Neoplastic Metastases to the Endocrine Glands
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Risk of Tumour Recurrence in Patients Undergoing Renal
The Risk of Tumour Recurrence in Patients Undergoing Renal Transplantation for End-stage Renal Disease after Previous Treatment for a Urological Cancer: A Systematic Review Romain Boissier, Vital Hevia, Harman Max Bruins, Klemens Budde, Arnaldo Figueiredo, Enrique Lledó-García, Jonathon Olsburgh, Heinz Regele, Claire Fraser Taylor, Rhana Hassan Zakri, et al. To cite this version: Romain Boissier, Vital Hevia, Harman Max Bruins, Klemens Budde, Arnaldo Figueiredo, et al.. The Risk of Tumour Recurrence in Patients Undergoing Renal Transplantation for End-stage Renal Disease after Previous Treatment for a Urological Cancer: A Systematic Review. European Urology, Elsevier, 2018, pp.94 - 108. 10.1016/j.eururo.2017.07.017. hal-01792732 HAL Id: hal-01792732 https://hal-amu.archives-ouvertes.fr/hal-01792732 Submitted on 18 May 2018 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. 1 The risk of tumour recurrence in patients undergoing renal transplantation for end- stage renal disease after previous treatment for a urological cancer: a systematic review Romain Boissier1*, Vital Hevia2*, Harman Max Bruins3, Klemens Budde4, Arnaldo Figueiredo5, Enrique Lledó García6, Jonathon Olsburgh7, Heinz Regele8, Claire Fraser Taylor9, Rhana Hassan Zakri7, Cathy Yuhong Yuan10 and Alberto Breda11 * These authors contributed equally and share the first authorship 1. -

Adrenal Cancer Causes, Risk Factors, and Prevention Adrenal
cancer.org | 1.800.227.2345 Adrenal Cancer Causes, Risk Factors, and Prevention Risk Factors A risk factor is anything that affects your chance of getting a disease such as cancer. Learn more about the risk factors for adrenal cancer. ● Adrenal Cancer Risk Factors ● What Causes Adrenal Cancer? Prevention Since there are no known preventable risk factors for this cancer, it is not possible to prevent this disease. Adrenal Cancer Risk Factors A risk factor is anything that changes your chance of getting a disease such as cancer. Different cancers have different risk factors. Some risk factors, like smoking, can be changed. Others, like a person’s age or family history, can’t be changed. Scientists have found few risk factors that make a person more likely to develop adrenal cancer. Even if a patient does have one or more risk factors for adrenal cancer, it is impossible to know for sure how much that risk factor contributed to causing the cancer. 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 But having a risk factor, or even several, does not mean that you will get the disease. Many people with risk factors never develop adrenal cancer, while others with this disease may have few or no known risk factors. Genetic syndromes The majority of adrenal cortex cancers are not inherited (sporadic), but some (up to 15%) are caused by a genetic defect. This is more common in adrenal cancers in children. Li-Fraumeni syndrome The Li-Fraumeni syndrome is a rare condition that is most often caused by a defect in the TP53 gene. -

Wilms Tumour (Nephroblastoma) – Brief Information
Wilms Tumour (Nephroblastoma) – Brief information Copyright © 2017 Competence Network Paediatric Oncology and Haematology Author: Maria Yiallouros, created 2009/02/12, Editor: Maria Yiallouros, Release: Prof. Dr. med. Norbert Graf, English Translation: Dr. med. habil. Gesche Tallen, Last modified: 2017/06/27 Kinderkrebsinfo is sponsored by Deutsche Kinderkrebsstiftung Wilms Tumour (Nephroblastoma) – Brief information Page 2 Table of Content 1. General information on the disease ................................................................................... 3 2. Incidence .......................................................................................................................... 3 3. Causes ............................................................................................................................. 4 4. Symptoms ........................................................................................................................ 4 5. Diagnosis ......................................................................................................................... 4 5.1. Diagnostic imaging ....................................................................................................... 5 5.2. More tests to confirm diagnosis and to assess tumour spread (metastases) ..................... 5 5.3. Tests for preparing the treatment ................................................................................... 5 5.4. Obtaining a tumour sample (biopsy) ............................................................................. -

