62694474 Hague
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Adrenal Cancer Causes, Risk Factors, and Prevention Adrenal
cancer.org | 1.800.227.2345 Adrenal Cancer Causes, Risk Factors, and Prevention Risk Factors A risk factor is anything that affects your chance of getting a disease such as cancer. Learn more about the risk factors for adrenal cancer. ● Adrenal Cancer Risk Factors ● What Causes Adrenal Cancer? Prevention Since there are no known preventable risk factors for this cancer, it is not possible to prevent this disease. Adrenal Cancer Risk Factors A risk factor is anything that changes your chance of getting a disease such as cancer. Different cancers have different risk factors. Some risk factors, like smoking, can be changed. Others, like a person’s age or family history, can’t be changed. Scientists have found few risk factors that make a person more likely to develop adrenal cancer. Even if a patient does have one or more risk factors for adrenal cancer, it is impossible to know for sure how much that risk factor contributed to causing the cancer. 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 But having a risk factor, or even several, does not mean that you will get the disease. Many people with risk factors never develop adrenal cancer, while others with this disease may have few or no known risk factors. Genetic syndromes The majority of adrenal cortex cancers are not inherited (sporadic), but some (up to 15%) are caused by a genetic defect. This is more common in adrenal cancers in children. Li-Fraumeni syndrome The Li-Fraumeni syndrome is a rare condition that is most often caused by a defect in the TP53 gene. -

Ectopic Adrenocortical Adenoma in the Renal Hilum
Liu et al. Diagnostic Pathology (2016) 11:40 DOI 10.1186/s13000-016-0490-6 CASE REPORT Open Access Ectopic adrenocortical adenoma in the renal hilum: a case report and literature review Yang Liu1,2*, Yue-Feng Jiang1,2, Ye-Lin Wang1,2, Hong-Yi Cao1,2, Liang Wang1,2, Hong-Tao Xu1,2, Qing-Chang Li1,2, Xue-shan Qiu1,2 and En-Hua Wang1,2 Abstract Background: Ectopic (accessory) adrenocortical tissue, also known as adrenal rests, is a developmental abnormality of the adrenal gland. The most common ectopic site is in close proximity to the adrenal glands and along the path of descent or migration of the gonads because of the close spatial relationship between the adrenocortical primordium and gonadal blastema during embryogenesis. Ectopic rests may undergo marked hyperplasia, and occasionally induce ectopic adrenocortical adenomas or carcinomas. Case presentation: A 27-year-old Chinese female patient who presented with amenorrhea of 3 months duration underwent computed tomography urography after ultrasound revealed a solitary mass in the left renal hilum. Histologically, the prominent eosinophilic tumor cells formed an alveolar- or acinar-like configuration. The immunohistochemical profile (alpha-inhibin+, Melan-A+, synaptophysin+) indicated the adrenocortical origin of the tumor, diagnosed as ectopic adrenocortical adenoma. The patient was alive with no tumor recurrence or metastasis at the 3-month follow-up examination. Conclusions: The unusual histological appearance of ectopic adrenocortical adenoma may result in its misdiagnosis as oncocytoma or clear cell renal cell carcinoma, especially if the specimen is limited. This case provides a reminder to pathologists to be aware of atypical cases of this benign tumor. -

Endocrine Pathology (537-577)
LABORATORY INVESTIGATION THE BASIC AND TRANSLATIONAL PATHOLOGY RESEARCH JOURNAL LI VOLUME 99 | SUPPLEMENT 1 | MARCH 2019 2019 ABSTRACTS ENDOCRINE PATHOLOGY (537-577) MARCH 16-21, 2019 PLATF OR M & 2 01 9 ABSTRACTS P OSTER PRESENTATI ONS EDUCATI ON C O M MITTEE Jason L. Hornick , C h air Ja mes R. Cook R h o n d a K. Y a nti s s, Chair, Abstract Revie w Board S ar a h M. Dr y and Assign ment Co m mittee Willi a m C. F a q ui n Laura W. La mps , Chair, C ME Subco m mittee C ar ol F. F ar v er St e v e n D. Billi n g s , Interactive Microscopy Subco m mittee Y uri F e d ori w Shree G. Shar ma , Infor matics Subco m mittee Meera R. Ha meed R aj a R. S e et h al a , Short Course Coordinator Mi c h ell e S. Hir s c h Il a n W ei nr e b , Subco m mittee for Unique Live Course Offerings Laksh mi Priya Kunju D a vi d B. K a mi n s k y ( Ex- Of ici o) A n n a M ari e M ulli g a n Aleodor ( Doru) Andea Ri s h P ai Zubair Baloch Vi nita Parkas h Olca Bast urk A nil P ar w a ni Gregory R. Bean , Pat h ol o gist-i n- Trai ni n g D e e p a P atil D a ni el J. -

