Overexpression of Epidermal Growth Factor and Hepatocyte Growth Factor Receptors in a Proportion of Gastrinomas Correlates with Aggressive Growth and Lower Curability
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Adrenal Cancer Causes, Risk Factors, and Prevention Adrenal
cancer.org | 1.800.227.2345 Adrenal Cancer Causes, Risk Factors, and Prevention Risk Factors A risk factor is anything that affects your chance of getting a disease such as cancer. Learn more about the risk factors for adrenal cancer. ● Adrenal Cancer Risk Factors ● What Causes Adrenal Cancer? Prevention Since there are no known preventable risk factors for this cancer, it is not possible to prevent this disease. Adrenal Cancer Risk Factors A risk factor is anything that changes your chance of getting a disease such as cancer. Different cancers have different risk factors. Some risk factors, like smoking, can be changed. Others, like a person’s age or family history, can’t be changed. Scientists have found few risk factors that make a person more likely to develop adrenal cancer. Even if a patient does have one or more risk factors for adrenal cancer, it is impossible to know for sure how much that risk factor contributed to causing the cancer. 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 But having a risk factor, or even several, does not mean that you will get the disease. Many people with risk factors never develop adrenal cancer, while others with this disease may have few or no known risk factors. Genetic syndromes The majority of adrenal cortex cancers are not inherited (sporadic), but some (up to 15%) are caused by a genetic defect. This is more common in adrenal cancers in children. Li-Fraumeni syndrome The Li-Fraumeni syndrome is a rare condition that is most often caused by a defect in the TP53 gene. -
Endocrine Pathology (537-577)
LABORATORY INVESTIGATION THE BASIC AND TRANSLATIONAL PATHOLOGY RESEARCH JOURNAL LI VOLUME 99 | SUPPLEMENT 1 | MARCH 2019 2019 ABSTRACTS ENDOCRINE PATHOLOGY (537-577) MARCH 16-21, 2019 PLATF OR M & 2 01 9 ABSTRACTS P OSTER PRESENTATI ONS EDUCATI ON C O M MITTEE Jason L. Hornick , C h air Ja mes R. Cook R h o n d a K. Y a nti s s, Chair, Abstract Revie w Board S ar a h M. Dr y and Assign ment Co m mittee Willi a m C. F a q ui n Laura W. La mps , Chair, C ME Subco m mittee C ar ol F. F ar v er St e v e n D. Billi n g s , Interactive Microscopy Subco m mittee Y uri F e d ori w Shree G. Shar ma , Infor matics Subco m mittee Meera R. Ha meed R aj a R. S e et h al a , Short Course Coordinator Mi c h ell e S. Hir s c h Il a n W ei nr e b , Subco m mittee for Unique Live Course Offerings Laksh mi Priya Kunju D a vi d B. K a mi n s k y ( Ex- Of ici o) A n n a M ari e M ulli g a n Aleodor ( Doru) Andea Ri s h P ai Zubair Baloch Vi nita Parkas h Olca Bast urk A nil P ar w a ni Gregory R. Bean , Pat h ol o gist-i n- Trai ni n g D e e p a P atil D a ni el J. -
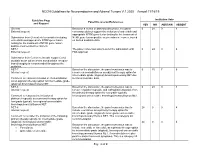
NCCN Guidelines for Neuroendocrine and Adrenal Tumors V.1.2020 – Annual 11/18/19
NCCN Guidelines for Neuroendocrine and Adrenal Tumors V.1.2020 – Annual 11/18/19 Guideline Page Institution Vote Panel Discussion/References and Request YES NO ABSTAIN ABSENT General Based on a review of data and discussion, the panel 0 24 0 4 External request: consensus did not support the inclusion of entrectinib and appropriate NTRK gene fusion testing for the treatment of Submission from Genentech to consider including NTRK gene fusion-positive neuroendocrine cancer, based entrectinib and appropriate NTRK gene fusion on limited available data. testing for the treatment of NTRK gene fusion- positive neuroendocrine cancers. NET-1 The panel consensus was to defer the submission until 0 24 0 4 External request: FDA approval. Submission from Curium to include copper Cu 64 dotatate as an option where somatostatin receptor- based imaging is recommended throughout the guideline. NET-7 Based on the discussion, the panel consensus was to 0 15 7 6 Internal request: remove chemoradiation as an adjuvant therapy option for intermediate grade (atypical) bronchopulmonary NET due Comment to reassess inclusion of chemoradiation to limited available data. as an adjuvant therapy option for intermediate grade (atypical) bronchopulmonary NET. NET-8 Based on the discussion, the panel consensus was to 0 24 0 4 Internal request: remove cisplatin/etoposide and carboplatin/etoposide from the primary therapy option for low grade (typical), Comment to reassess the inclusion of locoregional unresectable bronchopulmonary/thymus NET. platinum/etoposide as a primary therapy option for low grade (typical), locoregional unresectable bronchopulmonary/thymus NET. NET-8 Based on the discussion, the panel consensus was to 24 0 0 4 Internal request: include everolimus as a primary therapy option for intermediate grade (atypical), locoregional unresectable Comment to consider the inclusion of the following bronchopulmonary/thymus NET. -