Partial Nephrectomy for Renal Cancer: Part I
REVIEW ARTICLE Partial nephrectomy for renal cancer: Part I BJUIBJU INTERNATIONAL Paul Russo Department of Surgery, Urology Service, and Weill Medical College, Cornell University, Memorial Sloan Kettering Cancer Center, New York, NY, USA INTRODUCTION The Problem of Kidney Cancer Kidney Cancer Is The Third Most Common Genitourinary Tumour With 57 760 New Cases And 12 980 Deaths Expected In 2009 [1]. There Are Currently Two Distinct Groups Of Patients With Kidney Cancer. The First Consists Of The Symptomatic, Large, Locally Advanced Tumours Often Presenting With Regional Adenopathy, Adrenal Invasion, And Extension Into The Renal Vein Or Inferior Vena Cava. Despite Radical Nephrectomy (Rn) In Conjunction With Regional Lymphadenectomy And Adrenalectomy, Progression To Distant Metastasis And Death From Disease Occurs In ≈30% Of These Patients. For Patients Presenting With Isolated Metastatic Disease, Metastasectomy In Carefully Selected Patients Has Been Associated With Long-term Survival [2]. For Patients With Diffuse Metastatic Disease And An Acceptable Performance Status, Cytoreductive Nephrectomy Might Add Several Additional Months Of Survival, As Opposed To Cytokine Therapy Alone, And Prepare Patients For Integrated Treatment, Now In Neoadjuvant And Adjuvant Clinical Trials, With The New Multitargeted Tyrosine Kinase Inhibitors (Sunitinib, Sorafenib) And Mtor Inhibitors (Temsirolimus, Everolimus) [3,4]. The second groups of patients with kidney overall survival. The explanation for this cancer are those with small renal tumours observation is not clear and could indicate (median tumour size <4 cm, T1a), often that aggressive surgical treatment of small incidentally discovered in asymptomatic renal masses in patients not in imminent patients during danger did not counterbalance a population imaging for of patients with increasingly virulent larger nonspecific abdominal tumours. -

Endocrine Pathology (537-577)
LABORATORY INVESTIGATION THE BASIC AND TRANSLATIONAL PATHOLOGY RESEARCH JOURNAL LI VOLUME 99 | SUPPLEMENT 1 | MARCH 2019 2019 ABSTRACTS ENDOCRINE PATHOLOGY (537-577) MARCH 16-21, 2019 PLATF OR M & 2 01 9 ABSTRACTS P OSTER PRESENTATI ONS EDUCATI ON C O M MITTEE Jason L. Hornick , C h air Ja mes R. Cook R h o n d a K. Y a nti s s, Chair, Abstract Revie w Board S ar a h M. Dr y and Assign ment Co m mittee Willi a m C. F a q ui n Laura W. La mps , Chair, C ME Subco m mittee C ar ol F. F ar v er St e v e n D. Billi n g s , Interactive Microscopy Subco m mittee Y uri F e d ori w Shree G. Shar ma , Infor matics Subco m mittee Meera R. Ha meed R aj a R. S e et h al a , Short Course Coordinator Mi c h ell e S. Hir s c h Il a n W ei nr e b , Subco m mittee for Unique Live Course Offerings Laksh mi Priya Kunju D a vi d B. K a mi n s k y ( Ex- Of ici o) A n n a M ari e M ulli g a n Aleodor ( Doru) Andea Ri s h P ai Zubair Baloch Vi nita Parkas h Olca Bast urk A nil P ar w a ni Gregory R. Bean , Pat h ol o gist-i n- Trai ni n g D e e p a P atil D a ni el J. -

