Children's Health and the Environment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Changing Pattern of Epidemic Dropsy in North India
Epidemic Dropsy in North India N. Sharma et al. ORIGINAL ARTICLE Changing Pattern of Epidemic Dropsy in North India NAVNEET SHARMA1,*, NAINA MOHAN 2, ASHISH BHALLA1, AMAN SHARMA1, SURJIT SINGH 1 1 The Department of Internal Medicine, Postgraduate Institute of Medical Education and Research, Chandigarh, India 2 King's College London, Strand, London, United Kingdom Abstract Background: Epidemic dropsy occurs due to ingestion of mustard oil contaminated with oil from Argemone mexicana, leading to edema and tenderness of the abdomen, upper and lower limbs. In this study, clinical profiles of patients presented with epidemic dropsy in north India are described. Methods: This was a prospective study of patients presented with epidemic dropsy to the emergency department of Nehru Hospital, during the period from March 2004 to December 2011. Inclusion criteria were patients presenting with tender bilateral pitting leg edema and dermal telangiectasia. Clinical and laboratory data of patients were entered into case record forms at the time of presentation until discharge from the hospital. Results: Leg edema was the principal symptom in our series, and was in concurrence with current literature. Erythema has only been reported in 35-82% of published series, though it was present in all of our patients. Similarly, features such as diarrhea, hepatomegaly and anemia were more frequent in our cases compared to the literature. Furthermore, pancytopenia which was documented on peripheral blood counts in 54% of our cases has never been reported before. Conclusion: Epidemic dropsy should be considered in patients presenting with progressive erythema, edema, and tenderness of the limbs who had a history of consumption of mustard oil and confirmation of Argemone oil contamination according to laboratory tests. -

Epidemic Dropsy in India
Postgrad Med J 1999;75:657–661 © The Fellowship of Postgraduate Medicine, 1999 Postgrad Med J: first published as 10.1136/pgmj.75.889.657 on 1 November 1999. Downloaded from Epidemic dropsy in India B D Sharma, Sanjay Malhotra, Vikram Bhatia, Mandeep Rathee Summary Epidemic dropsy results from ingestion of edible oil adulterated with Argemone Epidemic dropsy is a clinical state mexicana (Mexican Poppy) oil. The outbreak of epidemic dropsy in the Indian resulting from use of edible oils capital, New Delhi, during the rainy season of 1998 was of one of the most severe adulterated with Argemone mexi- forms and had repercussions in both health and political circles. Some 2552 cana oil. Sanguinarine and dehyd- cases were reported and 65 deaths occurred between 5 August and 12 October, rosanguinarine are two major causing untold misery and economic loss to the aVected families. The actual fig- toxic alkaloids of Argemone oil, ures are likely to be much higher due to nonreporting of milder cases to the hos- which cause widespread capillary pitals. The aim of this article is to consolidate and update the available dilatation, proliferation and in- information on clinical aspects of epidemic dropsy. creased capillary permeability. The condition was first reported by Lyon in 1877 from Calcutta1 and has since Leakage of the protein-rich occurred in other countries including the Fiji Islands, Mauritius, Madagascar, plasma component into the extra- South Africa and Burma (Myanmar).2 In India, it has been reported from time cellular compartment leads to the to time from the States of West Bengal, Bihar, Orissa, Madhya Pradesh, Uttar formation of oedema. -