Neoplastic Metastases to the Endocrine Glands
27 1 Endocrine-Related A Angelousi et al. Metastases to endocrine 27:1 R1–R20 Cancer organs REVIEW Neoplastic metastases to the endocrine glands Anna Angelousi1, Krystallenia I Alexandraki2, George Kyriakopoulos3, Marina Tsoli2, Dimitrios Thomas2, Gregory Kaltsas2 and Ashley Grossman4,5,6 1Endocrine Unit, 1st Department of Internal Medicine, Laiko Hospital, National and Kapodistrian University of Athens, Athens, Greece 2Endocrine Unit, 1st Department of Propaedeutic Medicine, Laiko University Hospital, Medical School, National and Kapodistrian University of Athens, Athens, Greece 3Department of Pathology, General Hospital ‘Evangelismos’, Αthens, Greece 4Department of Endocrinology, OCDEM, University of Oxford, Oxford, UK 5Neuroendocrine Tumour Unit, Royal Free Hospital, London, UK 6Centre for Endocrinology, Barts and the London School of Medicine, Queen Mary University of London, London, UK Correspondence should be addressed to A Angelousi: [email protected] Abstract Endocrine organs are metastatic targets for several primary cancers, either through Key Words direct extension from nearby tumour cells or dissemination via the venous, arterial and f glands lymphatic routes. Although any endocrine tissue can be affected, most clinically relevant f cancer metastases involve the pituitary and adrenal glands with the commonest manifestations f metastases being diabetes insipidus and adrenal insufficiency respectively. The most common f pituitary primary tumours metastasing to the adrenals include melanomas, breast and lung f adrenal carcinomas, which may lead to adrenal insufficiency in the presence of bilateral adrenal f thyroid involvement. Breast and lung cancers are the most common primaries metastasing to f ovaries the pituitary, leading to pituitary dysfunction in approximately 30% of cases. The thyroid gland can be affected by renal, colorectal, lung and breast carcinomas, and melanomas, but has rarely been associated with thyroid dysfunction. -

A Case of Postpartum Hypopituitarism Accompanied by Cushing's
Endocrine Journal 2005, 52 (2), 219–222 A Case of Postpartum Hypopituitarism Accompanied by Cushing’s Syndrome as a Result of an Adrenocortical Carcinoma MEHMET SENCAN AND HATICE SEBILA DOKMETAS* Department of Hematology, Faculty of Medicine, Cumhuriyet University, 58140 Sivas, Turkey *Department of Endocrinology, Faculty of Medicine, Cumhuriyet University, 58140 Sivas, Turkey Abstract. Sheehan’s syndrome frequently causes hypopituitarism either immediately or after a delay of several years, depending on the degrees of postpartum ischemic pituitary necrosis. A 55 year-old woman whose last child was born 27 yr ago with massive hemorrhage was diagnosed as postpartum hypopituitarism. She had deficiency of growth hormone, prolactin, gonadotropins and thyrotropin. However, she interestingly had apparent hypercortisolism without suppression response to the dexamethasone tests. We found an adrenal mass with distant metastases to the liver and lung while investigating the origin of the hypercortisolism. Hyperandrogenism and very high levels of 17 hydroxyprogesterone were present. Accordingly, the patient was diagnosed as hypopituitarism due to Sheehan’s syndrome accompanied by Cushing’s syndrome as a result of an adrenocortical carcinoma. Key words: Sheehan’s syndrome, Hypopituitarism, Hypercortisolism, Adrenocortical carcinoma (Endocrine Journal 52: 219–222, 2005) SHEEHAN’S syndrome occurs as a result of ischemic with adrenocortical carcinoma may show different pituitary necrosis due to severe postpartum hemor- endocrine syndromes depending on the secretion of rhage and is characterized by various degrees of tumor; hypercortisolism and hyperandrogenism are hypopituitarism [1, 2]. Sheehan’s syndrome is a rare the most prevalent [4, 5]. postpartum complication of pregnancy with better In this report, a case with hypopituitarism due to obstetric care in developed countries. -

