Evaluation of Poisoning and Drug Overdose
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Methamphetamine Presentations to an Emergency Department: Management and Complications
Isoardi Katherine (Orcid ID: 0000-0002-1176-7923) Abstract Objective: There is little recent published data characterising methamphetamine intoxication. This study aims to describe the clinical effects, management, complications and disposition of patients with methamphetamine exposure. Methods: This is a retrospective review of patients presenting with methamphetamine intoxication to an Emergency Department in 2016. All presentations were extracted from a relational database and each medical record reviewed. Demographics, clinical features, complications and disposition were extracted. Results: There were 378 presentations of 329 patients (234 males [71%]), median age 31 years (range 16-68 years). The commonest clinical effect was acute behavioural disturbance, occurring in 295 (78%) presentations. This was successfully managed with oral sedation alone in 180 (61%) patients with the remainder receiving parenteral sedation. Other effects included tachycardia in 212 (56%), hypertension in 160 (42%) and hyperthermia in 17 (4%) presentations. No antihypertensives were given. One patient was actively cooled. Complications included 21 (30%) presentations with rhabdomyolysis and 43 (11%) presentations with acute kidney injury. There were two seizures, three intracranial bleeds and one myocardial infarction. The majority of This is the author manuscript accepted for publication and has undergone full peer review but has not been through the copyediting, typesetting, pagination and proofreading process, which may lead to differences between this version and the Version of Record. Please cite this article as doi: 10.1111/1742-6723.13219 This article is protected by copyright. All rights reserved. patients (310 [82%]) were managed solely within the emergency department. The median length of stay was 14 hours. There were 41(11%) mental health admissions. -

Unintentional Fentanyl Overdoses Among Persons Who Thought They
Morbidity and Mortality Weekly Report Notes from the Field Unintentional Fentanyl Overdoses Among emergency departments; 2) holding a multiagency press Persons Who Thought They Were Snorting conference; 3) conducting media interviews; 4) informing Cocaine — Fresno, California, January 7, 2019 law enforcement, prehospital providers, and the public about Patil Armenian, MD1; Jeffrey D. Whitman, MD2; Adina Badea, PhD2; naloxone distribution and use; 5) educating persons on Whitney Johnson, MD1; Chelsea Drake, MS1; Simranjit Singh Dhillon3; the proper disposal of old or new but unused medications Michelle Rivera3; Nicklaus Brandehoff, MD1; Kara L. Lynch, PhD2 through the Fresno County Department of Behavioral Health/ California Health Collaborative drop-off containers§; and On January 7, 2019, three patients arrived at the Community 6) publicizing the California Central Valley Opioid Safety Regional Medical Center emergency department in Fresno, Coalition webpage,¶ which provides information about California, after snorting (i.e., nasally insufflating) white pow- naloxone and substance use disorders. der they thought was cocaine. One (patient A) was in cardiac On January 12, 2019, a similar drug overdose incident was arrest, and two (patients B and C) had opioid toxidrome reported in Chico, California, in which postmortem toxicol- (miosis, respiratory depression, and depressed mental status) ogy testing for one person confirmed fentanyl (1). Fourteen (Table). After spontaneous circulation was reestablished in other persons at the same event were hospitalized with opioid patient A, he was admitted to the intensive care unit, where toxidrome and later released. They reported thinking they he was pronounced brain-dead 3 days later. Patients B and C were snorting cocaine,** but confirmatory toxicology results responded to naloxone, but repeated dosing was required to are unavailable. -

