Guideline on Antidote Availability for Emergency Departments January 2017
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
RCEM NPIS Antidote Guideline Appx 1
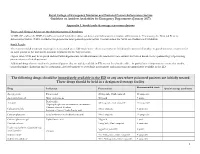
Royal College of Emergency Medicine and National Poisons Information Service Guideline on Antidote Availability for Emergency Departments (January 2017) Appendix 1. Stock levels & storage recommendations Doses and Clinical Advice on the Administration of Antidotes TOXBASE and/or the BNF should be consulted for further advice on doses and indications for antidote administration. If necessary, the National Poisons Information Service (NPIS) should be telephoned for more patient-specific advice. Contact details for NPIS are available on TOXBASE. Stock Levels The recommended minimum stocking levels (rounded up to full “pack-sizes” where necessary) are based on the amount of antidote required to initiate treatment for an adult patient in the ED and to continue treatment for the first 24 hours. Higher stock levels may be required and individual departments should determine the amount of each antidote they stock based on the epidemiology of poisoning presentations to their department. Additional drugs that are used in the poisoned patient that are widely available in ED are not listed in the table – in particular it is important to ensure that insulin, benzodiazepines (diazepam and/or lorazepam), glyceryl trinitrate or isosorbide mononitrate and magnesium are immediately available in the ED. The following drugs should be immediately available in the ED or any area where poisoned patients are initially treated These drugs should be held in a designated storage facility Recommended stock Drug Indication Presentation Special storage conditions -

Fomepizole for Acetaminophen Toxicity
Clinical Pharmacology & Toxicology Pearl of the Week Fomepizole for Acetaminophen Toxicity Mechanisms There are two ways that fomepizole works to help prevent hepatotoxicity in APAP overdose. The primary mechanism involves inhibition of CYP450 2E1. o When a toxic amount of APAP is ingested, the pathways that convert it into nontoxic metabolites become overwhelmed. o Thus, more APAP gets converted into NAPQI. o Fomepizole inhibits the 2E1 pathway, thus preventing conversion of APAP into NAPQI. The second mechanism of action is the JNK (“junk”) enzyme. o NAPQI-induced mitochondrial dysfunction leads to formation of reactive oxidant species. This oxidant stress leads to activation of c-jun N-terminal kinase, or JNK, enzyme. o This enzyme translocates to the mitochondria, amplifying oxidant stress, and ultimately resulting in the cessation of ATP production. o Additionally, the JNK enzyme can lead to the rupture of the outer mitochondrial membrane, causing release of intermembrane proteins, which can potentially lead to DNA fragmentation o Interestingly, it is thought that both metabolic acidosis, as well as elevated lactate levels, may be the result of alterations in mitochondrial respiratory function o Fomepizole works by preventing the APAP-induced activation of this enzyme. Role in Acetaminophen poisoning management In cases where fomepizole and NAC were administered together, evidence has shown that the combination has contributed to a decrease in both hepatotoxicity and mortality. Most of the evidence has come from case reports and animal models. Currently, fomepizole is recommended for massive APAP ingestions (as in, ingestions over 500- 600 mg/kg or in cases where 4-hour equivalent acetaminophen concentrations over 5000 umol/L). -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

'Tis the Season for Antifreeze…And Its Toxicities!
VETTALK Volume 15, Number 02 American College of Veterinary Pharmacists ‘Tis the Season for Antifreeze…and its Toxicities! Introduction outcomes. As with ethanol and methanol, resembles ethanol (alcohol) intoxication. Antifreeze is known to most as the EG is also metabolized by ADH to form Dogs and cats exhibit vomiting due to GI neon green liquid that goes into our cars glycoaldehyde which is then oxidized to irritation, polydipsia, polyuria, and neu- to lower the freezing point and prevent glycolate, glyoxalate, and oxalate. Gly- rologic signs such as CNS depression, our radiators from locking up in cold colate and oxalate are responsible for stupor, ataxia, knuckling, decreased with- weather. However, to veterinarians and metabolic acidosis and renal damage. drawal or righting reflexes. Polydipsia veterinary pharmacists, it is ethylene gly- This is because ethylene glycol metabo- occurs due to osmotic stimulation of the col, a source of tens of thousands of ani- lites target the kidney and lead to oliguric thirst center, and polyuria occurs due to mal poisonings each year, the majority of or anuric acute renal injury, which in turn an osmotic diuresis. As CNS depression which occur in late fall, winter, and early slows elimination of ethylene glycol mak- increases in severity, dogs and cats drink spring which is why the timing appeared ing toxicity worst. The process of renal less, however the osmotic diuresis contin- suitable for this newsletter. The other failure is primarily due to glycolate- ues and results in severe dehydration. reason for publishing this article now is induced direct damage to tubules, al- Dogs may appear to transiently recover that the antidote for antifreeze poisoning, though tubule obstruction from precipi- from these CNS signs approximately 12 Antizol-Vet®(fomepizole), is on indefi- tated oxalate crystals may contribute as hours after ingestion. -