Adrenal Cortical Tumors, Pheochromocytomas and Paragangliomas
Modern Pathology (2011) 24, S58–S65 S58 & 2011 USCAP, Inc. All rights reserved 0893-3952/11 $32.00 Adrenal cortical tumors, pheochromocytomas and paragangliomas Ricardo V Lloyd Department of Pathology, University of Wisconsin School of Medicine and Public Health, Madison, WI, USA Distinguishing adrenal cortical adenomas from carcinomas may be a difficult diagnostic problem. The criteria of Weiss are very useful because of their reliance on histologic features. From a practical perspective, the most useful criteria to separate adenomas from carcinomas include tumor size, presence of necrosis and mitotic activity including atypical mitoses. Adrenal cortical neoplasms in pediatric patients are more difficult to diagnose and to separate adenomas from carcinomas. The diagnosis of pediatric adrenal cortical carcinoma requires a higher tumor weight, larger tumor size and more mitoses compared with carcinomas in adults. Pheochromocytomas are chromaffin-derived tumors that develop in the adrenal gland. Paragangliomas are tumors arising from paraganglia that are distributed along the parasympathetic nerves and sympathetic chain. Positive staining for chromogranin and synaptophysin is present in the chief cells, whereas the sustentacular cells are positive for S100 protein. Hereditary conditions associated with pheochromocytomas include multiple endocrine neoplasia 2A and 2B, Von Hippel–Lindau disease and neurofibromatosis I. Hereditary paraganglioma syndromes with mutations of SDHB, SDHC and SDHD are associated with paragangliomas and some pheochromocytomas. -
Epigenetic Alterations in Endocrine- Related Cancer
S Rodrı´guez-Rodero et al. Epigenetics and endocrine 21:4 R319–R330 Review cancer Epigenetic alterations in endocrine- related cancer Sandra Rodrı´guez-Rodero1,2, Elı´as Delgado-A´ lvarez1, Agustı´n F Ferna´ndez2, Juan L Ferna´ndez-Morera1, Edelmiro Mene´ndez-Torre1 and Mario F Fraga2,3 Correspondence 1Endocrinology and Nutrition Service, Hospital Universitario Central de Asturias, Av. Julian Claverı´a s/n, should be addressed 33006 Oviedo, Spain to E Mene´ ndez-Torre or 2Cancer Epigenetics Laboratory, Instituto Universitario de Oncologı´a del Principado de Asturias (IUOPA), M F Fraga Universidad de Oviedo, 33006 Oviedo, Spain Emails 3Department of Immunology and Oncology, National Center for Biotechnology, CNB-CSIC, Cantoblanco, [email protected] or Madrid E-28049, Spain [email protected] Abstract Aberrant epigenetics is a hallmark of cancer, and endocrine-related tumors are no exception. Key Words Recent research has been identifying an ever-growing number of epigenetic alterations in " multiple endocrine both genomic DNA methylation and histone post-translational modification in tumors of the neoplasias endocrine system. Novel microarray and ultra-deep sequencing technologies have allowed " neuroendocrine tumors the identification of genome-wide epigenetic patterns in some tumor types such as " oncology adrenocortical, parathyroid, and breast carcinomas. However, in other cancer types, such " pathogenesis as the multiple endocrine neoplasia syndromes and thyroid cancer, tumor information is limited to candidate genes alone. Future research should fill this gap and deepen our understanding of the functional role of these alterations in cancer, as well as defining Endocrine-Related Cancer their possible clinical uses. Endocrine-Related Cancer (2014) 21, R319–R330 Introduction Epigeneticsisdefinedasthestudyofthosestable However, all such mechanisms in fact cooperate with each genetic modifications that result in changes in function other, and also with other levels of regulation, to establish and gene expression without altering the DNA sequence. -

Feminizing Adrenocortical Carcinoma with Distant