Wilms' Tumour (Nephroblastoma)
Wilms’ tumour (nephroblastoma) Wilms’ tumour is generally found only in children and very rarely in adults. JANET E POOLE, MB BCh, DCH (SA), FCP (SA) Paed Professor, Department of Paediatrics, Charlotte Maxeke Johannesburg Academic Hospital and University of the Witwatersrand, Johannesburg Janet Poole qualified as a medical doctor in 1978 at the University of the Witwatersrand and became a specialist paediatrician in 1983. She commenced work in the Paediatric Haematology/Oncology Unit at the Johannesburg Hospital in 1984 and has 25 years’ experience in that field. She was head of the Chris Hani Baragwanath Paediatric Haematology/Oncology Unit from 1989 to 1997, after which she became head of the Unit at Johannesburg Hospital. Her special interests are childhood leukaemia, Wilms’ tumour, and inherited haemoglobin defects. She has been involved with CHOC (a parent support group) since starting work in the unit. Correspondence to: J Poole ([email protected]) a bleeding diathesis, polycythaemia, weight loss, urinary infection, Epidemiology diarrhoea or constipation. Wilms’ tumour or nephroblastoma is a cancer of the kidney that The differential diagnosis of a renal mass includes hydronephrosis, typically occurs in children and very rarely in adults. The common polycystic kidney disease and infrequently xanthogranulomatous name is an eponym, referring to Dr Max Wilms, the German pyelonephritis. Non-renal peritoneal masses include neuroblastoma surgeon who first described this type of tumour in 1899. Wilms’ and teratoma (Fig. 1). tumour is the most common form of kidney cancer in children and is also known as nephroblastoma. Nephro means kidney, and a blastoma is a tumour of embryonic tissue that has not yet fully developed. -

MDM2 Gene Polymorphisms May Be Associated with Tumor
in vivo 31 : 357-363 (2017) doi:10.21873/invivo.11067 The Role of p16 and MDM2 Gene Polymorphisms in Prolactinoma: MDM2 Gene Polymorphisms May Be Associated with Tumor Shrinkage SEDA TURGUT 1, MUZAFFER ILHAN 2, SAIME TURAN 3, OZCAN KARAMAN 2, ILHAN YAYLIM 3, OZLEM KUCUKHUSEYIN 3 and ERTUGRUL TASAN 2 Departments of 1Internal Medicine, and 2Endocrinology and Metabolism, Bezmialem Vakif University, Istanbul, Turkey; 3Department of Molecular Medicine, The Institute of Experimental Medicine, Istanbul University, Istanbul, Turkey → Abstract. Aim: Prolactinomas are thought to arise from genotype (TT+GG) of MDM2 SNP309T G was clonal expansion of a single mutated cell which is subjected significantly higher than in heterozygous genotype (TG) to growth stimuli of several permissive factors, although the carriers (odds ratio(OR)=0.18, 95% confidence pathogenetic mechanisms underlying tumorigenesis remain interval(CI)=0.06-0.58; p=0.003). Conclusion: This study unclear. The present study aimed to investigate the role of showed that p16 and MDM2 polymorphisms do not play a → → p16 (540C G and 580C T) and mouse double minute 2 decisive role in tumorigenesis, but some genotypes of these → (MDM2) (SNP309T G) gene polymorphisms in polymorphisms might be associated with follow-up tumorigenesis and characteristics of prolactinoma. Patients characteristics of prolactinoma. and Methods: A total of 74 patients with prolactinoma and 100 age- and gender-matched healthy individuals were Prolactinoma is the most frequent type of functional pituitary enrolled in the study. Serum prolactin levels were measured tumor, with an estimated prevalence of approximately 45 by enzyme-linked immunosorbent assay (ELISA). p16 and cases per 100,000 population in adults (1). -

