3.5 3.6 Rangan Metals Metalloids New Orleans
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharmacology/Therapeutics Ii Block 1 Handouts – 2015-16
PHARMACOLOGY/THERAPEUTICS II BLOCK 1 HANDOUTS – 2015‐16 55. H2 Blockers, PPls – Moorman 56. Palliation of Contipation & Nausea/Vomiting – Kristopaitis 57. On‐Line Only – Principles of Clinical Toxicology – Kennedy 58. Anti‐Parasitic Agents – Johnson Histamine Antagonists and PPIs January 6, 2016 Debra Hoppensteadt Moorman, Ph.D. Histamine Antagonists and PPIs Debra Hoppensteadt Moorman, Ph.D. Office # 64625 Email: [email protected] KEY CONCEPTS AND LEARNING OBJECTIVES . 1 To understand the clinical uses of H2 receptor antagonists. 2 To describe the drug interactions associated with the use of H2 receptor antagonists. 3 To understand the mechanism of action of PPIs 4 To describe the adverse effects and drugs interactions with PPIs 5 To understand when the histamine antagonists and the PPIs are to be used for treatment 6 To describe the drugs used to treat H. pylori infection Drug List: See Summary Table. Histamine Antagonists and PPIs January 6, 2016 Debra Hoppensteadt Moorman, Ph.D. Histamine Antagonists and PPIs I. H2 Receptor Antagonists These drugs reduce gastric acid secretion, and are used to treat peptic ulcer disease and gastric acid hypersecretion. These are remarkably safe drugs, and are now available over the counter. The H2 antagonists are available OTC: 1. Cimetidine (Tagamet®) 2. Famotidine (Pepcid®) 3. Nizatidine (Axid®) 4. Ranitidine (Zantac®) All of these have different structures and, therefore, different side-effects. The H2 antagonists are rapidly and well absorbed after oral administration (bioavailability 50-90%). Peak plasma concentrations are reached in 1-3 hours, and the drugs have a t1/2 of 1-3 hours. H2 antagonists also inhibit stimulated (due to feeding, gastrin, hypoglycemia, vagal) acid secretion and are useful in controlling nocturnal acidity – useful when added to proton pump therapy to control “nocturnal acid breakthrough”. -

Poisoning in Children
ARTICLE IN PRESS Current Paediatrics (2005) 15, 563–568 www.elsevier.com/locate/cupe Poisoning in children Fiona JepsenÃ, Mary Ryan Emergency Medicine, Royal Liverpool Children’s NHS Trust, Alder Hey, Liverpool L12 2AP, UK KEYWORDS Summary Poisoning accounts for about 7% of all accidents in children under 5 Poisoning; years and is implicated in about 2% of all childhood deaths in the developed world, Child; and over 5% in the developing world (National Poisons Information Service). In Accidents; considering this topic, however, it is important to differentiate accidental overdose Home (common in the younger age groups) and deliberate overdose (more common in young adults). Although initial assessment and treatment of these groups may not differ significantly, the social issues and ongoing follow-up of these children will be totally different and the treating physician must remain aware of this difference. The initial identification and treatment of these children remains the mainstay of management, and many ingested substances do not have a specific antidote. Supportive treatment must be planned and the potential for delayed or long-term effects noted. The specific presentation and treatment of some of the commonly ingested substances will be addressed in this article, and guidance given on when to contact expert help. & 2005 Elsevier Ltd. All rights reserved. Introduction such as bleaches, detergents and turpentine sub- stitutes. More than 100 000 individuals are admitted to Toxic compounds may be ingested or inhaled hospital in England and Wales annually due to either accidentally or deliberately. Accidental poisoning, accounting for 10% of all acute admis- poisoning can occur at any age, but is much more 1 sions.1 However, the true incidence of acute common in children. -