World Health Organization Model List of Essential Medicines, 21St List, 2019
World Health Organizatio n Model List of Essential Medicines 21st List 2019 World Health Organizatio n Model List of Essential Medicines 21st List 2019 WHO/MVP/EMP/IAU/2019.06 © World Health Organization 2019 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. World Health Organization Model List of Essential Medicines, 21st List, 2019. Geneva: World Health Organization; 2019. Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. CIP data are available at http://apps.who.int/iris. -

Evaluation of Poisoning and Drug Overdose
Evaluation of Poisoning and Drug Overdose Kara Lynch, PhD, DABCC University of California San Francisco San Francisco, CA Learning Objectives • Understand the laboratories role in the diagnosis and treatment of toxicology cases • Review the pathophysiology of toxic exposures • Identify the common toxidromes • Calculate the osmolar gap and anion gap • Be able to recognize drug overdoses Paraclesus – “father of toxicology” • “All things are poison, and nothing is without poison; only the dose permits something not to be poisonous.” • “The dose makes the poison.” • substances considered toxic are harmless in small doses, and an ordinarily harmless substance can be deadly if over-consumed Paraclesus, 1490 - 1541 Definition of “Poisoning” • A poisoning occurs when a person’s exposure to a natural or manmade substance has an undesirable effect - CDC • Poisonings can be classified as: – Self-harm or suicide – Assault or homicide – Unintentional or accidental, when no harm was intended – includes overdoses resulting from drug misuse, drug abuse or taking too much of a drug for medical reasons Monitoring Poisonings • AAPCC – American Association of Poison Control Centers – – National poison data system (NPDS) annual report • DAWN – Drug Abuse Warning Network • SAMHSA World Drug Report – Substance Abuse and Mental Health Services Administration • CDC – Center for Disease Control – National Vital Statistics System (NVSS) Poisoning / Overdose Trends Poisoning / Overdose Trends AAPCC: Top 25 human exposures AAPCC: Top 25 pediatric exposures Increase -

Poison Control Antidote Poster
Antidote Chart (The suggested minimum stocking level is a combination of factors; anticipation of the highest total dose of a drug generally given during a 24 hour period to a 70 kg adult.) General Decontamination Uses Dose Comments Activated Charcoal (without sorbitol) Most ingestions occurring within one hour Adults: 25–100 grams, Children: 1 g/kg May be given in multiple doses depending on ingestant to enhance elimination Activated Charcoal (with sorbitol) May be used as first AC given to patient if presents within Adults: 25–50 grams Should not be used for multiple dose activated charcoal regimens one hour of ingestion Children: Not generally recommended Whole Bowel Irrigation Drugs not bound by charcoal, sustained Adults: 500–2000 ml/hour Nasogastric tube should be used to maintain amount given (Polyethylene Glycol) release formulations, and body stuffers Children: 25 ml/kg/hour Syrup of Ipecac No longer recommended No longer recommended No longer recommended Poisoning Antidote Quantity to Stock* Comments Acetaminophen N-ACETYLYCYSTEINE 10–20% 600 ml (20% Mucomyst®) Because vomiting of the oral NAC is common, the facility should maintain a repeat dose (Mucomyst®) or 1200 ml (10% Mucomyst®) for each patient for initial dosing if continuation of treatment at facility is not anticipated. ACETADOTE® The IV Acetadote® was just approved in February 2004. Call the MAPCC for dosing, ACETYLCYSTEINE Injection for IV use 4 (30 ml) vials of 20% solution precautions and contraindications. Both the oral and IV forms of acetylcysteine should be administered within 8 hours for maximal protection against hepatic injury. Anticholinergic Poisoning PHYSOSTIGMINE (Antilirium®) 2–4 mg* Not generally recommended for children. -