Clinics and Practice 2014; volume 4:651 Feminizing adrenocortical (either virilization or feminization), although mixed clinical features can be observed.1,5 Correspondence: Alessandro Fancellu, Unit of carcinoma with distant Feminizing ACCs, i.e. malignant adrenal General Surgery 2 - Clinica Chirurgica, metastases: can surgery tumors causing features of estrogen excess, Department of Clinical and Experimental be considered? are an extremely rare cause of abdominal Medicine, University of Sassari, v.le San Pietro mass. 43, 07100 Sassari, Italy. Tel.: +39.079.228432 - Fax: +39.079 228394. Alessandro Fancellu, Antonio Pinna, We herein present a case of a young man E-mail: [email protected] Alberto Porcu having a giant feminizing ACC with distant metastases, which posed serious management Key words: adrenocortical carcinoma, feminizing, Unit of General Surgery 2, Department problems principally related to the burden of treatment, gynecomastia, rare tumor. of Clinical and Experimental Medicine, the primary tumor. University of Sassari, Italy Conflicts of interest: the authors declare no potential conflicts of interest. Case Report Contributions: the authors contributed equally. Abstract Received for publication: 9 May 2014. A 41-year-old gentleman presented com- Accepted for publication: 12 June 2014. plaining of a 6-month history of bilateral Functioning adrenocortical carcinomas are gynecomastia without galactorrhea, and a sig- This work is licensed under a Creative Commons rare diseases with dismal prognosis. A 41-year- Attribution NonCommercial 3.0 License (CC BY- nificant weight loss (8 kg in the last three old man presenting with gynecomastia had a NC 3.0). months). In the last two months he also giant feminizing adrenocortical carcinoma at noticed abdominal and back pain, dyspepsia, stage IV. -

Thyroid and Adrenal Gland NAACCR 2011‐2012 Webinar Series 12/1/11
11/28/2011 Thyroid and Adrenal Gland NAACCR 2011‐2012 Webinar Series 12/1/11 Q&A • Please submit all questions concerning webinar content through the Q&A panel. Reminder: • If you have participants watching this webinar at your site, please collect their names and emails. – We will be distributing a Q&A document in about one week. This document will fully answer questions asked during the webinar and will contain any corrections that we may discover after the webinar. 2 Fabulous Prizes 3 1 11/28/2011 Agenda • Coding moment – Submitting questions to the standard setters • Thyroid – Overview – Collaborative Stage Data Collection System (CS) – Quiz – Exercise • Adrenal Gland – Overview – CS – Quiz – Exercise Coding Moment SUBMITTING QUESTIONS TO STANDARD SETTERS Who do I submit questions to? • That depends on the question! 2 11/28/2011 Questions for SEER • Questions concerning the following topics should go to Ask a SEER Registrar http://seer.cancer.gov/registrars/contact.html – Multiple primary rules – ICD‐0‐3 – ICD‐10 Question for CAnswer Forum • Questions concerning the following topics should go to the CAnswer Forum http://cancerbulletin.facs.org/forums/content.php – AJCC TNM Staging – Collaborative Stage Submitting Questions to SEER 1. Search the SEER Inquiry System – http://seer.cancer.gov/seerinquiry/index.php?page= search 2. If you don’t find an answer to your question, submit your question to Ask A SEER Registrar – http://seer.cancer.gov/registrars/contact.html 3 11/28/2011 4 11/28/2011 5 11/28/2011 Submitting Questions to the CAnswer -

From Benign Adrenal Incidentaloma to Adrenocortical Carcinoma: an Exceptional Random Event
176:6 AUTHOR COPY ONLY I Belmihoub and others From adrenal adenoma to ACC 176:6 K15–K19 Case Report From benign adrenal incidentaloma to adrenocortical carcinoma: an exceptional random event I Belmihoub1, S Silvera2, M Sibony3, B Dousset4, P Legmann5, X Bertagna1, J Bertherat1,6 and G Assié1,6 1Department of Endocrinology, Center for Rare Adrenal Diseases, Hôpital Cochin, Assistance Publique Hôpitaux de Paris, Paris, France, 2Department of Radiology, Saint Joseph Hospital, Paris, France, Departments of 3Pathology, Correspondence 4Digestive and Endocrine Surgery and 5Radiology A, Hôpital Cochin, Assistance Publique Hôpitaux de Paris, Paris, should be addressed France, and 6Institut Cochin, Institut National de la Santé et de la Recherche Médicale U1016, Centre National de la to G Assié Recherche Scientifique UMR8104, Université Paris Descartes, Sorbonne Paris Cité, Paris, France Email [email protected] Abstract New European guidelines for the management of adrenal incidentalomas