Critical Care Nursing of Infants and Children Martha A
University of Pennsylvania ScholarlyCommons Miscellaneous Papers Miscellaneous Papers 1-1-2001 Critical Care Nursing of Infants and Children Martha A. Q. Curley University of Pennsylvania, [email protected] Patricia A. Moloney-Harmon The Children's Hospital at Sinai Copyright by the author. Reprinted from Critical Care Nursing of Infants and Children, Martha A.Q. Curley and Patricia A. Moloney-Harmon (Editors), (Philadelphia: W.B. Saunders Co., 2001), 1,128 pages. NOTE: At the time of publication, the author, Martha Curley was affiliated with the Children's Hospital of Boston. Currently, she is a faculty member in the School of Nursing at the University of Pennsylvania. This paper is posted at ScholarlyCommons. http://repository.upenn.edu/miscellaneous_papers/4 For more information, please contact [email protected]. Please Note: The full version of this book and all of its chapters (below) can be found on ScholarlyCommons (from the University of Pennsylvania) at http://repository.upenn.edu/miscellaneous_papers/4/ Information page in ScholarlyCommons Full book front.pdf - Front Matter, Contributors, Forward, Preface, Acknowledgements, and Contents Chapter 1.pdf - The Essence of Pediatric Critical Care Nursing Chapter 2.pdf - Caring Practices: Providing Developmentally Supportive Care Chapter_3.pdf - Caring Practices: The Impact of the Critical Care Experience on the Family Chapter_4.pdf - Leadership in Pediatric Critical Care Chapter 5.pdf - Facilitation of Learning Chapter_6.pdf - Advocacy and Moral Agency: A Road Map for -

Chelation Therapy
Corporate Medical Policy Chelation Therapy File Name: chelation_therapy Origination: 12/1995 Last CAP Review: 2/2021 Next CAP Review: 2/2022 Last Review: 2/2021 Description of Procedure or Service Chelation therapy is an established treatment for the removal of metal toxins by converting them to a chemically inert form that can be excreted in the urine. Chelation therapy comprises intravenous or oral administration of chelating agents that remove metal ions such as lead, aluminum, mercury, arsenic, zinc, iron, copper, and calcium from the body. Specific chelating agents are used for particular heavy metal toxicities. For example, desferroxamine (not Food and Drug Administration [FDA] approved) is used for patients with iron toxicity, and calcium-ethylenediaminetetraacetic acid (EDTA) is used for patients with lead poisoning. Note that disodium-EDTA is not recommended for acute lead poisoning due to the increased risk of death from hypocalcemia. Another class of chelating agents, called metal protein attenuating compounds (MPACs), is under investigation for the treatment of Alzheimer’s disease, which is associated with the disequilibrium of cerebral metals. Unlike traditional systemic chelators that bind and remove metals from tissues systemically, MPACs have subtle effects on metal homeostasis and abnormal metal interactions. In animal models of Alzheimer’s disease, they promote the solubilization and clearance of β-amyloid protein by binding to its metal-ion complex and also inhibit redox reactions that generate neurotoxic free radicals. MPACs therefore interrupt two putative pathogenic processes of Alzheimer’s disease. However, no MPACs have received FDA approval for treating Alzheimer’s disease. Chelation therapy has also been investigated as a treatment for other indications including atherosclerosis and autism spectrum disorder. -

