Endocrine Pathology (537-577)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Endo4 PRINT.Indb
Contents 1 Tumours of the pituitary gland 11 Spindle epithelial tumour with thymus-like differentiation 123 WHO classifi cation of tumours of the pituitary 12 Intrathyroid thymic carcinoma 125 Introduction 13 Paraganglioma and mesenchymal / stromal tumours 127 Pituitary adenoma 14 Paraganglioma 127 Somatotroph adenoma 19 Peripheral nerve sheath tumours 128 Lactotroph adenoma 24 Benign vascular tumours 129 Thyrotroph adenoma 28 Angiosarcoma 129 Corticotroph adenoma 30 Smooth muscle tumours 132 Gonadotroph adenoma 34 Solitary fi brous tumour 133 Null cell adenoma 37 Haematolymphoid tumours 135 Plurihormonal and double adenomas 39 Langerhans cell histiocytosis 135 Pituitary carcinoma 41 Rosai–Dorfman disease 136 Pituitary blastoma 45 Follicular dendritic cell sarcoma 136 Craniopharyngioma 46 Primary thyroid lymphoma 137 Neuronal and paraneuronal tumours 48 Germ cell tumours 139 Gangliocytoma and mixed gangliocytoma–adenoma 48 Secondary tumours 142 Neurocytoma 49 Paraganglioma 50 3 Tumours of the parathyroid glands 145 Neuroblastoma 51 WHO classifi cation of tumours of the parathyroid glands 146 Tumours of the posterior pituitary 52 TNM staging of tumours of the parathyroid glands 146 Mesenchymal and stromal tumours 55 Parathyroid carcinoma 147 Meningioma 55 Parathyroid adenoma 153 Schwannoma 56 Secondary, mesenchymal and other tumours 159 Chordoma 57 Haemangiopericytoma / Solitary fi brous tumour 58 4 Tumours of the adrenal cortex 161 Haematolymphoid tumours 60 WHO classifi cation of tumours of the adrenal cortex 162 Germ cell tumours 61 TNM classifi -

Adrenal Cancer Causes, Risk Factors, and Prevention Adrenal
cancer.org | 1.800.227.2345 Adrenal Cancer Causes, Risk Factors, and Prevention Risk Factors A risk factor is anything that affects your chance of getting a disease such as cancer. Learn more about the risk factors for adrenal cancer. ● Adrenal Cancer Risk Factors ● What Causes Adrenal Cancer? Prevention Since there are no known preventable risk factors for this cancer, it is not possible to prevent this disease. Adrenal Cancer Risk Factors A risk factor is anything that changes your chance of getting a disease such as cancer. Different cancers have different risk factors. Some risk factors, like smoking, can be changed. Others, like a person’s age or family history, can’t be changed. Scientists have found few risk factors that make a person more likely to develop adrenal cancer. Even if a patient does have one or more risk factors for adrenal cancer, it is impossible to know for sure how much that risk factor contributed to causing the cancer. 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 But having a risk factor, or even several, does not mean that you will get the disease. Many people with risk factors never develop adrenal cancer, while others with this disease may have few or no known risk factors. Genetic syndromes The majority of adrenal cortex cancers are not inherited (sporadic), but some (up to 15%) are caused by a genetic defect. This is more common in adrenal cancers in children. Li-Fraumeni syndrome The Li-Fraumeni syndrome is a rare condition that is most often caused by a defect in the TP53 gene. -

Adrenal Neuroblastoma Mimicking Pheochromocytoma in an Adult With