615.9Barref.Pdf
INDEX Abortifacient, abortifacients bees, wasps, and ants ginkgo, 492 aconite, 737 epinephrine, 963 ginseng, 500 barbados nut, 829 blister beetles goldenseal blister beetles, 972 cantharidin, 974 berberine, 506 blue cohosh, 395 buckeye hawthorn, 512 camphor, 407, 408 ~-escin, 884 hypericum extract, 602-603 cantharides, 974 calamus inky cap and coprine toxicity cantharidin, 974 ~-asarone, 405 coprine, 295 colocynth, 443 camphor, 409-411 ethanol, 296 common oleander, 847, 850 cascara, 416-417 isoxazole-containing mushrooms dogbane, 849-850 catechols, 682 and pantherina syndrome, mistletoe, 794 castor bean 298-302 nutmeg, 67 ricin, 719, 721 jequirity bean and abrin, oduvan, 755 colchicine, 694-896, 698 730-731 pennyroyal, 563-565 clostridium perfringens, 115 jellyfish, 1088 pine thistle, 515 comfrey and other pyrrolizidine Jimsonweed and other belladonna rue, 579 containing plants alkaloids, 779, 781 slangkop, Burke's, red, Transvaal, pyrrolizidine alkaloids, 453 jin bu huan and 857 cyanogenic foods tetrahydropalmatine, 519 tansy, 614 amygdalin, 48 kaffir lily turpentine, 667 cyanogenic glycosides, 45 lycorine,711 yarrow, 624-625 prunasin, 48 kava, 528 yellow bird-of-paradise, 749 daffodils and other emetic bulbs Laetrile", 763 yellow oleander, 854 galanthamine, 704 lavender, 534 yew, 899 dogbane family and cardenolides licorice Abrin,729-731 common oleander, 849 glycyrrhetinic acid, 540 camphor yellow oleander, 855-856 limonene, 639 cinnamomin, 409 domoic acid, 214 rna huang ricin, 409, 723, 730 ephedra alkaloids, 547 ephedra alkaloids, 548 Absorption, xvii erythrosine, 29 ephedrine, 547, 549 aloe vera, 380 garlic mayapple amatoxin-containing mushrooms S-allyl cysteine, 473 podophyllotoxin, 789 amatoxin poisoning, 273-275, gastrointestinal viruses milk thistle 279 viral gastroenteritis, 205 silibinin, 555 aspartame, 24 ginger, 485 mistletoe, 793 Medical Toxicology ofNatural Substances, by Donald G. -

The Kalinga Collection of Nazarana Coins Auction 41
The Kalinga Collection of Nazarana Coins Auction 41 10 Sep. 2015 | The Diplomat Highlight of Auction 39 63 64 133 111 90 96 97 117 78 103 110 112 138 122 125 142 166 169 Auction 41 The Kalinga Collection of Nazarana Coins (with Proof & OMS Coins) Thursday, 10th September 2015 7.00 pm onwards VIEWING Noble Room Monday 7 Sept. 2015 11:00 am - 6:00 pm The Diplomat Hotel Behind Taj Mahal Palace, Tuesday 8 Sept. 2015 11:00 am - 6:00 pm Opp. Starbucks Coffee, Wednesday 9 Sept. 2015 11:00 am - 6:00 pm Apollo Bunder At Rajgor’s SaleRoom Mumbai 400001 605 Majestic Shopping Centre, Near Church, 144 JSS Road, Opera House, Mumbai 400004 Thursday 10 Sept. 2015 3:00 pm - 6:30 pm At the Diplomat Category LOTS Coins of Mughal Empire 1-75 DELIVERY OF LOTS Coins of Independent Kingdoms 76-80 Delivery of Auction Lots will be done from the Princely States of India 81-202 Mumbai Office of the Rajgor’s. European Powers in India 203-236 BUYING AT RAJGOR’S Republic of India 237-245 For an overview of the process, see the Easy to buy at Rajgor’s Foreign Coins 246-248 CONDITIONS OF SALE Front cover: Lot 111 • Back cover: Lot 166 This auction is subject to Important Notices, Conditions of Sale and to Reserves To download the free Android App on your ONLINE CATALOGUE Android Mobile Phone, View catalogue and leave your bids online at point the QR code reader application on your www.Rajgors.com smart phone at the image on left side. -

A Short History of Occupational Disease: 2. Asbestos, Chemicals
Ulster Med J 2021;90(1):32-34 Medical History A SHORT HISTORY OF OCCUPATIONAL DISEASE: 2. ASBESTOS, CHEMICALS, RADIUM AND BEYOND Petts D, Wren MWD, Nation BR, Guthrie G, Kyle B, Peters L, Mortlock S, Clarke S, Burt C. ABSTRACT OCCUPATIONAL CANCER Historically, the weighing out and manipulation of dangerous Towards the end of the 18th century, a possible causal link chemicals frequently occurred without adequate protection between chemicals and cancer was reported by two London from inhalation or accidental ingestion. The use of gloves, surgeons. In 1761, John Hill reported an association between eye protection using goggles, masks or visors was scant. snuff, a tobacco product, and nasopharyngeal cancer, From Canary Girls and chimney sweeps to miners, stone and, in 1775, Percival Pott described a high incidence of cutters and silo fillers, these are classic exemplars of the subtle scrotal cancer in chimney sweeps. Pott, a surgeon at St (and in some cases not so subtle) effects that substances, Bartholomew’s Hospital in London, published his findings,6 environments and practices can have on individual health. which he attributed to contamination with soot. This excellent INTRODUCTION epidemiological study is considered to be the first report of a potential carcinogen. Pott’s work led to the foundation of It has been known for many centuries that certain diseases occupational medicine and to the Chimney Sweep Act of were associated with particular occupations (i.e. wool- 1788. In 1895, Ludwig Reyn reported that aromatic amines sorters disease in the textile industry, cowpox in milk maids used in certain dye industries in Germany were linked and respiratory problems in miners and stone workers). -