A Short History of Occupational Disease: 2. Asbestos, Chemicals
Ulster Med J 2021;90(1):32-34 Medical History A SHORT HISTORY OF OCCUPATIONAL DISEASE: 2. ASBESTOS, CHEMICALS, RADIUM AND BEYOND Petts D, Wren MWD, Nation BR, Guthrie G, Kyle B, Peters L, Mortlock S, Clarke S, Burt C. ABSTRACT OCCUPATIONAL CANCER Historically, the weighing out and manipulation of dangerous Towards the end of the 18th century, a possible causal link chemicals frequently occurred without adequate protection between chemicals and cancer was reported by two London from inhalation or accidental ingestion. The use of gloves, surgeons. In 1761, John Hill reported an association between eye protection using goggles, masks or visors was scant. snuff, a tobacco product, and nasopharyngeal cancer, From Canary Girls and chimney sweeps to miners, stone and, in 1775, Percival Pott described a high incidence of cutters and silo fillers, these are classic exemplars of the subtle scrotal cancer in chimney sweeps. Pott, a surgeon at St (and in some cases not so subtle) effects that substances, Bartholomew’s Hospital in London, published his findings,6 environments and practices can have on individual health. which he attributed to contamination with soot. This excellent INTRODUCTION epidemiological study is considered to be the first report of a potential carcinogen. Pott’s work led to the foundation of It has been known for many centuries that certain diseases occupational medicine and to the Chimney Sweep Act of were associated with particular occupations (i.e. wool- 1788. In 1895, Ludwig Reyn reported that aromatic amines sorters disease in the textile industry, cowpox in milk maids used in certain dye industries in Germany were linked and respiratory problems in miners and stone workers). -
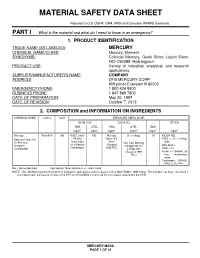
Material Safety Data Sheet
MATERIAL SAFETY DATA SHEET Prepared to U.S. OSHA, CMA, ANSI and Canadian WHMIS Standards PART I What is the material and what do I need to know in an emergency? 1. PRODUCT IDENTIFICATION TRADE NAME (AS LABELED) : MERCURY CHEMICAL NAME/CLASS : Mercury; Element SYNONYMS: Colloidal Mercury, Quick Silver; Liquid Silver; NCI-C60399; Hydrargyrum PRODUCT USE : Variety of industrial, analytical, and research applications. SUPPLIER/MANUFACTURER'S NAME : COMPANY ADDRESS : DFG MERCURY CORP 909 pitner Evanston Ill 60202 EMERGENCY PHONE : 1 800 424 9300 BUSINESS PHONE : 1 847 869 7800 DATE OF PREPARATION : May 20, 1997 DATE OF REVISION : October 7, 2013 2. COMPOSITION and INFORMATION ON INGREDIENTS CHEMICAL NAME CAS # %w/w EXPOSURE LIMITS IN AIR ACGIH-TLV OSHA-PEL OTHER TWA STEL TWA STEL IDLH mg/m 3 mg/m 3 mg/m 3 mg/m 3 mg/m 3 mg/m 3 Mercury 7439-97-6 100 0.025, (skin) NE Mercury 0.1 (ceiling) 10 NIOSH REL: Exposure limits are A4 (Not Vapor: 0.5, STEL = 0.1 (ceiling, for Mercury, Classifiable Skin; Non-alkyl Mercury skin) Inorganic as a Human (Vacated Compounds: 0.1 DFG MAKs: Compounds Carcinogen) 1989 PEL) Ceiling, skin TWA = 0.1 (Vacated 1989 PEAK = 10 •MAK 30 PEL) min., momentary value Carcinogen: EPA-D; IARC-3, TLV-A4 NE = Not Established. See Section 16 for Definitions of Terms Used. NOTE: ALL WHMIS required information is included in appropriate sections based on the ANSI Z400.1-1998 format. This product has been classified in accordance with the hazard criteria of the CPR and the MSDS contains all the information required by the CPR. -

Complete Issue (PDF)
Abstracts Eliminating Occupational Disease: areas in the country. The study studied 40 small scale industries, and collected 40 water samples (potable) for cyanide and mer- Translating Research into Action cury which are used in mining. Questionnaire-guided interviews EPICOH 2017 and work analysis covering mining practices and risk exposures were conducted, as well as chemical analysis through gas chro- 28–31 August 2017, Edinburgh, UK matography. Results of the study showed unsafe conditions in the industries such as risk of fall during erection and dismantling of scaffolds, guard rails were not provided in scaffoldings, man- Poster Presentation ual extraction of underground ores, use of explosives, poor visi- bility in looking for ores to take out to surface, exposure to Pesticides noise from explosives, and to dust from the demolished struc- tures. Mine waste was drained into soil or ground and/or rivers and streams. The most common health problems among miners 0007 ASSESSMENT OF PESTICIDE EXPOSURE AND were hypertension (62%), followed by hypertensive cardiovascu- OCCUPATIONAL SAFETY AND HEALTH OF FARMERS IN lar disease due to left wall ischemia (14%). Health symptoms THE PHILIPPINES such as dermatitis, and peripheral neuropathy were noted and Jinky Leilanie Lu. National Institutes of Health, Institute of Health Policy and Development these can be considered as manifestations of chronic cyanide poi- Studies, University of the Philippines Manila, Manila, The Philippines soning, further, aggravated by improper use of protective equip- ment. For the environmental samples of potable water, 88% and 10.1136/oemed-2017-104636.1 98% were positive with mercury and cyanide respectively. About 52% of drinking water samples exceeded the TLV for mercury Aims This is a study conducted among 534 farmers in an while 2% exceeded the TLV for cyanide. -