17 Endocrine Disorders T Hat Cause Diabetes
1 7 Endocrine Disorders t hat Cause Diabetes Neil A. Hanley Endocrine Sciences Research Group, University of Manchester, Manchester, UK Keypoints • Endocrine causes of diabetes are mainly a result of an excess of • Glucagonoma and somatostatinoma are rare islet cell tumors that hormones that are counter - regulatory to insulin, and act by inhibiting produce hormones that inhibit the secretion and action of insulin. insulin secretion and/or action. • Thyrotoxicosis commonly causes mild glucose intolerance, but overt • Acromegaly is almost always secondary to growth hormone - secreting diabetes only occurs in a tiny minority. adenomas of the anterior pituitary somatotrophs and disturbs glucose • Other endocrinopathies such as primary aldosteronism and primary homeostasis in up to approximately 50% of patients. hyperparathyroidism can disturb glucose homeostasis. • Cushing syndrome is caused by excessive levels of glucocorticoids and • Polycystic ovarian syndrome occurs in 5 – 10% of women of disturbs glucose homeostasis to some degree in over 50% of cases. reproductive age and associates with some degree of glucose • Pheochromocytoma is a tumor of the chromaffi n cells, which in 90% of intolerance or diabetes resulting from insulin resistance in cases is located in the adrenal medulla and causes hyperglycemia in approximately 50% of cases. approximately 50% of cases. or a carcinoid tumor of the lung or pancreas [1] . A small percent- Introduction age of acromegaly occurs within the wider endocrine syndrome of multiple endocrine neoplasia type 1 (MEN1) caused by muta- The primary focus of this chapter is on those endocrine disorders tions in the tumor suppressor gene, MENIN [3] . MEN1 can also that cause hyperglycemia and where effective treatment of the include glucagonomas and somatostatinomas, both of which are endocrinopathy can be expected to normalize the blood glucose separately capable of causing secondary diabetes. -

AACE Annual Meeting 2021 Abstracts Editorial Board
June 2021 Volume 27, Number 6S AACE Annual Meeting 2021 Abstracts Editorial board Editor-in-Chief Pauline M. Camacho, MD, FACE Suleiman Mustafa-Kutana, BSC, MB, CHB, MSC Maywood, Illinois, United States Boston, Massachusetts, United States Vin Tangpricha, MD, PhD, FACE Atlanta, Georgia, United States Andrea Coviello, MD, MSE, MMCi Karel Pacak, MD, PhD, DSc Durham, North Carolina, United States Bethesda, Maryland, United States Associate Editors Natalie E. Cusano, MD, MS Amanda Powell, MD Maria Papaleontiou, MD New York, New York, United States Boston, Massachusetts, United States Ann Arbor, Michigan, United States Tobias Else, MD Gregory Randolph, MD Melissa Putman, MD Ann Arbor, Michigan, United States Boston, Massachusetts, United States Boston, Massachusetts, United States Vahab Fatourechi, MD Daniel J. Rubin, MD, MSc Harold Rosen, MD Rochester, Minnesota, United States Philadelphia, Pennsylvania, United States Boston, Massachusetts, United States Ruth Freeman, MD Joshua D. Safer, MD Nicholas Tritos, MD, DS, FACP, FACE New York, New York, United States New York, New York, United States Boston, Massachusetts, United States Rajesh K. Garg, MD Pankaj Shah, MD Boston, Massachusetts, United States Staff Rochester, Minnesota, United States Eliza B. Geer, MD Joseph L. Shaker, MD Paul A. Markowski New York, New York, United States Milwaukee, Wisconsin, United States CEO Roma Gianchandani, MD Lance Sloan, MD, MS Elizabeth Lepkowski Ann Arbor, Michigan, United States Lufkin, Texas, United States Chief Learning Officer Martin M. Grajower, MD, FACP, FACE Takara L. Stanley, MD Lori Clawges The Bronx, New York, United States Boston, Massachusetts, United States Senior Managing Editor Allen S. Ho, MD Devin Steenkamp, MD Corrie Williams Los Angeles, California, United States Boston, Massachusetts, United States Peer Review Manager Michael F. -
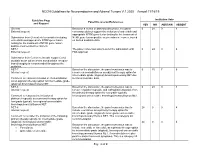
NCCN Guidelines for Neuroendocrine and Adrenal Tumors V.1.2020 – Annual 11/18/19
NCCN Guidelines for Neuroendocrine and Adrenal Tumors V.1.2020 – Annual 11/18/19 Guideline Page Institution Vote Panel Discussion/References and Request YES NO ABSTAIN ABSENT General Based on a review of data and discussion, the panel 0 24 0 4 External request: consensus did not support the inclusion of entrectinib and appropriate NTRK gene fusion testing for the treatment of Submission from Genentech to consider including NTRK gene fusion-positive neuroendocrine cancer, based entrectinib and appropriate NTRK gene fusion on limited available data. testing for the treatment of NTRK gene fusion- positive neuroendocrine cancers. NET-1 The panel consensus was to defer the submission until 0 24 0 4 External request: FDA approval. Submission from Curium to include copper Cu 64 dotatate as an option where somatostatin receptor- based imaging is recommended throughout the guideline. NET-7 Based on the discussion, the panel consensus was to 0 15 7 6 Internal request: remove chemoradiation as an adjuvant therapy option for intermediate grade (atypical) bronchopulmonary NET due Comment to reassess inclusion of chemoradiation to limited available data. as an adjuvant therapy option for intermediate grade (atypical) bronchopulmonary NET. NET-8 Based on the discussion, the panel consensus was to 0 24 0 4 Internal request: remove cisplatin/etoposide and carboplatin/etoposide from the primary therapy option for low grade (typical), Comment to reassess the inclusion of locoregional unresectable bronchopulmonary/thymus NET. platinum/etoposide as a primary therapy option for low grade (typical), locoregional unresectable bronchopulmonary/thymus NET. NET-8 Based on the discussion, the panel consensus was to 24 0 0 4 Internal request: include everolimus as a primary therapy option for intermediate grade (atypical), locoregional unresectable Comment to consider the inclusion of the following bronchopulmonary/thymus NET. -