Contemporary Stone Beadmaking in Khambhat, India
Contemporary Stone Beadmaking in Khambhat, India: Patterns of Craft Specialization and Organization of Production as Reflected in the Archaeological Record Author(s): Jonathan Mark Kenoyer, Massimo Vidale, Kuldeep Kumar Bhan Reviewed work(s): Source: World Archaeology, Vol. 23, No. 1, Craft Production and Specialization (Jun., 1991), pp. 44-63 Published by: Taylor & Francis, Ltd. Stable URL: http://www.jstor.org/stable/124728 . Accessed: 24/01/2012 13:12 Your use of the JSTOR archive indicates your acceptance of the Terms & Conditions of Use, available at . http://www.jstor.org/page/info/about/policies/terms.jsp JSTOR is a not-for-profit service that helps scholars, researchers, and students discover, use, and build upon a wide range of content in a trusted digital archive. We use information technology and tools to increase productivity and facilitate new forms of scholarship. For more information about JSTOR, please contact [email protected]. Taylor & Francis, Ltd. is collaborating with JSTOR to digitize, preserve and extend access to World Archaeology. http://www.jstor.org Contemporarystone beadmaking in Khambhat, India: patterns of craft specialization and organization of production as reflected in the archaeologicalrecord Jonathan MarkKenoyer, Massimo Vidale and Kuldeep KumarBhan Introduction At present, the city of Khambhat in western India is one of the largest stone beadworking centers of the world, and it has been an important center for over two thousand years of documented history (Arkell 1936; Trivedi 1964) (Fig. 1). Using archaeological evidence, the stone bead industry in this region of India can be traced back even earlier to the cities and villages of the Harappan Phase of the Indus Tradition, dated to around 2500 BC (Hegde et al. -
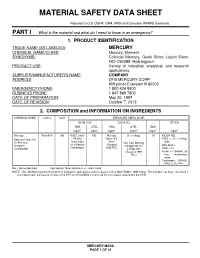
Material Safety Data Sheet
MATERIAL SAFETY DATA SHEET Prepared to U.S. OSHA, CMA, ANSI and Canadian WHMIS Standards PART I What is the material and what do I need to know in an emergency? 1. PRODUCT IDENTIFICATION TRADE NAME (AS LABELED) : MERCURY CHEMICAL NAME/CLASS : Mercury; Element SYNONYMS: Colloidal Mercury, Quick Silver; Liquid Silver; NCI-C60399; Hydrargyrum PRODUCT USE : Variety of industrial, analytical, and research applications. SUPPLIER/MANUFACTURER'S NAME : COMPANY ADDRESS : DFG MERCURY CORP 909 pitner Evanston Ill 60202 EMERGENCY PHONE : 1 800 424 9300 BUSINESS PHONE : 1 847 869 7800 DATE OF PREPARATION : May 20, 1997 DATE OF REVISION : October 7, 2013 2. COMPOSITION and INFORMATION ON INGREDIENTS CHEMICAL NAME CAS # %w/w EXPOSURE LIMITS IN AIR ACGIH-TLV OSHA-PEL OTHER TWA STEL TWA STEL IDLH mg/m 3 mg/m 3 mg/m 3 mg/m 3 mg/m 3 mg/m 3 Mercury 7439-97-6 100 0.025, (skin) NE Mercury 0.1 (ceiling) 10 NIOSH REL: Exposure limits are A4 (Not Vapor: 0.5, STEL = 0.1 (ceiling, for Mercury, Classifiable Skin; Non-alkyl Mercury skin) Inorganic as a Human (Vacated Compounds: 0.1 DFG MAKs: Compounds Carcinogen) 1989 PEL) Ceiling, skin TWA = 0.1 (Vacated 1989 PEAK = 10 •MAK 30 PEL) min., momentary value Carcinogen: EPA-D; IARC-3, TLV-A4 NE = Not Established. See Section 16 for Definitions of Terms Used. NOTE: ALL WHMIS required information is included in appropriate sections based on the ANSI Z400.1-1998 format. This product has been classified in accordance with the hazard criteria of the CPR and the MSDS contains all the information required by the CPR. -