Clinical Radiation Oncology Review
Clinical Radiation Oncology Review Daniel M. Trifiletti University of Virginia Disclaimer: The following is meant to serve as a brief review of information in preparation for board examinations in Radiation Oncology and allow for an open-access, printable, updatable resource for trainees. Recommendations are briefly summarized, vary by institution, and there may be errors. NCCN guidelines are taken from 2014 and may be out-dated. This should be taken into consideration when reading. 1 Table of Contents 1) Pediatrics 6) Gastrointestinal a) Rhabdomyosarcoma a) Esophageal Cancer b) Ewings Sarcoma b) Gastric Cancer c) Wilms Tumor c) Pancreatic Cancer d) Neuroblastoma d) Hepatocellular Carcinoma e) Retinoblastoma e) Colorectal cancer f) Medulloblastoma f) Anal Cancer g) Epndymoma h) Germ cell, Non-Germ cell tumors, Pineal tumors 7) Genitourinary i) Craniopharyngioma a) Prostate Cancer j) Brainstem Glioma i) Low Risk Prostate Cancer & Brachytherapy ii) Intermediate/High Risk Prostate Cancer 2) Central Nervous System iii) Adjuvant/Salvage & Metastatic Prostate Cancer a) Low Grade Glioma b) Bladder Cancer b) High Grade Glioma c) Renal Cell Cancer c) Primary CNS lymphoma d) Urethral Cancer d) Meningioma e) Testicular Cancer e) Pituitary Tumor f) Penile Cancer 3) Head and Neck 8) Gynecologic a) Ocular Melanoma a) Cervical Cancer b) Nasopharyngeal Cancer b) Endometrial Cancer c) Paranasal Sinus Cancer c) Uterine Sarcoma d) Oral Cavity Cancer d) Vulvar Cancer e) Oropharyngeal Cancer e) Vaginal Cancer f) Salivary Gland Cancer f) Ovarian Cancer & Fallopian -

(Pro)Renin Receptor (PRR) Expression in Renal Tumours
diagnostics Article Clinical Implications of (Pro)renin Receptor (PRR) Expression in Renal Tumours Jon Danel Solano-Iturri 1,2,3, Enrique Echevarría 4, Miguel Unda 5, Ana Loizaga-Iriarte 5, Amparo Pérez-Fernández 5, Javier C. Angulo 6, José I. López 3,7 and Gorka Larrinaga 3,4,8,* 1 Department of Pathology, Donostia University Hospital, 20014 Donostia/San Sebastian, Spain; [email protected] 2 Department of Medical-Surgical Specialities, Faculty of Medicine and Nursing, University of the Basque Country (UPV/EHU), 48940 Leioa, Spain 3 Biocruces-Bizkaia Health Research Institute, 48903 Barakaldo, Spain; [email protected] 4 Department of Physiology, Faculty of Medicine and Nursing, University of the Basque Country (UPV/EHU), 48940 Leioa, Spain; [email protected] 5 Department of Urology, Basurto University Hospital, University of the Basque Country (UPV/EHU), 48013 Bilbao, Spain; [email protected] (M.U.); [email protected] (A.L.-I.); [email protected] (A.P.-F.) 6 Clinical Department. Faculty of Medical Sciences. European University of Madrid, 28905 Getafe, Spain; [email protected] 7 Department of Pathology, Cruces University Hospital, 48903 Barakaldo, Spain 8 Department of Nursing, Faculty of Medicine and Nursing, University of the Basque Country (UPV/EHU), 48940 Leioa, Spain * Correspondence: [email protected] Citation: Solano-Iturri, J.D.; Abstract: (1) Background: Renal cancer is one of the most frequent malignancies in Western countries, Echevarría, E.; Unda, M.; with an unpredictable clinical outcome, partly due to its high heterogeneity and the scarcity of Loizaga-Iriarte, A.; Pérez-Fernández, reliable biomarkers of tumour progression. -
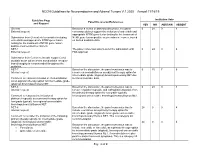
NCCN Guidelines for Neuroendocrine and Adrenal Tumors V.1.2020 – Annual 11/18/19
NCCN Guidelines for Neuroendocrine and Adrenal Tumors V.1.2020 – Annual 11/18/19 Guideline Page Institution Vote Panel Discussion/References and Request YES NO ABSTAIN ABSENT General Based on a review of data and discussion, the panel 0 24 0 4 External request: consensus did not support the inclusion of entrectinib and appropriate NTRK gene fusion testing for the treatment of Submission from Genentech to consider including NTRK gene fusion-positive neuroendocrine cancer, based entrectinib and appropriate NTRK gene fusion on limited available data. testing for the treatment of NTRK gene fusion- positive neuroendocrine cancers. NET-1 The panel consensus was to defer the submission until 0 24 0 4 External request: FDA approval. Submission from Curium to include copper Cu 64 dotatate as an option where somatostatin receptor- based imaging is recommended throughout the guideline. NET-7 Based on the discussion, the panel consensus was to 0 15 7 6 Internal request: remove chemoradiation as an adjuvant therapy option for intermediate grade (atypical) bronchopulmonary NET due Comment to reassess inclusion of chemoradiation to limited available data. as an adjuvant therapy option for intermediate grade (atypical) bronchopulmonary NET. NET-8 Based on the discussion, the panel consensus was to 0 24 0 4 Internal request: remove cisplatin/etoposide and carboplatin/etoposide from the primary therapy option for low grade (typical), Comment to reassess the inclusion of locoregional unresectable bronchopulmonary/thymus NET. platinum/etoposide as a primary therapy option for low grade (typical), locoregional unresectable bronchopulmonary/thymus NET. NET-8 Based on the discussion, the panel consensus was to 24 0 0 4 Internal request: include everolimus as a primary therapy option for intermediate grade (atypical), locoregional unresectable Comment to consider the inclusion of the following bronchopulmonary/thymus NET. -