Pancreatic Gangliocytic Paraganglioma Harboring Lymph
Nonaka et al. Diagnostic Pathology (2017) 12:57 DOI 10.1186/s13000-017-0648-x CASEREPORT Open Access Pancreatic gangliocytic paraganglioma harboring lymph node metastasis: a case report and literature review Keisuke Nonaka1,2, Yoko Matsuda1, Akira Okaniwa3, Atsuko Kasajima2, Hironobu Sasano2 and Tomio Arai1* Abstract Background: Gangliocytic paraganglioma (GP) is a rare neuroendocrine neoplasm, which occurs mostly in the periampullary portion of the duodenum; the majority of the reported cases of duodenal GP has been of benign nature with a low incidence of regional lymph node metastasis. GP arising from the pancreas is extremely rare. To date, only three cases have been reported and its clinical characteristics are largely unknown. Case presentation: A nodule located in the pancreatic head was incidentally detected in an asymptomatic 68-year-old woman. Computed tomography revealed 18-, 8-, and 12-mm masses in the pancreatic head, the pancreatic tail, and the left adrenal gland, respectively. Subsequent genetic examination revealed an absence of mutations in the MEN1 and VHL genes. Macroscopically, the tumor located in the pancreatic head was 22 mm in size and displayed an ill-circumscribed margin along with yellowish-white color. Microscopically, it was composed of three cell components: epithelioid cells, ganglion-like cells, and spindle cells, which led to the diagnosis of GP. The tumor was accompanied by a peripancreatic lymph node metastasis. The tumor in the pancreatic tail was histologically classified as a neuroendocrine tumor (NET) G1 (grade 1, WHO 2010), whereas the tumor in the left adrenal gland was identified as an adrenocortical adenoma. The patient was disease-free at the 12-month follow-up examination. -