At Work in the World
Perspectives in Medical Humanities At Work in the World Proceedings of the Fourth International Conference on the History of Occupational and Environmental Health Edited by Paul D. Blanc, MD and Brian Dolan, PhD Page Intentionally Left Blank At Work in the World Proceedings of the Fourth International Conference on the History of Occupational and Environmental Health Perspectives in Medical Humanities Perspectives in Medical Humanities publishes scholarship produced or reviewed under the auspices of the University of California Medical Humanities Consortium, a multi-campus collaborative of faculty, students and trainees in the humanities, medi- cine, and health sciences. Our series invites scholars from the humanities and health care professions to share narratives and analysis on health, healing, and the contexts of our beliefs and practices that impact biomedical inquiry. General Editor Brian Dolan, PhD, Professor of Social Medicine and Medical Humanities, University of California, San Francisco (ucsf) Recent Monograph Titles Health Citizenship: Essays in Social Medicine and Biomedical Politics By Dorothy Porter (Fall 2011) Paths to Innovation: Discovering Recombinant DNA, Oncogenes and Prions, In One Medical School, Over One Decade By Henry Bourne (Fall 2011) The Remarkables: Endocrine Abnormalities in Art By Carol Clark and Orlo Clark (Winter 2011) Clowns and Jokers Can Heal Us: Comedy and Medicine By Albert Howard Carter iii (Winter 2011) www.medicalhumanities.ucsf.edu [email protected] This series is made possible by the generous support of the Dean of the School of Medicine at ucsf, the Center for Humanities and Health Sciences at ucsf, and a Multi-Campus Research Program grant from the University of California Office of the President. -

Mercury Study Report to Congress
United States EPA-452/R-97-007 Environmental Protection December 1997 Agency Air Mercury Study Report to Congress Volume V: Health Effects of Mercury and Mercury Compounds Office of Air Quality Planning & Standards and Office of Research and Development c7o032-1-1 MERCURY STUDY REPORT TO CONGRESS VOLUME V: HEALTH EFFECTS OF MERCURY AND MERCURY COMPOUNDS December 1997 Office of Air Quality Planning and Standards and Office of Research and Development U.S. Environmental Protection Agency TABLE OF CONTENTS Page U.S. EPA AUTHORS ............................................................... iv SCIENTIFIC PEER REVIEWERS ...................................................... v WORK GROUP AND U.S. EPA/ORD REVIEWERS ......................................viii LIST OF TABLES...................................................................ix LIST OF FIGURES ................................................................. xii LIST OF SYMBOLS, UNITS AND ACRONYMS ........................................xiii EXECUTIVE SUMMARY ......................................................... ES-1 1. INTRODUCTION ...........................................................1-1 2. TOXICOKINETICS ..........................................................2-1 2.1 Absorption ...........................................................2-1 2.1.1 Elemental Mercury ..............................................2-1 2.1.2 Inorganic Mercury ..............................................2-2 2.1.3 Methylmercury .................................................2-3 2.2 Distribution -

Sign up to Receive ATOTW Weekly – Email [email protected]
Sign up to receive ATOTW weekly – email [email protected] ACCIDENTAL POISONING IN CHILDREN ANAESTHESIA TUTORIAL OF THE WEEK 95 9TH JUNE 2008 Dr Susara Ribbens Specialist Registrar North Central London School of Anaesthetics [email protected] Introduction Poisoning is a significant global public health problem. According to the World Health Organisation data, an estimated 350 000 people died from unintentional poisoning in 2002. Accidental poisoning occurs most often in the age group 1-5 years although less than one per cent of poisoning in children is serious. More than 94% of fatal poisonings occur in low- and middle-income countries. It remains a challenge to identify those at risk at an early stage. Education of the general public and also the provision of child-proof containers for household chemicals and medicines play a key role in prevention. (Toxic plants, insect and snake bites are not discussed in this tutorial, but see www.rch.org.au/poisons for more information) Questions True or false: 1. Emesis or nasogastric aspiration are indicated after sodium hydroxide ingestion. 2. Regarding paraffin ingestion – abnormalities on the chest film may be seen in the absence of symptoms. 3. A fever after paraffin ingestion is always due to a secondary infection. 4. Ingestion of small amounts of paraquat is usually harmless. 5. High FiO2 should be avoided in paraquat ingestion to prevent pulmonary fibrosis. 6. Organophosphate forms an irreversible complex with cholinesterase. 7. Carbon monoxide is irritant with a distinctive odour. 8. The SpO2 reading in carbon monoxide poisoning is usually less than 85%. 9. A plasma paracetamol level should be taken within 2 hours of ingestion. -