Pharmacology/Therapeutics Ii Block 1 Handouts – 2015-16
PHARMACOLOGY/THERAPEUTICS II BLOCK 1 HANDOUTS – 2015‐16 55. H2 Blockers, PPls – Moorman 56. Palliation of Contipation & Nausea/Vomiting – Kristopaitis 57. On‐Line Only – Principles of Clinical Toxicology – Kennedy 58. Anti‐Parasitic Agents – Johnson Histamine Antagonists and PPIs January 6, 2016 Debra Hoppensteadt Moorman, Ph.D. Histamine Antagonists and PPIs Debra Hoppensteadt Moorman, Ph.D. Office # 64625 Email: [email protected] KEY CONCEPTS AND LEARNING OBJECTIVES . 1 To understand the clinical uses of H2 receptor antagonists. 2 To describe the drug interactions associated with the use of H2 receptor antagonists. 3 To understand the mechanism of action of PPIs 4 To describe the adverse effects and drugs interactions with PPIs 5 To understand when the histamine antagonists and the PPIs are to be used for treatment 6 To describe the drugs used to treat H. pylori infection Drug List: See Summary Table. Histamine Antagonists and PPIs January 6, 2016 Debra Hoppensteadt Moorman, Ph.D. Histamine Antagonists and PPIs I. H2 Receptor Antagonists These drugs reduce gastric acid secretion, and are used to treat peptic ulcer disease and gastric acid hypersecretion. These are remarkably safe drugs, and are now available over the counter. The H2 antagonists are available OTC: 1. Cimetidine (Tagamet®) 2. Famotidine (Pepcid®) 3. Nizatidine (Axid®) 4. Ranitidine (Zantac®) All of these have different structures and, therefore, different side-effects. The H2 antagonists are rapidly and well absorbed after oral administration (bioavailability 50-90%). Peak plasma concentrations are reached in 1-3 hours, and the drugs have a t1/2 of 1-3 hours. H2 antagonists also inhibit stimulated (due to feeding, gastrin, hypoglycemia, vagal) acid secretion and are useful in controlling nocturnal acidity – useful when added to proton pump therapy to control “nocturnal acid breakthrough”. -

Approach to the Poisoned Patient
PED-1407 Chocolate to Crystal Methamphetamine to the Cinnamon Challenge - Emergency Approach to the Intoxicated Child BLS 08 / ALS 75 / 1.5 CEU Target Audience: All Pediatric and adolescent ingestions are common reasons for 911 dispatches and emergency department visits. With greater availability of medications and drugs, healthcare professionals need to stay sharp on current trends in medical toxicology. This lecture examines mind altering substances, initial prehospital approach to toxicology and stabilization for transport, poison control center resources, and ultimate emergency department and intensive care management. Pediatric Toxicology Dr. James Burhop Pediatric Emergency Medicine Children’s Hospital of the Kings Daughters Objectives • Epidemiology • History of Poisoning • Review initial assessment of the child with a possible ingestion • General management principles for toxic exposures • Case Based (12 common pediatric cases) • Emerging drugs of abuse • Cathinones, Synthetics, Salvia, Maxy/MCAT, 25I, Kratom Epidemiology • 55 Poison Centers serving 295 million people • 2.3 million exposures in 2011 – 39% are children younger than 3 years – 52% in children younger than 6 years • 1-800-222-1222 2011 Annual report of the American Association of Poison Control Centers Toxic Exposure Surveillance System Introduction • 95% decline in the number of pediatric poisoning deaths since 1960 – child resistant packaging – heightened parental awareness – more sophisticated interventions – poison control centers Epidemiology • Unintentional (1-2 -

Poisoning in Children
ARTICLE IN PRESS Current Paediatrics (2005) 15, 563–568 www.elsevier.com/locate/cupe Poisoning in children Fiona JepsenÃ, Mary Ryan Emergency Medicine, Royal Liverpool Children’s NHS Trust, Alder Hey, Liverpool L12 2AP, UK KEYWORDS Summary Poisoning accounts for about 7% of all accidents in children under 5 Poisoning; years and is implicated in about 2% of all childhood deaths in the developed world, Child; and over 5% in the developing world (National Poisons Information Service). In Accidents; considering this topic, however, it is important to differentiate accidental overdose Home (common in the younger age groups) and deliberate overdose (more common in young adults). Although initial assessment and treatment of these groups may not differ significantly, the social issues and ongoing follow-up of these children will be totally different and the treating physician must remain aware of this difference. The initial identification and treatment of these children remains the mainstay of management, and many ingested substances do not have a specific antidote. Supportive treatment must be planned and the potential for delayed or long-term effects noted. The specific presentation and treatment of some of the commonly ingested substances will be addressed in this article, and guidance given on when to contact expert help. & 2005 Elsevier Ltd. All rights reserved. Introduction such as bleaches, detergents and turpentine sub- stitutes. More than 100 000 individuals are admitted to Toxic compounds may be ingested or inhaled hospital in England and Wales annually due to either accidentally or deliberately. Accidental poisoning, accounting for 10% of all acute admis- poisoning can occur at any age, but is much more 1 sions.1 However, the true incidence of acute common in children. -