Drug Consumption at Wholesale Prices in 2017 - 2020
Page 1 Drug consumption at wholesale prices in 2017 - 2020 2020 2019 2018 2017 Wholesale Hospit. Wholesale Hospit. Wholesale Hospit. Wholesale Hospit. ATC code Subgroup or chemical substance price/1000 € % price/1000 € % price/1000 € % price/1000 € % A ALIMENTARY TRACT AND METABOLISM 321 590 7 309 580 7 300 278 7 295 060 8 A01 STOMATOLOGICAL PREPARATIONS 2 090 9 1 937 7 1 910 7 2 128 8 A01A STOMATOLOGICAL PREPARATIONS 2 090 9 1 937 7 1 910 7 2 128 8 A01AA Caries prophylactic agents 663 8 611 11 619 12 1 042 11 A01AA01 sodium fluoride 610 8 557 12 498 15 787 14 A01AA03 olaflur 53 1 54 1 50 1 48 1 A01AA51 sodium fluoride, combinations - - - - 71 1 206 1 A01AB Antiinfectives for local oral treatment 1 266 10 1 101 6 1 052 6 944 6 A01AB03 chlorhexidine 930 6 885 7 825 7 706 7 A01AB11 various 335 21 216 0 227 0 238 0 A01AB22 doxycycline - - 0 100 0 100 - - A01AC Corticosteroids for local oral treatment 113 1 153 1 135 1 143 1 A01AC01 triamcinolone 113 1 153 1 135 1 143 1 A01AD Other agents for local oral treatment 49 0 72 0 104 0 - - A01AD02 benzydamine 49 0 72 0 104 0 - - A02 DRUGS FOR ACID RELATED DISORDERS 30 885 4 32 677 4 35 102 5 37 644 7 A02A ANTACIDS 3 681 1 3 565 1 3 357 1 3 385 1 A02AA Magnesium compounds 141 22 151 22 172 22 155 19 A02AA04 magnesium hydroxide 141 22 151 22 172 22 155 19 A02AD Combinations and complexes of aluminium, 3 539 0 3 414 0 3 185 0 3 231 0 calcium and magnesium compounds A02AD01 ordinary salt combinations 3 539 0 3 414 0 3 185 0 3 231 0 A02B DRUGS FOR PEPTIC ULCER AND 27 205 5 29 112 4 31 746 5 34 258 8 -

The Effect of 4-Methylpyrazole on Oxidative Metabolism of Acetaminophen in Human Volunteers
Journal of Medical Toxicology (2020) 16:169–176 https://doi.org/10.1007/s13181-019-00740-z ORIGINAL ARTICLE The Effect of 4-Methylpyrazole on Oxidative Metabolism of Acetaminophen in Human Volunteers A. Min Kang1,2 & Angela Padilla-Jones2 & Erik S. Fisher2 & Jephte Y. Akakpo3 & Hartmut Jaeschke3 & Barry H. Rumack4 & Richard D. Gerkin2 & Steven C. Curry1,2 Received: 12 July 2019 /Revised: 12 September 2019 /Accepted: 15 September 2019 /Published online: 25 November 2019 # American College of Medical Toxicology 2019 Abstract Introduction Acetaminophen (APAP) is commonly ingested in both accidental and suicidal overdose. Oxidative metabolism by cytochrome P450 2E1 (CYP2E1) produces the hepatotoxic metabolite, N-acetyl-p-benzoquinone imine. CYP2E1 inhibition using 4-methylpyrazole (4-MP) has been shown to prevent APAP-induced liver injury in mice and human hepatocytes. This study was conducted to assess the effect of 4-MP on APAP metabolism in humans. Methods This crossover trial examined the ability of 4-MP to inhibit CYP2E1 metabolism of APAP in five human volunteers. Participants received a single oral dose of APAP 80 mg/kg, both with and without intravenous 4-MP, after which urinary and plasma oxidative APAP metabolites were measured. The primary outcome was the fraction of ingested APAP excreted as total oxidative metabolites (APAP-CYS, APAP-NAC, APAP-GSH). Results Compared with APAP alone, co-treatment with 4-MP decreased the percentage of ingested APAP recovered as oxidative metabolites in 24-hour urine from 4.48 to 0.51% (95% CI = 2.31–5.63%, p = 0.003). Plasma concentrations of these oxidative metabolites also decreased. -