The Nervous System – Target Organ Into the Twenty-First Century
The Nervous System – Target Organ into the Twenty-First Century R. Douglas Hamm MD, CCFP, FRCPC (Occ Med), FCBOM President, Canadian Board of Occupational Medicine CONTENTS 1. WHY NEURONS MAKE GOOD TARGETS FOR OCCUPATIONAL TOXICANTS 2. FROM CLASSICAL PLUMBISM TO BEHAVIORAL TOXICOLOGY 3. TOXICOKINETICS, COMPARTMENTS, AND PBPK MODELS 4. THE DIVERSE TOXICODYNAMICS OF THE NERVOUS SYSTEM 1. Peripheral Neurons (neuronopathy, axonopathy, myelinopathy) 2. Synaptic Neurotransmission (cholinergic pathways) 3. Special Senses (visual, auditory, olfactory) 4. Movement Disorders (parkinsonism, ataxia, tremor) 5. Neuroaffective and Neurocognitive Effects 5. NOTEWORTHY OCCUPATIONAL NEUROTOXICANTS 1. “Heavy metals” (Pb, Hg, Tl) and other elements (Mn, As, Al, Sb, Te) 2. Organic Solvents (toluene, xylene, styrene, C2HCl3, C2Cl4, CH3CCl3, CS2) 3. Gases (HCN, CO, H2S, ethylene oxide) 4. Pesticides (organophosphates, carbamates, organochlorines, pyrethroids, neonicotinoids) 6. CLINICAL NEUROTOXICOLOGY 1. Identification of Occupational Neurotoxic Disorders 2. Biomarkers of Exposure and Effect 3. Clinical Investigations of Neurotoxicity 1. WHY NEURONS MAKE GOOD 2. FROM CLASSICAL PLUMBISM TO TARGETS FOR OCCUPATIONAL BEHAVIORAL TOXICOLOGY TOXICANTS Hippocrates (c. 460-370 BC) has been cited as Neuroanatomical structures have large surface the first ancient author to describe a case of areas and receptor populations, e.g., the occupational neurotoxicity but this has been surface area of the brain’s 100 billion neurons shown to be erroneous (Osler, 1907; Waldron, totals hundreds of square metres. 1973, 1978; Skrabanek, 1986; Vance, 2007). The earliest report appears to be that of Neurons have high rates of metabolism, e.g., Nicander of Colophon (2nd cent. BC) who the brain at 2% body mass consumes 20% of observed that in “psimuthion” i.e. -

Evaluation of Poisoning and Drug Overdose
Evaluation of Poisoning and Drug Overdose Kara Lynch, PhD, DABCC University of California San Francisco San Francisco, CA Learning Objectives • Understand the laboratories role in the diagnosis and treatment of toxicology cases • Review the pathophysiology of toxic exposures • Identify the common toxidromes • Calculate the osmolar gap and anion gap • Be able to recognize drug overdoses Paraclesus – “father of toxicology” • “All things are poison, and nothing is without poison; only the dose permits something not to be poisonous.” • “The dose makes the poison.” • substances considered toxic are harmless in small doses, and an ordinarily harmless substance can be deadly if over-consumed Paraclesus, 1490 - 1541 Definition of “Poisoning” • A poisoning occurs when a person’s exposure to a natural or manmade substance has an undesirable effect - CDC • Poisonings can be classified as: – Self-harm or suicide – Assault or homicide – Unintentional or accidental, when no harm was intended – includes overdoses resulting from drug misuse, drug abuse or taking too much of a drug for medical reasons Monitoring Poisonings • AAPCC – American Association of Poison Control Centers – – National poison data system (NPDS) annual report • DAWN – Drug Abuse Warning Network • SAMHSA World Drug Report – Substance Abuse and Mental Health Services Administration • CDC – Center for Disease Control – National Vital Statistics System (NVSS) Poisoning / Overdose Trends Poisoning / Overdose Trends AAPCC: Top 25 human exposures AAPCC: Top 25 pediatric exposures Increase