Multiple Endocrine Neoplasia Type 1 (MEN1)
Lab Management Guidelines v2.0.2019 Multiple Endocrine Neoplasia Type 1 (MEN1) MOL.TS.285.A v2.0.2019 Introduction Multiple Endocrine Neoplasia Type 1 (MEN1) is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline MEN1 Known Familial Mutation Analysis 81403 MEN1 Deletion/Duplication Analysis 81404 MEN1 Full Gene Sequencing 81405 What is Multiple Endocrine Neoplasia Type 1 Definition Multiple Endocrine Neoplasia Type 1 (MEN1) is an inherited form of tumor predisposition characterized by multiple tumors of the endocrine system. Incidence or Prevalence MEN1 has a prevalence of 1/10,000 to 1/100,000 individuals.1 Symptoms The presenting symptom in 90% of individuals with MEN1 is primary hyperparathyroidism (PHPT). Parathyroid tumors cause overproduction of parathyroid hormone which leads to hypercalcemia. The average age of onset is 20-25 years. Parathyroid carcinomas are rare in individuals with MEN1.2,3,4 Pituitary tumors are seen in 30-40% of individuals and are the first clinical manifestation in 10% of familial cases and 25% of simplex cases. Tumors are typically solitary and there is no increased prevalence of pituitary carcinoma in individuals with MEN1.2,5 © eviCore healthcare. All Rights Reserved. 1 of 9 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines v2.0.2019 Prolactinomas are the most commonly seen pituitary subtype and account for 60% of pituitary adenomas. -

Tnm Frequently Asked Questions (Faq’S)
TNM FREQUENTLY ASKED QUESTIONS (FAQ’S) The TNM Project Committee receives questions concerning the use of TNM and how to interpret rules in specific situations. Some questions and answers are listed below by category for your convenience. These FAQs can th also be found in the TNM Supplement: a Commentary on Uniform Use, 4 Edition, 2012 (edited by Ch. Wittekind, C. Compton, J. Brierley, L. H. Sobin). Advice on further questions may be obtained from the TNM Helpdesk by accessing the TNM Classification of Malignant Tumours page at the UICC website www.uicc.org TABLE OF CONTENTS GENERAL QUESTIONS AJCC versus UICC TNM ................................................................................................................3 In situ carcinoma .............................................................................................................................3 Pathological Versus Clinical TNM ...................................................................................................3 When in Doubt ................................................................................................................................4 R Classification ...............................................................................................................................4 R Classification and Tis ..................................................................................................................5 Positive Cytology ............................................................................................................................5