Mitochondrial Stress and Metabolic Dysfunction in the Liver: a Role for the Unfolded Protein
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Identification of the Binding Partners for Hspb2 and Cryab Reveals
Brigham Young University BYU ScholarsArchive Theses and Dissertations 2013-12-12 Identification of the Binding arP tners for HspB2 and CryAB Reveals Myofibril and Mitochondrial Protein Interactions and Non- Redundant Roles for Small Heat Shock Proteins Kelsey Murphey Langston Brigham Young University - Provo Follow this and additional works at: https://scholarsarchive.byu.edu/etd Part of the Microbiology Commons BYU ScholarsArchive Citation Langston, Kelsey Murphey, "Identification of the Binding Partners for HspB2 and CryAB Reveals Myofibril and Mitochondrial Protein Interactions and Non-Redundant Roles for Small Heat Shock Proteins" (2013). Theses and Dissertations. 3822. https://scholarsarchive.byu.edu/etd/3822 This Thesis is brought to you for free and open access by BYU ScholarsArchive. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of BYU ScholarsArchive. For more information, please contact [email protected], [email protected]. Identification of the Binding Partners for HspB2 and CryAB Reveals Myofibril and Mitochondrial Protein Interactions and Non-Redundant Roles for Small Heat Shock Proteins Kelsey Langston A thesis submitted to the faculty of Brigham Young University in partial fulfillment of the requirements for the degree of Master of Science Julianne H. Grose, Chair William R. McCleary Brian Poole Department of Microbiology and Molecular Biology Brigham Young University December 2013 Copyright © 2013 Kelsey Langston All Rights Reserved ABSTRACT Identification of the Binding Partners for HspB2 and CryAB Reveals Myofibril and Mitochondrial Protein Interactors and Non-Redundant Roles for Small Heat Shock Proteins Kelsey Langston Department of Microbiology and Molecular Biology, BYU Master of Science Small Heat Shock Proteins (sHSP) are molecular chaperones that play protective roles in cell survival and have been shown to possess chaperone activity. -

4-6 Weeks Old Female C57BL/6 Mice Obtained from Jackson Labs Were Used for Cell Isolation
Methods Mice: 4-6 weeks old female C57BL/6 mice obtained from Jackson labs were used for cell isolation. Female Foxp3-IRES-GFP reporter mice (1), backcrossed to B6/C57 background for 10 generations, were used for the isolation of naïve CD4 and naïve CD8 cells for the RNAseq experiments. The mice were housed in pathogen-free animal facility in the La Jolla Institute for Allergy and Immunology and were used according to protocols approved by the Institutional Animal Care and use Committee. Preparation of cells: Subsets of thymocytes were isolated by cell sorting as previously described (2), after cell surface staining using CD4 (GK1.5), CD8 (53-6.7), CD3ε (145- 2C11), CD24 (M1/69) (all from Biolegend). DP cells: CD4+CD8 int/hi; CD4 SP cells: CD4CD3 hi, CD24 int/lo; CD8 SP cells: CD8 int/hi CD4 CD3 hi, CD24 int/lo (Fig S2). Peripheral subsets were isolated after pooling spleen and lymph nodes. T cells were enriched by negative isolation using Dynabeads (Dynabeads untouched mouse T cells, 11413D, Invitrogen). After surface staining for CD4 (GK1.5), CD8 (53-6.7), CD62L (MEL-14), CD25 (PC61) and CD44 (IM7), naïve CD4+CD62L hiCD25-CD44lo and naïve CD8+CD62L hiCD25-CD44lo were obtained by sorting (BD FACS Aria). Additionally, for the RNAseq experiments, CD4 and CD8 naïve cells were isolated by sorting T cells from the Foxp3- IRES-GFP mice: CD4+CD62LhiCD25–CD44lo GFP(FOXP3)– and CD8+CD62LhiCD25– CD44lo GFP(FOXP3)– (antibodies were from Biolegend). In some cases, naïve CD4 cells were cultured in vitro under Th1 or Th2 polarizing conditions (3, 4). -

Mitochondrial Protein Quality Control Mechanisms
