOIRE M2 [CA/CA]; 4005-A, rue kind of regional protection available): ARIPO (BW, GH, de la Garlock, Sherbrooke, Quebec J1L 1W9 (CA). GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (72) Inventors: LEMIRE, Gaetan; 6505, rue de la fougere, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, Sherbrooke, Quebec JIN 3W3 (CA). -

Article/25/5/18-0438-App1.Pdf)
RESEARCH LETTERS Pathology. 2011;43:58–63. http://dx.doi.org/10.1097/ variabilis ticks can transmit the causative agent of Rocky PAT.0b013e328340e431 Mountain spotted fever, and Ixodes scapularis ticks can 8. Rodriguez-Lozano J, Pérez-Llantada E, Agüero J, Rodríguez-Fernández A, Ruiz de Alegria C, Martinez-Martinez L, transmit the causative agents of Lyme disease, babesiosis, et al. Sternal wound infection caused by Gordonia bronchialis: and human granulocytic anaplasmosis (1). Although less identification by MALDI-TOF MS. JMM Case Rep. 2016;3: common in the region, A. maculatum ticks are dominant e005067. in specific habitats and can transmit the causative agent of Rickettsia parkeri rickettsiosis (1). Address for correspondence: Rene Choi, Department of Ophthalmology, Persons who have occupations that require them to be Casey Eye Institute, Oregon Health and Science University, 3375 SW outside on a regular basis might have a greater risk for ac- Terwilliger Blvd, Portland, OR 97239, USA; email: [email protected] quiring a tickborne disease (2). Although numerous stud- ies have been conducted regarding risks for tickborne dis- eases among forestry workers in Europe, few studies have been performed in the United States (2,3). The studies that have been conducted in the United States have focused on forestry workers in the northeastern region (2). However, because of variable phenology and densities of ticks, it is useful to evaluate tick activity and pathogen prevalence in Rickettsiales in Ticks various regions and ecosystems. Burn-tolerant and burn-dependent ecosystems, such as Removed from Outdoor pine (Pinus spp.) and mixed pine forests commonly found Workers, Southwest Georgia in the southeastern United States, have unique tick dynam- and Northwest Florida, USA ics compared with those of other habitats (4). -
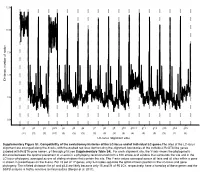
LC-Locus Alignment Sites Distance, Number of Nodes Supplementary
12.5 10.0 7.5 5.0 Distance, number of nodes 2.5 0.0 g1 g2 g3 g3.5 g4 g5 g6 g7 g8 g9 g10 g10.1 g11 g12 g13 g14 g15 (11) (3) (3) (10) (3) (3) (3) (3) (3) (3) (3) (4) (3) (3) (3) (2) (3) LC-locus alignment sites Supplementary Figure S1. Compatibility of the evolutionary histories of the LC-locus and of individual LC genes.The sites of the LC-locus alignment are arranged along the X-axis, with the dashed red lines demarcating the alignment boundaries of the individual RcGTA-like genes (labeled with RcGTA gene names, g1 through g15; see Supplementary Table S4). For each alignment site, the Y-axis shows the phylogenetic distance between the optimal placement of a taxon in a phylogeny reconstructed from a 100 amino-acid window that surrounds the site and in the LC-locus phylogeny, averaged across all sliding windows that contain the site. The Y-axis values averaged across all taxa and all sites within a gene is shown in parentheses on the X-axis. For 15 out of 17 genes, only 2-4 nodes separate the optimal taxon position in the LC-locus and gene phylogeny. The inflated distances for g1 and g3.5 are likely because only 15 and 21 of 95 LCs, respectively, have a homolog of these genes and the SSPB analysis is highly sensitive to missing data (Berger et al. 2011). a. Bacteria Unassigned Thermotogae Tenericutes Synergistetes Spirochaetes Proteobacteria ylum Planctomycetes h p Firmicutes Deferribacteres Cyanobacteria Chloroflexi Bacteroidetes Actinobacteria Acidobacteria 1(11,750) 2(1,750) 3(2,538) 4(168) 5(51) 6(54) 7(43) 8(32) 9(26) 10(40) 11(33) 12(198) 13(173) 14(101) 15(98) 16(43) 17(114) Number of rcc01682−rcc01698 homologs in a cluster b.