Guideline on Antidote Availability for Emergency Departments January 2017
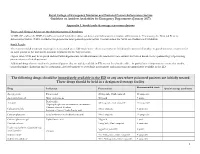
Royal College of Emergency Medicine and National Poisons Information Service Guideline on Antidote Availability for Emergency Departments January 2017 TOXBASE and/or the BNF should be consulted for further advice on doses and indications for antidote administration and, if necessary, the National Poisons Information Service (NPIS) should be telephoned for more patient-specific advice. Contact details for NPIS are available on TOXBASE. Additional drugs that are used in the poisoned patient that are widely available in ED are not listed in the table – in particular it is important to ensure that insulin, benzodiazepines (diazepam and/or lorazepam), glyceryl trinitrate or isosorbide dinitrate and magnesium are immediately available in the ED. The following drugs should be immediately available in the ED or any area where poisoned patients are initially treated. These drugs should be held in a designated storage facility* The stock held should be sufficient to initiate treatment (stocking guidance is in Appendix 1). Drug Indication Acetylcysteine Paracetamol Activated charcoal Many oral poisons Atropine Organophosphorus or carbamate insecticides Bradycardia Calcium chloride Calcium channel blockers Systemic effects of hydrofluoric acid Calcium gluconate Local infiltration for hydrofluoric acid Calcium gluconate gel Hydrofluoric acid Cyanide antidotes Cyanide Dicobalt edetate The choice of antidote depends on the severity of poisoning, certainty of diagnosis and cause Hydroxocobalamin (Cyanokit®) of poisoning/source of cyanide. Sodium nitrite - Dicobalt edetate is the antidote of choice in severe cases when there is a high clinical Sodium thiosulphate suspicion of cyanide poisoning e.g. after cyanide salt exposure. - Hydroxocobalamin (Cyanokit®) should be considered in smoke inhalation victims who have a severe lactic acidosis, are comatose, in cardiac arrest or have significant cardiovascular compromise - Sodium nitrite may be used if dicobalt edetate is not available. -

Pre-Hospital Use and Administration of Naloxone
Opioid Toxicity and Naloxone: Implications for the K-12 Population Elizabeth J. Scharman, Pharm.D., DABAT, FAACT, BCPS Director, West Virginia Poison Center Professor, WVU School of Pharmacy Outline • Definitions • Patterns of opioid exposure grades K-12 • Opioid Toxicology I. Opioid toxidrome II. Pharmacologic differences: effect on toxicity III. Designer opioids: what this means for WV • Naloxone I. Mechanism details II. Potential adverse effects III. Meaning of “response” to naloxone Definitions • Opioid – A drug that works by binding to the opioid receptors • Opioid receptors are where the body’s “natural” painkillers (endorphins for example) attach to decrease the perception of pain – Examples: morphine, hydrocodone, heroin, oxycodone • Naloxone – Opioid antidote • Competitively takes the place of the opioid on the opioid receptor 1 Young Opioid Abusers • Survey of 50 injection drug users 16-25 years – Hydrocodone/acetaminophen, oxycodone, oxycodone/acetaminophen most common initial opioid drugs misused • Average age first use = 14.5 years • Obtained from family member, their own Rx, friend/contact • Oral = 41, Sniffing/snorting = 8, Injecting = 1 – Followed initial use of alcohol (avg 12.8 years of age), marijuana (avg 12.5 years of age), Rx stimulants (avg 14.1 years of age) • Opioid misuse prior to heroin (n = 43) – Average age of first use = 16.1 years WV Poison Center Data 2014 2015 ≤ 5 years 6 – 19 years ≤ 5 years 6 – 19 years Heroin 1201 Single Opioid 59 30 64 21 Comb. Opioid 18 41 21 27 Acetaminophen 83 88 Non-steroidal 120 -