G C A T T A C G G C A T genes Review Mitochondrial Protein Quality Control Mechanisms Pooja Jadiya * and Dhanendra Tomar * Center for Translational Medicine, Lewis Katz School of Medicine, Temple University, Philadelphia, PA 19140, USA * Correspondence: [email protected] (P.J.); [email protected] (D.T.); Tel.: +1-215-707-9144 (D.T.) Received: 29 April 2020; Accepted: 15 May 2020; Published: 18 May 2020 Abstract: Mitochondria serve as a hub for many cellular processes, including bioenergetics, metabolism, cellular signaling, redox balance, calcium homeostasis, and cell death. The mitochondrial proteome includes over a thousand proteins, encoded by both the mitochondrial and nuclear genomes. The majority (~99%) of proteins are nuclear encoded that are synthesized in the cytosol and subsequently imported into the mitochondria. Within the mitochondria, polypeptides fold and assemble into their native functional form. Mitochondria health and integrity depend on correct protein import, folding, and regulated turnover termed as mitochondrial protein quality control (MPQC). Failure to maintain these processes can cause mitochondrial dysfunction that leads to various pathophysiological outcomes and the commencement of diseases. Here, we summarize the current knowledge about the role of different MPQC regulatory systems such as mitochondrial chaperones, proteases, the ubiquitin-proteasome system, mitochondrial unfolded protein response, mitophagy, and mitochondria-derived vesicles in the maintenance of mitochondrial proteome and health. The proper understanding of mitochondrial protein quality control mechanisms will provide relevant insights to treat multiple human diseases. Keywords: mitochondria; proteome; ubiquitin; proteasome; chaperones; protease; mitophagy; mitochondrial protein quality control; mitochondria-associated degradation; mitochondrial unfolded protein response 1. Introduction Mitochondria are double membrane, dynamic, and semiautonomous organelles which have several critical cellular functions. -

Download (PDF)
Table S1. Putative miR-322 target transcripts which is highly expressed in MGCs ________________________________________________________________________________ 0610037L13Rik, 1700037H04Rik, 2310061I04Rik, 2810006K23Rik, Abcc5, Abhd16a, Acbd3, Acox1, Acsbg1, Acsl4, Actr1a, Actr2, Adck5, Adh5, Adrbk1, Aff4, Agk, Ahcyl1, Akap11, Akap7, Akirin1, Alg3, Amfr, Ammecr1, Amotl2, Ankfy1, Ankhd1, Ankrd52, Ap2a1, Ap2b1, Ap3b1, Ap3d1, App, Arcn1, Arf3, Arfgap2, Arhgap12, Arhgap5, Arhgdia, Arhgef11, Arih1, Arl2, Arl3, Arl8b, Armcx6, Asap1, Asnsd1, Atf6, Atg13, Atg4b, Atp13a3, Atp5g1, Atp6v1a, Atxn2, Atxn7l3, Atxn7l3b, AW549877, B4galt1, B4galt7, Bace1, Bag5, Baiap2, Baz2a, BC037034, Bcl2l1, Bcl2l2, Bfar, Bmpr1a, Bptf, Brd2, Brd4, Brpf3, Btbd3, Btg2, Cab39, Cacna2d1, Calm1, Capns1, Caprin1, Capza2, Carm1, Caskin1, Cbfa2t3, Cbx5, Cbx6, Cc2d1b, Ccdc127, Ccdc6, Ccnd2, Ccnt2, Ccnyl1, Cd164, Cd2ap, Cdc25a, Cdc27, Cdc37l1, Cdc42se2, Cdca4, Cdipt, Cdk5rap3, Cdk8, Cdk9, Cdv3, Celf1, Cfl2, Chchd3, Chd6, Chmp1a, Chmp7, Chordc1, Chpf, Chpt1, Chst8, Chtf8, Cisd2, Clasrp, Clcn3, Clstn1, Cmpk1, Cnih2, Cnot1, Cnot2, Col4a3bp, Cope, Cops2, Cops7a, Cops7b, Copz1, Coq6, Cpd, Crebzf, Crim1, Crk, Crkl, Csde1, Cse1l, Ctnnb1, Cul4a, Cul4b, Cxx1a, Cxx1b, Cxx1c, D15Ertd621e, D2hgdh, Dcaf7, Dcbld2, Dcp1a, Dctn5, Ddost, Ddr1, Ddx39, Ddx3x, Ddx6, Dedd, Dhdds, Dhx16, Diap1, Dido1, Dlst, Dmtf1, Dnaja2, Dnajb14, Dnajb2, Dnajc1, Dnajc16, Dnajc25, Dph3, Dpm1, Dpp9, Dpy19l4, Dsel, Dtl, Dvl1, Dync1li2, Dynll2, Dynlt3, Dyrk1a, Dyrk1b, Ebna1bp2, Edc4, Eftud2, Egln2, Eif1a, Eif2b2, Eif2s1, -

Identification of Transcriptional Mechanisms Downstream of Nf1 Gene Defeciency in Malignant Peripheral Nerve Sheath Tumors Daochun Sun Wayne State University