Neoplastic Metastases to the Endocrine Glands
27 1 Endocrine-Related A Angelousi et al. Metastases to endocrine 27:1 R1–R20 Cancer organs REVIEW Neoplastic metastases to the endocrine glands Anna Angelousi1, Krystallenia I Alexandraki2, George Kyriakopoulos3, Marina Tsoli2, Dimitrios Thomas2, Gregory Kaltsas2 and Ashley Grossman4,5,6 1Endocrine Unit, 1st Department of Internal Medicine, Laiko Hospital, National and Kapodistrian University of Athens, Athens, Greece 2Endocrine Unit, 1st Department of Propaedeutic Medicine, Laiko University Hospital, Medical School, National and Kapodistrian University of Athens, Athens, Greece 3Department of Pathology, General Hospital ‘Evangelismos’, Αthens, Greece 4Department of Endocrinology, OCDEM, University of Oxford, Oxford, UK 5Neuroendocrine Tumour Unit, Royal Free Hospital, London, UK 6Centre for Endocrinology, Barts and the London School of Medicine, Queen Mary University of London, London, UK Correspondence should be addressed to A Angelousi: [email protected] Abstract Endocrine organs are metastatic targets for several primary cancers, either through Key Words direct extension from nearby tumour cells or dissemination via the venous, arterial and f glands lymphatic routes. Although any endocrine tissue can be affected, most clinically relevant f cancer metastases involve the pituitary and adrenal glands with the commonest manifestations f metastases being diabetes insipidus and adrenal insufficiency respectively. The most common f pituitary primary tumours metastasing to the adrenals include melanomas, breast and lung f adrenal carcinomas, which may lead to adrenal insufficiency in the presence of bilateral adrenal f thyroid involvement. Breast and lung cancers are the most common primaries metastasing to f ovaries the pituitary, leading to pituitary dysfunction in approximately 30% of cases. The thyroid gland can be affected by renal, colorectal, lung and breast carcinomas, and melanomas, but has rarely been associated with thyroid dysfunction. -

A “Tumour Trifecta:” Myelolipomata Arising Within an Adrenocortical Adenoma Ipsilateral to a Synchronous Clear Cell Renal Cell Carcinoma
Malaysian J Pathol 2010; 32(2) : 123 – 128 CASE REPORT A “tumour trifecta:” Myelolipomata arising within an adrenocortical adenoma ipsilateral to a synchronous clear cell renal cell carcinoma. Etienne MAHE B.Sc. M.D and Ihab EL-SHINNAWY FRCPC, FCAP Department of Pathology and Molecular Medicine, McMaster University, Hamilton, ON, Canada Abstract We present an intriguing case of adrenal myelolipomata occurring within an adrenocortical adenoma in concert with an ipsilateral clear cell renal cell carcinoma. A 50-year-old female presented with dull right fl ank pain and hematuria. Computed tomography indicated a 2.5 cm right renal mass as well as a 5 cm right adrenal mass. Both masses were surgically resected concurrently. Histology of the renal mass was consistent with conventional clear cell renal cell carcinoma, Fuhrman grade III. There was no extra-renal extension or lymphovascular invasion. The adrenal mass was a cortical adenoma with solid and nested patterns, with discrete zones consisting of erythroid, myeloid and megakaryocytic cells intermixed with mature adipocytes. Mitoses were inconspicuous. The solid tumour component was strongly positive for vimentin, inhibin and CD56, focally positive for low- molecular-weight cytokeratin (Cam 5.2), calretinin and CD10 (chiefl y in the myelolipomatous zones), and negative for chromogranin, S100, HMB-45, melan-A (A103), Mart-1, synaptophysin, SMA, CK7, CK20, ER, PR, TTF-1, CD99 and GCDFP (BRST-2). Ki67 (MIB1) staining indicated a low tumour proliferation index. Although well-described individually, a search of the English language literature suggests that this is the fi rst such documented case of synchrony of these three lesions. -

Preclinical Cushing's Syndrome Resulting from Adrenal Black
Endocrine Journal 2007, 54 (4), 543–551 Preclinical Cushing’s Syndrome Resulting from Adrenal Black Adenoma Diagnosed with Diabetic Ketoacidosis TOSHIO KAHARA, CHIKASHI SETO*, AKIO UCHIYAMA**, DAISUKE USUDA, HIROSHI AKAHORI, EIJI TAJIKA*, ATSUO MIWA**, RIKA USUDA, TAKASHI SUZUKI*** AND HIRONOBU SASANO*** Department of Internal Medicine, Toyama Prefectural Central Hospital, 2-2-78 Nishinagae, Toyama 930-8550, Japan *Department of Urology, Toyama Prefectural Central Hospital, 2-2-78 Nishinagae, Toyama 930-8550, Japan **Department of Pathology, Toyama Prefectural Central Hospital, 2-2-78 Nishinagae, Toyama 930-8550, Japan ***Department of Pathology, Tohoku University School of Medicine, 2-1 Seiryo-machi, Aoba-ku, Sendai 980-8575, Japan Abstract. A right adrenal tumor was incidentally discovered on abdominal computed tomography performed on a 53- year-old Japanese man, who had been hospitalized with diabetic ketoacidosis. Normal values were obtained for adrenal hormones in the morning after an overnight fast and urinary cortisol excretion after treatment of diabetic ketoacidosis with insulin. However, overnight dexamethasone administration with 1 mg or 8 mg did not completely suppress serum cortisol levels. There were no remarkable physical findings related to Cushing’s syndrome. The patient was diagnosed as having preclinical Cushing’s syndrome (PCS). Histological examination of the adrenalectomy specimen demonstrated adrenal black adenoma. Blood glucose levels subsequently improved after adrenalectomy, and the patient never developed adrenal insufficiency after hydrocortisone withdrawal. The patient was treated with diet therapy alone, and maintained good glycemic control. However, the patient still showed a diabetic pattern in an oral glucose tolerance test. It seems that the existence of PCS in addition to the underlying type 2 diabetes mellitus contributed to aggravation of blood glucose levels. -