Khalayleh et al. Int Arch Endocrinol Clin Res 2017, 3:008 Volume 3 | Issue 1 International Archives of Endocrinology Clinical Research Case Report : Open Access Adrenal Neuroblastoma Mimicking Pheochromocytoma in an Adult with Neurofibromatosis Type 1 Harbi Khalayleh1, Hilla Knobler2, Vitaly Medvedovsky2, Edit Feldberg3, Judith Diment3, Lena Pinkas4, Guennadi Kouniavsky1 and Taiba Zornitzki2* 1Department of Surgery, Hebrew University Medical School of Jerusalem, Israel 2Endocrinology, Diabetes and Metabolism Institute, Kaplan Medical Center, Hebrew University Medical School of Jerusalem, Israel 3Pathology Institute, Kaplan Medical Center, Israel 4Nuclear Medicine Institute, Kaplan Medical Center, Israel *Corresponding author: Taiba Zornitzki, MD, Endocrinology, Diabetes and Metabolism Institute, Kaplan Medical Center, Hebrew University Medical School of Jerusalem, Bilu 1, 76100 Rehovot, Israel, Tel: +972-894- 41315, Fax: +972-8 944-1912, E-mail: [email protected] Context 2. This is the first reported case of an adrenal neuroblastoma occurring in an adult patient with NF1 presenting as a large Neurofibromatosis type 1 (NF1) is a genetic disorder asso- adrenal mass with increased catecholamine levels mimicking ciated with an increased risk of malignant disorders. Adrenal a pheochromocytoma. neuroblastoma is considered an extremely rare tumor in adults and was not previously described in association with NF1. 3. This case demonstrates the clinical overlap between pheo- Case description: A 42-year-old normotensive woman with chromocytoma and neuroblastoma. typical signs of NF1 underwent evaluation for abdominal pain, Keywords and a large 14 × 10 × 16 cm left adrenal mass displacing the Adrenal neuroblastoma, Neurofibromatosis type 1, Pheo- spleen, pancreas and colon was found. An initial diagnosis of chromocytoma, Neural crest-derived tumors pheochromocytoma was done based on the known strong association between pheochromocytoma, NF1 and increased catecholamine levels. -

MDM2 Gene Polymorphisms May Be Associated with Tumor
in vivo 31 : 357-363 (2017) doi:10.21873/invivo.11067 The Role of p16 and MDM2 Gene Polymorphisms in Prolactinoma: MDM2 Gene Polymorphisms May Be Associated with Tumor Shrinkage SEDA TURGUT 1, MUZAFFER ILHAN 2, SAIME TURAN 3, OZCAN KARAMAN 2, ILHAN YAYLIM 3, OZLEM KUCUKHUSEYIN 3 and ERTUGRUL TASAN 2 Departments of 1Internal Medicine, and 2Endocrinology and Metabolism, Bezmialem Vakif University, Istanbul, Turkey; 3Department of Molecular Medicine, The Institute of Experimental Medicine, Istanbul University, Istanbul, Turkey → Abstract. Aim: Prolactinomas are thought to arise from genotype (TT+GG) of MDM2 SNP309T G was clonal expansion of a single mutated cell which is subjected significantly higher than in heterozygous genotype (TG) to growth stimuli of several permissive factors, although the carriers (odds ratio(OR)=0.18, 95% confidence pathogenetic mechanisms underlying tumorigenesis remain interval(CI)=0.06-0.58; p=0.003). Conclusion: This study unclear. The present study aimed to investigate the role of showed that p16 and MDM2 polymorphisms do not play a → → p16 (540C G and 580C T) and mouse double minute 2 decisive role in tumorigenesis, but some genotypes of these → (MDM2) (SNP309T G) gene polymorphisms in polymorphisms might be associated with follow-up tumorigenesis and characteristics of prolactinoma. Patients characteristics of prolactinoma. and Methods: A total of 74 patients with prolactinoma and 100 age- and gender-matched healthy individuals were Prolactinoma is the most frequent type of functional pituitary enrolled in the study. Serum prolactin levels were measured tumor, with an estimated prevalence of approximately 45 by enzyme-linked immunosorbent assay (ELISA). p16 and cases per 100,000 population in adults (1). -

Endocrine Surgery Goals and Objectives