The Anticholinergic Toxidrome
Poison HOTLINE Partnership between Iowa Health System and University of Iowa Hospitals and Clinics July 2011 The Anticholinergic Toxidrome A toxidrome is a group of symptoms associated with poisoning by a particular class of agents. One example is the opiate toxidrome, the triad of CNS depression, respiratory depression, and pinpoint pupils, and which usually responds to naloxone. The anticholinergic toxidrome is most frequently associated with overdoses of diphenhydramine, a very common OTC medication. However, many drugs and plants can produce the anticholinergic toxidrome. A partial list includes: tricyclic antidepressants (amitriptyline), older antihistamines (chlorpheniramine), Did you know …… phenothiazines (promethazine) and plants containing the anticholinergic alkaloids atropine, hyoscyamine and scopolamine (Jimson Weed). Each summer, the ISPCC receives approximately 10-20 The mnemonic used to help remember the symptoms and signs of this snake bite calls, some being toxidrome are derived from the Alice in Wonderland story: from poisonous snakes (both Blind as a Bat (mydriasis and inability to focus on near objects) local and exotic). Red as a Beet (flushed skin color) Four poisonous snakes can be Hot as Hades (elevated temperature) found in Iowa: the prairie These patients can sometimes die of agitation-induced hyperthermia. rattlesnake, the massasauga, Dry as a Bone (dry mouth and dry skin) the copperhead, and the Mad as a Hatter (hallucinations and delirium) timber rattlesnake. Each Bowel and bladder lose their tone (urinary retention and constipation) snake has specific territories Heart races on alone (tachycardia) within the state. ISPCC A patient who has ingested only an anticholinergic substance and is not specialists have access to tachycardic argues against a serious anticholinergic overdose. -
RCEM NPIS Antidote Guideline Appx 1
Royal College of Emergency Medicine and National Poisons Information Service Guideline on Antidote Availability for Emergency Departments (January 2017) Appendix 1. Stock levels & storage recommendations Doses and Clinical Advice on the Administration of Antidotes TOXBASE and/or the BNF should be consulted for further advice on doses and indications for antidote administration. If necessary, the National Poisons Information Service (NPIS) should be telephoned for more patient-specific advice. Contact details for NPIS are available on TOXBASE. Stock Levels The recommended minimum stocking levels (rounded up to full “pack-sizes” where necessary) are based on the amount of antidote required to initiate treatment for an adult patient in the ED and to continue treatment for the first 24 hours. Higher stock levels may be required and individual departments should determine the amount of each antidote they stock based on the epidemiology of poisoning presentations to their department. Additional drugs that are used in the poisoned patient that are widely available in ED are not listed in the table – in particular it is important to ensure that insulin, benzodiazepines (diazepam and/or lorazepam), glyceryl trinitrate or isosorbide mononitrate and magnesium are immediately available in the ED. The following drugs should be immediately available in the ED or any area where poisoned patients are initially treated These drugs should be held in a designated storage facility Recommended stock Drug Indication Presentation Special storage conditions -

Critical Care Nursing of Infants and Children Martha A
University of Pennsylvania ScholarlyCommons Miscellaneous Papers Miscellaneous Papers 1-1-2001 Critical Care Nursing of Infants and Children Martha A. Q. Curley University of Pennsylvania, [email protected] Patricia A. Moloney-Harmon The Children's Hospital at Sinai Copyright by the author. Reprinted from Critical Care Nursing of Infants and Children, Martha A.Q. Curley and Patricia A. Moloney-Harmon (Editors), (Philadelphia: W.B. Saunders Co., 2001), 1,128 pages. NOTE: At the time of publication, the author, Martha Curley was affiliated with the Children's Hospital of Boston. Currently, she is a faculty member in the School of Nursing at the University of Pennsylvania. This paper is posted at ScholarlyCommons. http://repository.upenn.edu/miscellaneous_papers/4 For more information, please contact [email protected]. Please Note: The full version of this book and all of its chapters (below) can be found on ScholarlyCommons (from the University of Pennsylvania) at http://repository.upenn.edu/miscellaneous_papers/4/ Information page in ScholarlyCommons Full book front.pdf - Front Matter, Contributors, Forward, Preface, Acknowledgements, and Contents Chapter 1.pdf - The Essence of Pediatric Critical Care Nursing Chapter 2.pdf - Caring Practices: Providing Developmentally Supportive Care Chapter_3.pdf - Caring Practices: The Impact of the Critical Care Experience on the Family Chapter_4.pdf - Leadership in Pediatric Critical Care Chapter 5.pdf - Facilitation of Learning Chapter_6.pdf - Advocacy and Moral Agency: A Road Map for -