A Case of Postpartum Hypopituitarism Accompanied by Cushing's
Endocrine Journal 2005, 52 (2), 219–222 A Case of Postpartum Hypopituitarism Accompanied by Cushing’s Syndrome as a Result of an Adrenocortical Carcinoma MEHMET SENCAN AND HATICE SEBILA DOKMETAS* Department of Hematology, Faculty of Medicine, Cumhuriyet University, 58140 Sivas, Turkey *Department of Endocrinology, Faculty of Medicine, Cumhuriyet University, 58140 Sivas, Turkey Abstract. Sheehan’s syndrome frequently causes hypopituitarism either immediately or after a delay of several years, depending on the degrees of postpartum ischemic pituitary necrosis. A 55 year-old woman whose last child was born 27 yr ago with massive hemorrhage was diagnosed as postpartum hypopituitarism. She had deficiency of growth hormone, prolactin, gonadotropins and thyrotropin. However, she interestingly had apparent hypercortisolism without suppression response to the dexamethasone tests. We found an adrenal mass with distant metastases to the liver and lung while investigating the origin of the hypercortisolism. Hyperandrogenism and very high levels of 17 hydroxyprogesterone were present. Accordingly, the patient was diagnosed as hypopituitarism due to Sheehan’s syndrome accompanied by Cushing’s syndrome as a result of an adrenocortical carcinoma. Key words: Sheehan’s syndrome, Hypopituitarism, Hypercortisolism, Adrenocortical carcinoma (Endocrine Journal 52: 219–222, 2005) SHEEHAN’S syndrome occurs as a result of ischemic with adrenocortical carcinoma may show different pituitary necrosis due to severe postpartum hemor- endocrine syndromes depending on the secretion of rhage and is characterized by various degrees of tumor; hypercortisolism and hyperandrogenism are hypopituitarism [1, 2]. Sheehan’s syndrome is a rare the most prevalent [4, 5]. postpartum complication of pregnancy with better In this report, a case with hypopituitarism due to obstetric care in developed countries. -

Comparative Genomic Hybridization Analysis of Thymic Neuroendocrine Tumors
Modern Pathology (2005) 18, 358–364 & 2005 USCAP, Inc All rights reserved 0893-3952/05 $30.00 www.modernpathology.org Comparative genomic hybridization analysis of thymic neuroendocrine tumors Chin-Chen Pan1,2, Yiin-Jeng Jong3 and Yann-Jang Chen4,5 1Department of Pathology, National Yang-Ming University, Taipei, Taiwan; 2Taipei Veterans General Hospital, Taiwan; 3Institute of Genetics, National Yang-Ming University, Taipei, Taiwan; 4Faculty of Life Sciences, National Yang-Ming University, Taipei, Taiwan and 5Department of Pediatrics, Taipei Veterans General Hospital, Taiwan Thymic neuroendocrine (carcinoid) tumors are a rare neoplasm of the anterior mediastinum. The tumors frequently exhibit a wide spectrum of histology and appear to follow a more aggressive behavior than their nonthymic counterparts. Given the differing clinicopathologic manifestations, thymic neuroendocrine tumors may also possess different cytogenetic abnormalities from those that occur in foregut carcinoid tumors. In this study, we employed comparative genomic hybridization to detect genomic instability in 10 sporadic thymic neuroendocrine tumors and one multiple endocrine neoplasia type 1 (MEN1)-associated case. Gross chromosomal imbalances were found in nine cases, including gains of chromosomal material on regions X, 8, 18 and 20p and losses on 3, 6, 9q, 13q and 11q. We did not observe deletion at locus 11q13 where the MEN1 gene is located. These findings were essentially dissimilar to those reported in sporadic and MEN1-associated foregut carcinoid tumors. Consequently,