Lenox Hill Hospital Department of Surgery Endocrine Surgery Goals and Objectives Medical Knowledge and Patient Care: Residents must demonstrate knowledge and application of the pathophysiology and epidemiology of the diseases listed below for this rotation, with the pertinent clinical and laboratory findings, differential diagnosis and therapeutic options including preventive measures, and procedural knowledge. They must show that they are able to gather accurate and relevant information using medical interviewing, physical examination, appropriate diagnostic workup, and use of information technology. They must be able to synthesize and apply information in the clinical setting to make informed recommendations about preventive, diagnostic and therapeutic options, based on clinical judgement, scientific evidence, and patient preferences. They should be able to prescribe, perform, and interpret surgical procedures listed below for this rotation. All Residents are expected to understand: 1. Normal physiology and anatomy of the thyroid glands. 2. Normal physiology and anatomy of the parathyroid glands. 3. Normal physiology and anatomy of the adrenal glands 4. Normal physiology of the pancreatic neuroendocrine cells. 5. Normal physiology of the pituitary gland. Disease-Based Learning Objectives: Hyperfunctioning Thyroid and Hypothyroid State: 1. Physiology of Grave’s disease and toxic goiter. 2. Management of a patient in hyperthyroid storm. 3. Medical and surgical treatment options for hyperthyroidism. 4. Physiology of Hashimoto’s thyroiditis and hypothyroidism. Thyroid Neoplasm: 1. Workup of a cold thyroid nodule. 2. Surgical management of papillary, follicular, medullary, and anaplastic thyroid carcinoma. 3. Adjuvant therapy for thyroid neoplasms. 4. Postoperative medical management and long-term follow-up of thyroid cancer. Hyperparathyroidism: 1. Diagnosis and work-up of hypercalcemia and primary, secondary, and tertiary hyperparathyroidism. -

Genetic Landscape of Papillary Thyroid Carcinoma and Nuclear Architecture: an Overview Comparing Pediatric and Adult Populations
cancers Review Genetic Landscape of Papillary Thyroid Carcinoma and Nuclear Architecture: An Overview Comparing Pediatric and Adult Populations 1, 2, 2 3 Aline Rangel-Pozzo y, Luiza Sisdelli y, Maria Isabel V. Cordioli , Fernanda Vaisman , Paola Caria 4,*, Sabine Mai 1,* and Janete M. Cerutti 2 1 Cell Biology, Research Institute of Oncology and Hematology, University of Manitoba, CancerCare Manitoba, Winnipeg, MB R3E 0V9, Canada; [email protected] 2 Genetic Bases of Thyroid Tumors Laboratory, Division of Genetics, Department of Morphology and Genetics, Universidade Federal de São Paulo/EPM, São Paulo, SP 04039-032, Brazil; [email protected] (L.S.); [email protected] (M.I.V.C.); [email protected] (J.M.C.) 3 Instituto Nacional do Câncer, Rio de Janeiro, RJ 22451-000, Brazil; [email protected] 4 Department of Biomedical Sciences, University of Cagliari, 09042 Cagliari, Italy * Correspondence: [email protected] (P.C.); [email protected] (S.M.); Tel.: +1-204-787-2135 (S.M.) These authors contributed equally to this paper. y Received: 29 September 2020; Accepted: 26 October 2020; Published: 27 October 2020 Simple Summary: Papillary thyroid carcinoma (PTC) represents 80–90% of all differentiated thyroid carcinomas. PTC has a high rate of gene fusions and mutations, which can influence clinical and biological behavior in both children and adults. In this review, we focus on the comparison between pediatric and adult PTC, highlighting genetic alterations, telomere-related genomic instability and changes in nuclear organization as novel biomarkers for thyroid cancers. Abstract: Thyroid cancer is a rare malignancy in the pediatric population that is highly associated with disease aggressiveness and advanced disease stages when compared to adult population. -

Ganglioneuroblastoma As Vasoactive Intestinal Polypeptide-Secreting10.5005/Jp-Journals-10002-1167 Tumor: Rare Case Report in a Child Case Report