Wayne State University DigitalCommons@WayneState Wayne State University Dissertations 1-1-2012 Identification of transcriptional mechanisms downstream of nf1 gene defeciency in malignant peripheral nerve sheath tumors Daochun Sun Wayne State University, Follow this and additional works at: http://digitalcommons.wayne.edu/oa_dissertations Recommended Citation Sun, Daochun, "Identification of transcriptional mechanisms downstream of nf1 gene defeciency in malignant peripheral nerve sheath tumors" (2012). Wayne State University Dissertations. Paper 558. This Open Access Dissertation is brought to you for free and open access by DigitalCommons@WayneState. It has been accepted for inclusion in Wayne State University Dissertations by an authorized administrator of DigitalCommons@WayneState. IDENTIFICATION OF TRANSCRIPTIONAL MECHANISMS DOWNSTREAM OF NF1 GENE DEFECIENCY IN MALIGNANT PERIPHERAL NERVE SHEATH TUMORS by DAOCHUN SUN DISSERTATION Submitted to the Graduate School of Wayne State University, Detroit, Michigan in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY 2012 MAJOR: MOLECULAR BIOLOGY AND GENETICS Approved by: _______________________________________ Advisor Date _______________________________________ _______________________________________ _______________________________________ © COPYRIGHT BY DAOCHUN SUN 2012 All Rights Reserved DEDICATION This work is dedicated to my parents and my wife Ze Zheng for their continuous support and understanding during the years of my education. I could not achieve my goal without them. ii ACKNOWLEDGMENTS I would like to express tremendous appreciation to my mentor, Dr. Michael Tainsky. His guidance and encouragement throughout this project made this dissertation come true. I would also like to thank my committee members, Dr. Raymond Mattingly and Dr. John Reiners Jr. for their sustained attention to this project during the monthly NF1 group meetings and committee meetings, Dr. -

The Proteasomal Deubiquitinating Enzyme PSMD14 Regulates Macroautophagy by Controlling Golgi-To-ER Retrograde Transport
Supplementary Materials The proteasomal deubiquitinating enzyme PSMD14 regulates macroautophagy by controlling Golgi-to-ER retrograde transport Bustamante HA., et al. Figure S1. siRNA sequences directed against human PSMD14 used for Validation Stage. Figure S2. Primer pairs sequences used for RT-qPCR. Figure S3. The PSMD14 DUB inhibitor CZM increases the Golgi apparatus area. Immunofluorescence microscopy analysis of the Golgi area in parental H4 cells treated for 4 h either with the vehicle (DMSO; Control) or CZM. The Golgi marker GM130 was used to determine the region of interest in each condition. Statistical significance was determined by Student's t-test. Bars represent the mean ± SEM (n =43 cells). ***P <0.001. Figure S4. CZM causes the accumulation of KDELR1-GFP at the Golgi apparatus. HeLa cells expressing KDELR1-GFP were either left untreated or treated with CZM for 30, 60 or 90 min. Cells were fixed and representative confocal images were acquired. Figure S5. Effect of CZM on proteasome activity. Parental H4 cells were treated either with the vehicle (DMSO; Control), CZM or MG132, for 90 min. Protein extracts were used to measure in vitro the Chymotrypsin-like peptidase activity of the proteasome. The enzymatic activity was quantified according to the cleavage of the fluorogenic substrate Suc-LLVY-AMC to AMC, and normalized to that of control cells. The statistical significance was determined by One-Way ANOVA, followed by Tukey’s test. Bars represent the mean ± SD of biological replicates (n=3). **P <0.01; n.s., not significant. Figure S6. Effect of CZM and MG132 on basal macroautophagy. (A) Immunofluorescence microscopy analysis of the subcellular localization of LC3 in parental H4 cells treated with either with the vehicle (DMSO; Control), CZM for 4 h or MG132 for 6 h. -