were recently released. One of the most novel recommendations is to stop following patients when they present a typical, small and non-secreting adenoma. We report here the case of a 71-year-old man with such an adenoma, who developed an adrenocortical carcinoma (ACC) fourteen years later, with subsequent metastases and death. Clinically, he had a normal blood pressure and no sign of hormonal hypersecretion. The hormonal work-up showed no hormone excess: urinary free cortisol level was normal, the diurnal cortisol rhythm was respected and urinary catecholamine metabolites levels were normal. Computed tomography (CT) scan showed a homogeneous lesion, with a low density. The lesion remained unchanged during the five years of follow-up. -

Endocrine Oncology: Special Issue
Metab y & o OPEN ACCESS Freely available online g lic lo S o y n n i r d c r o o Endocrinology & Metabolic Syndrome m d n e E ISSN: 2161-1017 Editorial Endocrine Oncology: Special Issue Ilene Fennoy* Department of Pediatrics, Division of Pediatric Diabetes, Endocrinology and Metabolism, Columbia University, New York, New York, USA About Special Issue • Small cell lung cancer Endocrinology & Metabolic Syndrome is an Open Access journal Endocrine pancreatic Tumors with rapid peer-reviewed publishes in the field like biosynthesis, Types of Endocrine pancreatic Tumorsare listed below storage, chemistry, and physiological function of hormones and the cells of endocrine glands and tissues that secrete them. • Non-functioning endocrine pancreatic tumors Endocrinology is happy to announce its Special Issue on “Endocrine • Insulinoma Oncology”. Endocrinology is offering special discounts on APC • Gastrinoma (Article Processing Charges) and immediate publication (within 21days from initial date of submission). Our Journal is planning to • Glucagonoma release issue by end of the Year i.e., Dec 30th, 2020. • VIPoma Endocrine oncologyis a medical specialty deals with the production Adrenals Tumors of hormones and tumors. There are several kinds of endocrine tumors, and are listed below Types of Adrenals Tumorsare listed below • Thyroid Cancer • Adrenocortical carcinoma • Parathyroid Tumors • Pheochromocytoma • Adrenocortical Carcinoma Syndromes of Endocrine Tumor • Pheochromocytoma Types of Syndromes of Endocrine Tumor are listed below • Neuroendocrine Tumors • Multiple Endocrine Neoplasia I, MEN1 • Pituitary Tumors • Multiple Endocrine Neoplasia II, MEN2 Gastrointestinal Tumors • von HippelLindau syndrome Types of gastrointestinal tumours are listed as below We are proud and glad to announce that our journal is ready to release volume 9Issue 7 in this year 2020 and the last issue of this • ECLoma year. -

Tumors of the Adrenal Glands – Genetic and Diagnostic Aspects
From the Department of Oncology-Pathology Karolinska Institutet, Stockholm, Sweden TUMORS OF THE ADRENAL GLANDS – GENETIC AND DIAGNOSTIC ASPECTS Fredrika Svahn Stockholm 2021 All previously published papers were reproduced with permission from the publisher. Published by Karolinska Institutet. Printed by Universitetsservice US-AB, Stockholm 2020 © Fredrika Svahn, 2021 ISBN 978-91-8016-064-3 Tumors of the adrenal glands – Genetic and Diagnostic aspects THESIS FOR DOCTORAL DEGREE (Ph.D.) The public defense of the dissertation will be held at the Lecture Hall in CCK floor 00, R8:00 Karolinska University Hospital Solna January 15th 2021 at 13:00 By Fredrika Svahn Principal Supervisor: Opponent: Catharina Larsson, Professor Erik Nordenström, Associate Professor Karolinska Institutet Lund University Department of Oncology-Pathology Department of Clinical Sciences Co-supervisors: Examination Board: Carl Christofer Juhlin, Associate Professor Bertha Brodin, Associate Professor Karolinska Institutet KTH Royal Institute of Technology Department of Oncology-Pathology Department of Applied Physics Karolinska Institutet Martin Bäckdahl, Professor Department of Microbiology, Tumor and Cell Karolinska Institutet Biology Department of Molecular Medicine and Surgery Anders Näsman, Associate Professor Karolinska Institutet Adam Stenman, Ph.D. Department of Oncology-Pathology Karolinska Institutet Department of Molecular Medicine and Bo Wängberg, Professor Surgery University of Gothenburg Institute of Clinical Sciences External mentor: Anders Öwall, Associate