Chelation Therapy
Corporate Medical Policy Chelation Therapy File Name: chelation_therapy Origination: 12/1995 Last CAP Review: 2/2021 Next CAP Review: 2/2022 Last Review: 2/2021 Description of Procedure or Service Chelation therapy is an established treatment for the removal of metal toxins by converting them to a chemically inert form that can be excreted in the urine. Chelation therapy comprises intravenous or oral administration of chelating agents that remove metal ions such as lead, aluminum, mercury, arsenic, zinc, iron, copper, and calcium from the body. Specific chelating agents are used for particular heavy metal toxicities. For example, desferroxamine (not Food and Drug Administration [FDA] approved) is used for patients with iron toxicity, and calcium-ethylenediaminetetraacetic acid (EDTA) is used for patients with lead poisoning. Note that disodium-EDTA is not recommended for acute lead poisoning due to the increased risk of death from hypocalcemia. Another class of chelating agents, called metal protein attenuating compounds (MPACs), is under investigation for the treatment of Alzheimer’s disease, which is associated with the disequilibrium of cerebral metals. Unlike traditional systemic chelators that bind and remove metals from tissues systemically, MPACs have subtle effects on metal homeostasis and abnormal metal interactions. In animal models of Alzheimer’s disease, they promote the solubilization and clearance of β-amyloid protein by binding to its metal-ion complex and also inhibit redox reactions that generate neurotoxic free radicals. MPACs therefore interrupt two putative pathogenic processes of Alzheimer’s disease. However, no MPACs have received FDA approval for treating Alzheimer’s disease. Chelation therapy has also been investigated as a treatment for other indications including atherosclerosis and autism spectrum disorder. -

Fomepizole for Acetaminophen Toxicity
Clinical Pharmacology & Toxicology Pearl of the Week Fomepizole for Acetaminophen Toxicity Mechanisms There are two ways that fomepizole works to help prevent hepatotoxicity in APAP overdose. The primary mechanism involves inhibition of CYP450 2E1. o When a toxic amount of APAP is ingested, the pathways that convert it into nontoxic metabolites become overwhelmed. o Thus, more APAP gets converted into NAPQI. o Fomepizole inhibits the 2E1 pathway, thus preventing conversion of APAP into NAPQI. The second mechanism of action is the JNK (“junk”) enzyme. o NAPQI-induced mitochondrial dysfunction leads to formation of reactive oxidant species. This oxidant stress leads to activation of c-jun N-terminal kinase, or JNK, enzyme. o This enzyme translocates to the mitochondria, amplifying oxidant stress, and ultimately resulting in the cessation of ATP production. o Additionally, the JNK enzyme can lead to the rupture of the outer mitochondrial membrane, causing release of intermembrane proteins, which can potentially lead to DNA fragmentation o Interestingly, it is thought that both metabolic acidosis, as well as elevated lactate levels, may be the result of alterations in mitochondrial respiratory function o Fomepizole works by preventing the APAP-induced activation of this enzyme. Role in Acetaminophen poisoning management In cases where fomepizole and NAC were administered together, evidence has shown that the combination has contributed to a decrease in both hepatotoxicity and mortality. Most of the evidence has come from case reports and animal models. Currently, fomepizole is recommended for massive APAP ingestions (as in, ingestions over 500- 600 mg/kg or in cases where 4-hour equivalent acetaminophen concentrations over 5000 umol/L).