Comparative Analysis of the Ubiquitin-Proteasome System in Homo Sapiens and Saccharomyces Cerevisiae
Comparative Analysis of the Ubiquitin-proteasome system in Homo sapiens and Saccharomyces cerevisiae Inaugural-Dissertation zur Erlangung des Doktorgrades der Mathematisch-Naturwissenschaftlichen Fakultät der Universität zu Köln vorgelegt von Hartmut Scheel aus Rheinbach Köln, 2005 Berichterstatter: Prof. Dr. R. Jürgen Dohmen Prof. Dr. Thomas Langer Dr. Kay Hofmann Tag der mündlichen Prüfung: 18.07.2005 Zusammenfassung I Zusammenfassung Das Ubiquitin-Proteasom System (UPS) stellt den wichtigsten Abbauweg für intrazelluläre Proteine in eukaryotischen Zellen dar. Das abzubauende Protein wird zunächst über eine Enzym-Kaskade mit einer kovalent gebundenen Ubiquitinkette markiert. Anschließend wird das konjugierte Substrat vom Proteasom erkannt und proteolytisch gespalten. Ubiquitin besitzt eine Reihe von Homologen, die ebenfalls posttranslational an Proteine gekoppelt werden können, wie z.B. SUMO und NEDD8. Die hierbei verwendeten Aktivierungs- und Konjugations-Kaskaden sind vollständig analog zu der des Ubiquitin- Systems. Es ist charakteristisch für das UPS, daß sich die Vielzahl der daran beteiligten Proteine aus nur wenigen Proteinfamilien rekrutiert, die durch gemeinsame, funktionale Homologiedomänen gekennzeichnet sind. Einige dieser funktionalen Domänen sind auch in den Modifikations-Systemen der Ubiquitin-Homologen zu finden, jedoch verfügen diese Systeme zusätzlich über spezifische Domänentypen. Homologiedomänen lassen sich als mathematische Modelle in Form von Domänen- deskriptoren (Profile) beschreiben. Diese Deskriptoren können wiederum dazu verwendet werden, mit Hilfe geeigneter Verfahren eine gegebene Proteinsequenz auf das Vorliegen von entsprechenden Homologiedomänen zu untersuchen. Da die im UPS involvierten Homologie- domänen fast ausschließlich auf dieses System und seine Analoga beschränkt sind, können domänen-spezifische Profile zur Katalogisierung der UPS-relevanten Proteine einer Spezies verwendet werden. Auf dieser Basis können dann die entsprechenden UPS-Repertoires verschiedener Spezies miteinander verglichen werden. -

SUPPLEMENTARY MATERIAL Dictyostelium As Model for Studying
www.intjdevbiol.com SUPPLEMENTARY MATERIAL corresponding to: Dictyostelium as model for studying ubiquitination and deubiquitination BARBARA PERGOLIZZI1, SALVATORE BOZZARO1 and ENRICO BRACCO2 1Department of Clinical and Biological Sciences and 2Department of Oncology, University of Torino, AOU S. Luigi, Orbassano (TO), Italy Full Text for this paper is available at: https://doi.org/10.1387/ijdb.190260eb TABLE S1: Dictyostelium discoideum Ubiquitin and Ubiquitin like family members UBLs/Ub members ID SUMO DDB_G0286189 NEDD8 DDB_G0278711 ATG12 DDB_G0282929 ATG8a DDB_G0286191 UBLs ATG8b DDB_G0290491 UFM DDB_G0295709 URM DDB_G0283737 FAU DDB_G0273743 Ubl5 DDB_G0284205 UbqA DDB_G0282295 UbqD DDB_G0286907 UbqF DDB_G0289449 UbqG DDB_G0282369 UbqH DDB_G0279721 UbqI DDB_G0291928 Ubiquitin UbqJ DDB_G0269458 UbqK DDB_G0280585 UbqN DDB_G0292984 UbqO DDB_G0292908 UbqB DDB_G0280755 UbqC DDB_G0276765 TABLE S2: Dictyostelium discoideum E1 ubiqutin conjugation members E1 Ub/Ubl Activating enzyme ID DDB_G0293306 Ubq DDB_G0268496 DDB_G0279641 SUMO DDB_G0286919 DDB_G0283891 NEDD8 DDB_G0287965 ATG8 DDB_G0271096 ATG12 DDB_G0271096 URM DDB_G0267980 FAT10 DDB_G0277047 ISG15 DDB_G0270272 UFM DDB_G0293306 FAU N.A. Ubl5 N.A. TABLE S3: Dictyostelium discoideum members of DUB family DUBs members D.d. gene ID H.s. gene orthologs name DDB_G0268872 N.A. USP49, USP44 DDB_G0284381 N.A. USP11, USP4, USP15 DDB_G0291239 ubpA USP5, USP13 DDB_G0276443 N.A. USP7 DDB_G0275021 ubpB USP10 DDB_G0290453 usp12 USP12 DDB_G0271264 N.A. USP14 DDB_G0293770 N.A. USP11, USP4, USP15 DDB_G0274207 N.A. USP45, USP16 DDB_G0271798 N.A. USP51 DDB_G0275415 N.A. N.A. USP DDB_G0271348 N.A. USP38 similar to H. sapiens DDB_G0270416 N.A. USP37 and USP26 DDB_G0278929 N.A. USP39 DDB_G0289611 N.A. USP40 DDB_G0274827 N.A. USP42, USP36 DDB_G0274795 N.A. USP48 Cys- DDB_G0292290 N.A. SENP1 dependent DDB_G0278795 senp8 SENP8 proteases DDB_G0293508 N.A. -