Complete Issue (PDF)
Abstracts Eliminating Occupational Disease: areas in the country. The study studied 40 small scale industries, and collected 40 water samples (potable) for cyanide and mer- Translating Research into Action cury which are used in mining. Questionnaire-guided interviews EPICOH 2017 and work analysis covering mining practices and risk exposures were conducted, as well as chemical analysis through gas chro- 28–31 August 2017, Edinburgh, UK matography. Results of the study showed unsafe conditions in the industries such as risk of fall during erection and dismantling of scaffolds, guard rails were not provided in scaffoldings, man- Poster Presentation ual extraction of underground ores, use of explosives, poor visi- bility in looking for ores to take out to surface, exposure to Pesticides noise from explosives, and to dust from the demolished struc- tures. Mine waste was drained into soil or ground and/or rivers and streams. The most common health problems among miners 0007 ASSESSMENT OF PESTICIDE EXPOSURE AND were hypertension (62%), followed by hypertensive cardiovascu- OCCUPATIONAL SAFETY AND HEALTH OF FARMERS IN lar disease due to left wall ischemia (14%). Health symptoms THE PHILIPPINES such as dermatitis, and peripheral neuropathy were noted and Jinky Leilanie Lu. National Institutes of Health, Institute of Health Policy and Development these can be considered as manifestations of chronic cyanide poi- Studies, University of the Philippines Manila, Manila, The Philippines soning, further, aggravated by improper use of protective equip- ment. For the environmental samples of potable water, 88% and 10.1136/oemed-2017-104636.1 98% were positive with mercury and cyanide respectively. About 52% of drinking water samples exceeded the TLV for mercury Aims This is a study conducted among 534 farmers in an while 2% exceeded the TLV for cyanide. -

At Work in the World
Perspectives in Medical Humanities At Work in the World Proceedings of the Fourth International Conference on the History of Occupational and Environmental Health Edited by Paul D. Blanc, MD and Brian Dolan, PhD Page Intentionally Left Blank At Work in the World Proceedings of the Fourth International Conference on the History of Occupational and Environmental Health Perspectives in Medical Humanities Perspectives in Medical Humanities publishes scholarship produced or reviewed under the auspices of the University of California Medical Humanities Consortium, a multi-campus collaborative of faculty, students and trainees in the humanities, medi- cine, and health sciences. Our series invites scholars from the humanities and health care professions to share narratives and analysis on health, healing, and the contexts of our beliefs and practices that impact biomedical inquiry. General Editor Brian Dolan, PhD, Professor of Social Medicine and Medical Humanities, University of California, San Francisco (ucsf) Recent Monograph Titles Health Citizenship: Essays in Social Medicine and Biomedical Politics By Dorothy Porter (Fall 2011) Paths to Innovation: Discovering Recombinant DNA, Oncogenes and Prions, In One Medical School, Over One Decade By Henry Bourne (Fall 2011) The Remarkables: Endocrine Abnormalities in Art By Carol Clark and Orlo Clark (Winter 2011) Clowns and Jokers Can Heal Us: Comedy and Medicine By Albert Howard Carter iii (Winter 2011) www.medicalhumanities.ucsf.edu [email protected] This series is made possible by the generous support of the Dean of the School of Medicine at ucsf, the Center for Humanities and Health Sciences at ucsf, and a Multi-Campus Research Program grant from the University of California Office of the President. -