Estonian Statistics on Medicines 2013 1/44
Estonian Statistics on Medicines 2013 DDD/1000/ ATC code ATC group / INN (rout of admin.) Quantity sold Unit DDD Unit day A ALIMENTARY TRACT AND METABOLISM 146,8152 A01 STOMATOLOGICAL PREPARATIONS 0,0760 A01A STOMATOLOGICAL PREPARATIONS 0,0760 A01AB Antiinfectives and antiseptics for local oral treatment 0,0760 A01AB09 Miconazole(O) 7139,2 g 0,2 g 0,0760 A01AB12 Hexetidine(O) 1541120 ml A01AB81 Neomycin+Benzocaine(C) 23900 pieces A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+Thymol(dental) 2639 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+Cetylpyridinium chloride(gingival) 179340 g A01AD81 Lidocaine+Cetrimide(O) 23565 g A01AD82 Choline salicylate(O) 824240 pieces A01AD83 Lidocaine+Chamomille extract(O) 317140 g A01AD86 Lidocaine+Eugenol(gingival) 1128 g A02 DRUGS FOR ACID RELATED DISORDERS 35,6598 A02A ANTACIDS 0,9596 Combinations and complexes of aluminium, calcium and A02AD 0,9596 magnesium compounds A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 591680 pieces 10 pieces 0,1261 A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 1998558 ml 50 ml 0,0852 A02AD82 Aluminium aminoacetate+Magnesium oxide(O) 463540 pieces 10 pieces 0,0988 A02AD83 Calcium carbonate+Magnesium carbonate(O) 3049560 pieces 10 pieces 0,6497 A02AF Antacids with antiflatulents Aluminium hydroxide+Magnesium A02AF80 1000790 ml hydroxide+Simeticone(O) DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 34,7001 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 3,5364 A02BA02 Ranitidine(O) 494352,3 g 0,3 g 3,5106 A02BA02 Ranitidine(P) -

Fomepizole (Antizol®)
ToxTidbits: Antidote Facts 1-800-222-1222 ® Fomepizole (Antizol ) Ethylene glycol (EG) and methanol are toxic alcohols that are responsible for thousands of human poisonings each year. Both are found in automotive products including antifreeze (EG) and windshield wiper fluid (methanol). Mechanism/Indications: Fomepizole is FDA approved for the treatment of methanol and EG poisoning. Fomepizole is an alcohol dehydrogenase inhibitor that works as an antidote by preventing formation of the toxic metabolites of EG and methanol. It can be used alone or in combination with hemodialysis. Indications for administering fomepizole are: • ≥ 0.2 mL/kg of 100% EG or ≥ 0.1 mL/kg of 100% methanol was ingested OR • Unknown amount was ingested and one of the following: - Serum EG or methanol concentration > 20 mg/dL (200 mcg/mL) - Presence of CNS depression - Metabolic acidosis with anion gap > 15 - Osmol gap > 20 (accounting for ethanol and other osmotically active substances) - End organ damage (e.g. eyes for methanol and kidneys for EG) Dosing: The dosing and administration of fomepizole is the same for children and adults. • Loading dose: 15 mg/kg IV; maximum of 1500 mg • 12 hours later, give the 1st maintenance dose of 10 mg/kg IV. Repeat every 12 hours x 4 doses. • Fomepizole induces its own metabolism, so after the fourth 10 mg/kg dose, increase the dose to 15 mg/kg IV every 12 hours. • Continue treatment until EG or methanol levels are below 20 mg/dL and the patient is asymptomatic with normal osmol gap AND normal pH. Fomepizole is available in 1.5 ml vials. -

New Zealand Data Sheet
NEW ZEALAND DATA SHEET 1. PRODUCT NAME ANTIZOL® Fomepizole 1g/mL concentrate for injection 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each vial contains 1.5 g of fomepizole. Excipient with known effect: none. For a full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Clear to yellow liquid at room temperature. Its melting point is 25 oC and it may present as a solid at room temperature. 4. CLINICAL PARTICULARS 4.1. Therapeutic Indications Antizol® (fomepizole) is indicated for the treatment of ethylene glycol or methanol poisoning. 4.2. Dose and method of administration CAUTION: MUST BE DILUTED PRIOR TO USE Treatment Guidelines: If ethylene glycol or methanol poisoning is left untreated, the natural progression of the poisoning leads to accumulation of toxic metabolites, including glycolic and oxalic acids (ethylene glycol intoxication) and formic acid (methanol intoxication). These metabolites can induce metabolic acidosis, nausea/vomiting, seizures, stupor, coma, calcium oxaluria, acute tubular necrosis, blindness and death. The diagnosis of these poisonings may be difficult because ethylene glycol and methanol concentrations diminish in the blood as they are metabolized to their respective metabolites. Antizol® solidifies at temperatures less than 25 °C hence, if the fomepizole solution has become solid in the vial, the solution should be liquefied by running the vial under warm tap water or by holding in the hand. Solidification does not affect the stability of Antizol®. Using sterile technique, the appropriate dose of fomepizole should be drawn from the vial with a syringe and injected into at least 100 mL of sterile 0.9% sodium chloride injection or dextrose 5% injection.