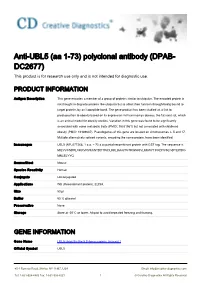
Anti-UBL5 (Aa 1-73) Polyclonal Antibody (DPAB- DC2677) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-UBL5 (aa 1-73) polyclonal antibody (DPAB- DC2677) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Antigen Description This gene encodes a member of a group of proteins similar to ubiquitin. The encoded protein is not thought to degrade proteins like ubiquitin but to affect their function through being bound to target proteins by an isopeptide bond. The gene product has been studied as a link to predisposition to obesity based on its expression in Psammomys obesus, the fat sand rat, which is an animal model for obesity studies. Variation in this gene was found to be significantly associated with some metabolic traits (PMID: 15331561) but not associated with childhood obesity (PMID: 19189687). Pseudogenes of this gene are located on chromosomes 3, 5 and 17. Multiple alternatively spliced variants, encoding the same protein, have been identified. Immunogen UBL5 (NP_077268, 1 a.a. ~ 73 a.a) partial recombinant protein with GST tag. The sequence is MIEVVCNDRLGKKVRVKCNTDDTIGDLKKLIAAQTGTRWNKIVLKKWYTIFKDHVSLGDYEIHDG MNLELYYQ Source/Host Mouse Species Reactivity Human Conjugate Unconjugated Applications WB (Recombinant protein), ELISA, Size 50 μl Buffer 50 % glycerol Preservative None Storage Store at -20°C or lower. Aliquot to avoid repeated freezing and thawing. GENE INFORMATION Gene Name UBL5 ubiquitin-like 5 [ Homo sapiens (human) ] Official Symbol UBL5 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved Synonyms UBL5; ubiquitin-like 5; HUB1; ubiquitin-like protein 5; beacon; Entrez Gene ID 59286 Protein Refseq NP_001041706 UniProt ID A0A024R7B0 Chromosome Location 19p13.3 Function molecular_function; protein binding; 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 2 © Creative Diagnostics All Rights Reserved. -

Spatial Sorting Enables Comprehensive Characterization of Liver Zonation
ARTICLES https://doi.org/10.1038/s42255-019-0109-9 Spatial sorting enables comprehensive characterization of liver zonation Shani Ben-Moshe1,3, Yonatan Shapira1,3, Andreas E. Moor 1,2, Rita Manco1, Tamar Veg1, Keren Bahar Halpern1 and Shalev Itzkovitz 1* The mammalian liver is composed of repeating hexagonal units termed lobules. Spatially resolved single-cell transcriptomics has revealed that about half of hepatocyte genes are differentially expressed across the lobule, yet technical limitations have impeded reconstructing similar global spatial maps of other hepatocyte features. Here, we show how zonated surface markers can be used to sort hepatocytes from defined lobule zones with high spatial resolution. We apply transcriptomics, microRNA (miRNA) array measurements and mass spectrometry proteomics to reconstruct spatial atlases of multiple zon- ated features. We demonstrate that protein zonation largely overlaps with messenger RNA zonation, with the periportal HNF4α as an exception. We identify zonation of miRNAs, such as miR-122, and inverse zonation of miRNAs and their hepa- tocyte target genes, highlighting potential regulation of gene expression levels through zonated mRNA degradation. Among the targets, we find the pericentral Wingless-related integration site (Wnt) receptors Fzd7 and Fzd8 and the periportal Wnt inhibitors Tcf7l1 and Ctnnbip1. Our approach facilitates reconstructing spatial atlases of multiple cellular features in the liver and other structured tissues. he mammalian liver is a structured organ, consisting of measurements would broaden our understanding of the regulation repeating hexagonally shaped units termed ‘lobules’ (Fig. 1a). of liver zonation and could be used to model liver metabolic func- In mice, each lobule consists of around 9–12 concentric lay- tion more precisely. -