WJOES Ganglioneuroblastoma as Vasoactive Intestinal Polypeptide-secreting10.5005/jp-journals-10002-1167 Tumor: Rare Case Report in a Child CASE REPORT Ganglioneuroblastoma as Vasoactive Intestinal Polypeptide-secreting Tumor: Rare Case Report in a Child 1Basant Kumar, 2Vijai D Upadhyaya, 3Ram Nawal Rao, 4Sheo Kumar ABSTRACT than 60 cases of pediatric VIP-secreting tumors.3 Most Pathologically elevated vasoactive intestinal polypeptide (VIP) of them are either adrenal pheochromocytoma or mixed plasma levels cause secretory diarrhea with excessive loss of pheochromocytoma-ganglioneuroma tumors. Mason water and electrolyte and is characterized by the typical symp- et al,4 first described the secretory nature of neuroblas- toms of hypokalemia and metabolic acidosis. It rarely occurs toma and vasoactive intestinal peptide (VIP) can be in patients with non-pancreatic disease. Despite the clinical severity, diagnosis of a VIP-secreting tumor is often delayed. produced by the mature neurogenic tumors. We herein We herein present a 14-month-old boy having prolonged present a 14 months old boy having prolonged therapy- therapy-resistant secretory diarrhea, persistent hypokalemia resistant secretory diarrhea, persistent hypokalemia with with tissue diagnosis of ganglioneuroblastoma and raised plasma VIP-levels. tissue diagnosis of ganglioneuroblastoma and briefly review the literature. Keywords: Ganglioneuroblastoma, Secretory diarrhea, VIPoma. CASE REPORT How to cite this article: Kumar B, Upadhyaya VD, Rao RN, Kumar S. Ganglioneuroblastoma as Vasoactive Intestinal A 14-month-old boy, weighing 9 kg with advanced symp- Polypeptide-secreting Tumor: Rare Case Report in a Child. World J Endoc Surg 2015;7(2):47-50. toms of persistent secretory diarrhea, hypokalemia and metabolic acidosis was referred to us with radiological Source of support: Nil (computed tomography) diagnosis of retroperitoneal Conflict of interest: None mass. -

Clinical Radiation Oncology Review
Clinical Radiation Oncology Review Daniel M. Trifiletti University of Virginia Disclaimer: The following is meant to serve as a brief review of information in preparation for board examinations in Radiation Oncology and allow for an open-access, printable, updatable resource for trainees. Recommendations are briefly summarized, vary by institution, and there may be errors. NCCN guidelines are taken from 2014 and may be out-dated. This should be taken into consideration when reading. 1 Table of Contents 1) Pediatrics 6) Gastrointestinal a) Rhabdomyosarcoma a) Esophageal Cancer b) Ewings Sarcoma b) Gastric Cancer c) Wilms Tumor c) Pancreatic Cancer d) Neuroblastoma d) Hepatocellular Carcinoma e) Retinoblastoma e) Colorectal cancer f) Medulloblastoma f) Anal Cancer g) Epndymoma h) Germ cell, Non-Germ cell tumors, Pineal tumors 7) Genitourinary i) Craniopharyngioma a) Prostate Cancer j) Brainstem Glioma i) Low Risk Prostate Cancer & Brachytherapy ii) Intermediate/High Risk Prostate Cancer 2) Central Nervous System iii) Adjuvant/Salvage & Metastatic Prostate Cancer a) Low Grade Glioma b) Bladder Cancer b) High Grade Glioma c) Renal Cell Cancer c) Primary CNS lymphoma d) Urethral Cancer d) Meningioma e) Testicular Cancer e) Pituitary Tumor f) Penile Cancer 3) Head and Neck 8) Gynecologic a) Ocular Melanoma a) Cervical Cancer b) Nasopharyngeal Cancer b) Endometrial Cancer c) Paranasal Sinus Cancer c) Uterine Sarcoma d) Oral Cavity Cancer d) Vulvar Cancer e) Oropharyngeal Cancer e) Vaginal Cancer f) Salivary Gland Cancer f) Ovarian Cancer & Fallopian -

Validation of Algorithms to Identify Pancreatic Cancer and Thyroid Neoplasms from Health Insurance Claims Data in a 10-Year Foll