Mercury Study Report to Congress
United States EPA-452/R-97-007 Environmental Protection December 1997 Agency Air Mercury Study Report to Congress Volume V: Health Effects of Mercury and Mercury Compounds Office of Air Quality Planning & Standards and Office of Research and Development c7o032-1-1 MERCURY STUDY REPORT TO CONGRESS VOLUME V: HEALTH EFFECTS OF MERCURY AND MERCURY COMPOUNDS December 1997 Office of Air Quality Planning and Standards and Office of Research and Development U.S. Environmental Protection Agency TABLE OF CONTENTS Page U.S. EPA AUTHORS ............................................................... iv SCIENTIFIC PEER REVIEWERS ...................................................... v WORK GROUP AND U.S. EPA/ORD REVIEWERS ......................................viii LIST OF TABLES...................................................................ix LIST OF FIGURES ................................................................. xii LIST OF SYMBOLS, UNITS AND ACRONYMS ........................................xiii EXECUTIVE SUMMARY ......................................................... ES-1 1. INTRODUCTION ...........................................................1-1 2. TOXICOKINETICS ..........................................................2-1 2.1 Absorption ...........................................................2-1 2.1.1 Elemental Mercury ..............................................2-1 2.1.2 Inorganic Mercury ..............................................2-2 2.1.3 Methylmercury .................................................2-3 2.2 Distribution -

3.5 3.6 Rangan Metals Metalloids New Orleans
Metals/Metalloids Metals and Metalloids Cyrus Rangan MD, FAAP, ACMT Los Angeles County Department of Public Health California Poison Control System Childrens Hospital Los Angeles 1 Treatment of Metal Poisoning Old School Approaches “The treatment of acute [insert metal here]-poisoning consists in the evacuation of the stomach, if necessary, the exhibition of the sulphate of sodium or of magnesium, and the meeting of the indications as they arise. The Epsom and Glauber’s salts act as chemical antidotes, by precipitating the insoluble sulphate of [insert metal here], and also, if in excess, empty the bowel of the compound formed. To allay gastrointestinal irritation, albuminous drinks should be given and opium freely exhibited…” Wood, HC: Therapeutics Materia Medica and Toxicology, 1879 2 Treatment of Metal Poisoning Old School Approaches “If possible, the rapid administration of 2 oz. (6-7 heaping teaspoonfuls) of Magnesium sulfate (Epsom Salts) or Sodium sulfate (Glauber’s Salt) in plenty of water. Alum (aluminum potassium sulfate) will also be useful in 4 gm (60 gr.) doses (dissolved) repeated. Very dilute Sulfuric acid may be employed (30 cc of a 10 % solution diluted to 1 quart). All soluble sulfates precipitate [metal] as an insoluble sulfate…” Lucas, GW: The Symptoms and Treatment of Acute Poisoning; 1953 3 1 Metals/Metalloids Overview of Metals • Iron • Lead • Arsenic • Mercury • … a whole bunch of other ones 4 What’s a Metal? What’s a Metalloid? 5 Iron Poisoning Introduction • Essential for normal tissue and organ function • In toxic doses, iron salts (ferrous sulfate, fumarate or gluconate) cause corrosive gastrointestinal effects followed by hypotension, metabolic acidosis, and multisystem failure. -

Online Exhibition | Irwin S. Chanin School of Architecture | 2020
Online Exhibition | Irwin S. Chanin School of Architecture | 2020 Stepwells of Ahmedabad The settlement pattern of north central Gujarat evolved in response to its undulating terrain and was deeply influenced by the collection, preservation, and use of water (see Gallery 1). The travel routes that linked these settlements also followed paths charted by the seasonal movement of water across the region’s wrinkled, semi-arid landscape. The settlements formed a network tying major cities and port towns to small agricultural and artisanal villages that collectively constituted the region’s productive hinterland. The city of Ahmedabad, which emerged on the Sabarmati River, was an historic center of this network. The Sabarmati river originates in the Aravalli hills in the northeast, meanders through the gently undulating alluvial plains of north central Gujarat, and finally merges with the Arabian Sea at the Gulf of Khambhat in the south. About 50 miles north of the port city of Khambhat, Sultan Ahmad Shah, the ruler of the Gujarat Sultanate, built a citadel along the Sabarmati in 1411, formally establishing the city of Ahmedabad. The citadel was strategically situated on the river’s elevated eastern bank, anticipating the settlement’s future eastward expansion.1 Strategic elevations in the undulating terrain were identified as areas for dwelling.2 As a seasonal river, the Sabarmati swells during the monsoon and contracts in the summer, leaving dry large swathes. During its dry period, the riverbed became an expansive public space, bustling with temporary markets, circuses, and seasonal farming, as well as a variety of human activities such as washing, dyeing, and drying textiles.3 Soon after its establishment, Ahmedabad emerged as the region’s administrative capital and as an important node in the Indian Ocean trade network.