SARS-Cov-2 Desensitizes Host Cells to Interferon Through Inhibition of the JAK-STAT Pathway
bioRxiv preprint doi: https://doi.org/10.1101/2020.10.27.358259; this version posted October 28, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. SARS-CoV-2 desensitizes host cells to interferon through inhibition of the JAK- STAT pathway Da-Yuan Chen1,2, Nazimuddin Khan1,2*, Brianna J. Close1,3*, Raghuveera K. Goel4, Benjamin Blum4, Alexander H. Tavares1,2, Devin Kenney2,3, Hasahn L. Conway1,2, Jourdan K. Ewoldt5,6,7, Sebastian Kapell1,2, Vipul C. Chitalia8,9,10, Nicholas A. Crossland2,11, Christopher S. Chen5,6,7, Darrell N. Kotton12,13, Susan C. Baker14, John H. Connor1,2, Florian Douam2,3, Andrew Emili4, Mohsan Saeed1,2# 1. Department of Biochemistry, Boston University School of Medicine, Boston, MA, USA 2. National Emerging Infectious Diseases Laboratories, Boston University, Boston, MA, USA 3. Department of Microbiology, Boston University School of Medicine, Boston, MA, USA 4. Center for Network Systems Biology, Boston University, Boston, MA, USA 5. Department of Biomedical Engineering, Boston University, Boston, MA, USA 6. Biological Design Center, Boston University, Boston, MA, USA 7. Wyss Institute for Biologically Inspired Engineering, Harvard University, Boston, MA, USA 8. Renal Section, Department of Medicine, Boston University School of Medicine, Boston, MA, USA 9. Boston Veterans Affairs Healthcare System, Boston, MA, USA bioRxiv preprint doi: https://doi.org/10.1101/2020.10.27.358259; this version posted October 28, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. -

A High-Throughput Study in Melanoma Identifies Epithelial- Mesenchymal Transition As a Major Determinant of Metastasis
Research Article A High-Throughput Study in Melanoma Identifies Epithelial- Mesenchymal Transition as a Major Determinant of Metastasis Soledad R. Alonso,1 Lorraine Tracey,1 Pablo Ortiz,4 Beatriz Pe´rez-Go´mez,5 Jose´ Palacios,1 Marina Polla´n,5 Juan Linares,6 Salvio Serrano,7 Ana I. Sa´ez-Castillo,6 Lydia Sa´nchez,2 Raquel Pajares,2 Abel Sa´nchez-Aguilera,1 Maria J. Artiga,1 Miguel A. Piris,1 and Jose´ L. Rodrı´guez-Peralto3 1Molecular Pathology Programme and 2Histology and Immunohistochemistry Unit, Centro Nacional de Investigaciones Oncolo´gicas; Departments of 3Pathology and 4Dermatology, Hospital Universitario 12 de Octubre; 5Centro Nacional de Epidemiologı´a, Instituto de Salud Carlos III, Madrid, Spain; and Departments of 6Pathology and 7Dermatology, Hospital Universitario San Cecilio, Granada, Spain Abstract with a less favorable prognosis as potential candidates for adjuvant Metastatic disease is the primary cause of death in cutaneous or novel therapies. malignant melanoma (CMM) patients. To understand the Currently, the prognosis of primary CMM is mainly based mechanisms of CMM metastasis and identify potential on histopathologic criteria. The most important of these is the predictive markers, we analyzed gene-expression profiles of Breslow index, although it is merely a measure of tumor depth. 34 vertical growth phase melanoma cases using cDNA micro- New molecular markers that correlate with melanoma genesis and/or progression are continuously being identified but, to date, arrays. All patients had a minimum follow-up of 36 months. Twenty-one cases developed nodal metastatic disease and 13 most of them have been obtained in experimental models and did not.