Validation of Algorithms to Identify Pancreatic Cancer and Thyroid Neoplasms From Health Insurance Claims Data in a 10-Year Follow-Up Study Caihua Liang, MD, PhD1*; Monica L Bertoia, MPH, PhD1; C Robin Clifford, MS1; Yan Ding, MSc1; Qing Qiao, MD, PhD2; Joshua J Gagne, PharmD, ScD1,3; David D Dore, PharmD, PhD1 1Optum Epidemiology, Boston, MA/Ann Arbor, MI, USA; 2Global Medical Affair AstraZeneca, Gothenburg, Sweden; 3Division of Pharmacoepidemiology, Department of Medicine, Brigham and Women’s Hospital and Harvard Medical School, Boston, USA. *Corresponding author: [email protected]. This study was funded through a research contract between Optum Epidemiology and AstraZeneca. Background Methods (cont.) Identification of cancer events in health insurance claims data can be Figure 1. Pancreatic cancer and thyroid neoplasm relaxed and restricted challenging and subject to misclassification. Given the low incidence of algorithms certain cancers, robust performance evaluation requires a large sample size PANCREATIC CANCER THYROID NEOPLASMS with long-term follow-up. ICD-9 Codes ICD-9 Codes (Malignant neoplasm of …) 193 Malignant neoplasm of thyroid gland 157.X … pancreas 226 Benign neoplasm of thyroid gland Objective 157.0 … head of pancreas 157.1 … body of pancreas Thyroid Cancer Benign Thyroid Neoplasm To validate algorithms for potential incident pancreatic cancer and thyroid 157.2 … tail of pancreas neoplasms in a 10-year follow-up study using a health insurance claims 157.3 … pancreatic duct Restricted Algorithm: Restricted Algorithm: 157.4 … islets of Langerhans a+b+c a+b+c database. 157.8 … other specified sites of Relaxed Algorithm: Relaxed Algorithm: pancreas a+b or a+c a+b or a+c 157.9 … pancreas, part unspecified Data Source a. -

Small Extra-Adrenal Pheochromocytoma Causing Severe Hypertension in an Elderly Patient
635 Hypertens Res Vol.29 (2006) No.8 p.635-638 Case Report Small Extra-Adrenal Pheochromocytoma Causing Severe Hypertension in an Elderly Patient Einosuke MIZUTA1), Toshihiro HAMADA2), Shin-ichi TANIGUCHI2), Masaki SHIMOYAMA2), Takahiro NAWADA3), Junichiro MIAKE2), Yasuhiro KAETSU2), Li PEILI2), Kiyosuke ISHIGURO4), Shingo ISHIGURO4), Osamu IGAWA2), Chiaki SHIGEMASA2), and Ichiro HISATOME1) We report the case of a 67-year-old woman with severe hypertension caused by an extra-adrenal pheochro- mocytoma. The tumor was detected by 131I metaiodobenzylguanidine scintigraphy and it was found to be small (2 cm ø) by enhanced CT. After the extirpation of the tumor, the blood pressure of the patient imme- diately normalized. It should be taken into account that a small extra-adrenal pheochromocytoma can be one of the causes of secondary hypertension in elderly patients. Since small extra-adrenal pheochromocytomas are difficult to detect, it is also important to perform suitable examinations to establish the diagnosis. Fur- thermore, we emphasize the importance of an accurate diagnosis in elderly patients with pheochromocy- toma, for they often have less symptomatology and more severe cardiovascular complications due to refractory hypertension than younger patients. (Hypertens Res 2006; 29: 635–638) Key Words: pheochromocytoma, extra-adrenal, hypertension, diagnosis mately 30% of these patients do not present these signs (7). Introduction Since most of their clinical signs and symptoms are derived from the actions of catecholamines secreted from the adrenal Pheochromocytoma is one of the major causes of secondary glands, adrenal pheochromocytoma induces more severe clin- hypertension, drug-resistant hypertension, and malignant ical signs than those observed in extra-adrenal pheochro- hypertension (1–3), but the rate of occurrence of the tumor mocytoma (7). -

(Glucagon) – New Drug Approval
Baqsimi™ (glucagon) – New drug approval • On July 24, 2019, the FDA announced the approval of Eli Lilly’s Baqsimi (glucagon) nasal powder, for the treatment of severe hypoglycemia in patients with diabetes ages 4 years and above. • Severe hypoglycemia occurs when a patient’s blood sugar levels fall to a level where he or she becomes confused or unconscious or suffers from other symptoms that require assistance from another person to treat. Typically, severe hypoglycemia occurs in people with diabetes who are using insulin treatment. — Injectable glucagon for the treatment of hypoglycemia has been approved for use in the U.S. for several decades. • Baqsimi is the first nasally administered formulation of glucagon. It is ready to use with no reconstitution required. • The efficacy of Baqsimi was evaluated in an open-label, crossover study in 70 adult patients with type 1 diabetes. The efficacy of a single 3 mg dose of Baqsimi was compared to a 1 mg dose of intramuscular glucagon (IMG). The primary efficacy measure was the proportion of patients achieving treatment success, which was defined as either an increase in blood glucose to ≥ 70 mg/dL or an increase of ≥ 20 mg/dL from glucose nadir within 30 minutes after receiving glucagon, without receiving additional actions to increase the blood glucose level. — Baqsimi demonstrated non-inferiority to IMG in reversing insulin-induced hypoglycemia with 100% of Baqsimi-treated patients and 100% of IMG-treated patients achieving treatment success. • The efficacy of Baqsimi was also evaluated in a similarly designed study in 83 adult patients with type 1 or type 2 diabetes. -
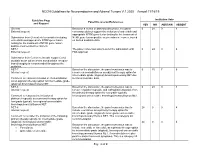
NCCN Guidelines for Neuroendocrine and Adrenal Tumors V.1.2020 – Annual 11/18/19
NCCN Guidelines for Neuroendocrine and Adrenal Tumors V.1.2020 – Annual 11/18/19 Guideline Page Institution Vote Panel Discussion/References and Request YES NO ABSTAIN ABSENT General Based on a review of data and discussion, the panel 0 24 0 4 External request: consensus did not support the inclusion of entrectinib and appropriate NTRK gene fusion testing for the treatment of Submission from Genentech to consider including NTRK gene fusion-positive neuroendocrine cancer, based entrectinib and appropriate NTRK gene fusion on limited available data. testing for the treatment of NTRK gene fusion- positive neuroendocrine cancers. NET-1 The panel consensus was to defer the submission until 0 24 0 4 External request: FDA approval. Submission from Curium to include copper Cu 64 dotatate as an option where somatostatin receptor- based imaging is recommended throughout the guideline. NET-7 Based on the discussion, the panel consensus was to 0 15 7 6 Internal request: remove chemoradiation as an adjuvant therapy option for intermediate grade (atypical) bronchopulmonary NET due Comment to reassess inclusion of chemoradiation to limited available data. as an adjuvant therapy option for intermediate grade (atypical) bronchopulmonary NET. NET-8 Based on the discussion, the panel consensus was to 0 24 0 4 Internal request: remove cisplatin/etoposide and carboplatin/etoposide from the primary therapy option for low grade (typical), Comment to reassess the inclusion of locoregional unresectable bronchopulmonary/thymus NET. platinum/etoposide as a primary therapy option for low grade (typical), locoregional unresectable bronchopulmonary/thymus NET. NET-8 Based on the discussion, the panel consensus was to 24 0 0 4 Internal request: include everolimus as a primary therapy option for intermediate grade (atypical), locoregional unresectable Comment to consider the inclusion of the following bronchopulmonary/thymus NET.