Poison Control Antidote Poster
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mapping the Dissociated Body
Lesley University DigitalCommons@Lesley Graduate School of Arts and Social Sciences Expressive Therapies Capstone Theses (GSASS) Spring 5-16-2020 Mapping the Dissociated Body Elizabeth Hough [email protected] Follow this and additional works at: https://digitalcommons.lesley.edu/expressive_theses Part of the Social and Behavioral Sciences Commons Recommended Citation Hough, Elizabeth, "Mapping the Dissociated Body" (2020). Expressive Therapies Capstone Theses. 239. https://digitalcommons.lesley.edu/expressive_theses/239 This Thesis is brought to you for free and open access by the Graduate School of Arts and Social Sciences (GSASS) at DigitalCommons@Lesley. It has been accepted for inclusion in Expressive Therapies Capstone Theses by an authorized administrator of DigitalCommons@Lesley. For more information, please contact [email protected], [email protected]. Running Head: MAPPING THE DISSOCIATED BODY 1 Mapping the Dissociated Body Elizabeth Hough Lesley University Running Head: MAPPING THE DISSOCIATED BODY 2 Abstract This capstone thesis explored the use of body mapping and body scans as a tool for assessing and tracking somatic dissociation and embodiment. The researcher utilized a client- centered approach and mindfulness-based interventions and theory to ground the work with the clients. While there were a variety of questionnaire-based tools for assessing dissociation with clients, many of them were lacking in the somatic component of dissociation. The available assessments were also exclusively self-reported and written or verbal, which had the potential to result in biased reporting. Clients may have also struggled to identify their level of somatic dissociation due to an inherent disconnection or dismissal of their somatic experience. This research described two case studies in which body scans and body mapping were utilized as a method to assess and track the client’s level of body dissociation and embodiment. -

Surfen, a Small Molecule Antagonist of Heparan Sulfate
Surfen, a small molecule antagonist of heparan sulfate Manuela Schuksz*†, Mark M. Fuster‡, Jillian R. Brown§, Brett E. Crawford§, David P. Ditto¶, Roger Lawrence*, Charles A. Glass§, Lianchun Wang*, Yitzhak Torʈ, and Jeffrey D. Esko*,** *Department of Cellular and Molecular Medicine, Glycobiology Research and Training Center, †Biomedical Sciences Graduate Program, ‡Department of Medicine, Division of Pulmonary and Critical Care Medicine and Veteran’s Administration San Diego Medical Center, ¶Moores Cancer Center, and ʈDepartment of Chemistry and Biochemistry, University of California at San Diego, La Jolla, CA 92093; and §Zacharon Pharmaceuticals, Inc, 505 Coast Blvd, South, La Jolla, CA 92037 Communicated by Carolyn R. Bertozzi, University of California, Berkeley, CA, June 18, 2008 (received for review May 26, 2007) In a search for small molecule antagonists of heparan sulfate, Surfen (bis-2-methyl-4-amino-quinolyl-6-carbamide) was first we examined the activity of bis-2-methyl-4-amino-quinolyl-6- described in 1938 as an excipient for the production of depot carbamide, also known as surfen. Fluorescence-based titrations insulin (16). Subsequent studies have shown that surfen can indicated that surfen bound to glycosaminoglycans, and the extent block C5a receptor binding (17) and lethal factor (LF) produced of binding increased according to charge density in the order by anthrax (18). It was also reported to have modest heparin- heparin > dermatan sulfate > heparan sulfate > chondroitin neutralizing effects in an oral feeding experiments in rats (19), sulfate. All charged groups in heparin (N-sulfates, O-sulfates, and but to our knowledge, no further studies involving heparin have carboxyl groups) contributed to binding, consistent with the idea been conducted, and its effects on HS are completely unknown. -

Activated Charcoal for Acute Poisoning: One Toxicologist's Journey
J. Med. Toxicol. (2010) 6:190–198 DOI 10.1007/s13181-010-0046-1 REVIEW ARTICLE Activated Charcoal for Acute Poisoning: One Toxicologist’s Journey Kent R. Olson Published online: 20 May 2010 # The Author(s) 2010. This article is published with open access at Springerlink.com Keywords Activated charcoal . Gastrointestinal As summarized by Matthew [13], Harstad and Danish decontamination . Poisoning . Drug overdose colleagues reported in 1942 that relatively little phenobar- bital was recovered by lavage even shortly after overdose [14] and this, along with their finding of particles of When I began studying clinical toxicology in 1981, the issue charcoal in the lungs of patients who died, led them to call of gastrointestinal decontamination after acute ingestion for the abandonment of gastric lavage for poisoning.) “ ” seemed pretty well settled: universal antidote, apomor- In recent years, my colleagues and I have continued to – phine and salt wateremesiswerenolongerused[1, 2]; and I debate the value of various methods of gastric decontam- was taught that barring a specific contraindication, the awake ination and the role and risks of activated charcoal, and it is patient was given syrup of ipecac to induce emesis, and the clear to me that the issue remains muddy. Some have taken drowsy or uncooperative patient was lavaged [3]. After a firm stand that no treatment should be recommended that is gastric emptying, everyone received activated charcoal not supported by evidence from a randomized controlled trial (AC). The only controversy seemed to be over whether one (RCT). Position statements published jointly by the Amer- should add a cathartic to speed gastrointestinal transit [4]. -

Management of Poisoning
MOH CLINICAL PRACTICE GUIDELINES December/2011 Management of Poisoning Health Ministry of Sciences Chapter of Emergency College of College of Family Manpower Authority Physicians Physicians, Physicians Academy of Medicine, Singapore Singapore Singapore Singapore Medical Pharmaceutical Society Society for Emergency Toxicology Singapore Paediatric Association of Singapore Medicine in Singapore Society (Singapore) Society Executive summary of recommendations Details of recommendations can be found in the main text at the pages indicated. Principles of management of acute poisoning – resuscitating the poisoned patient GPP In a critically poisoned patient, measures beyond standard resuscitative protocol like those listed above need to be implemented and a specialist experienced in poisoning management should be consulted (pg 55). GPP D Prolonged resuscitation should be attempted in drug-induced cardiac arrest (pg 55). Grade D, Level 3 1 C Titrated doses of naloxone, together with bag-valve-mask ventilation, should be administered for suspected opioid-induced coma, prior to intubation for respiratory insuffi ciency (pg 56). Grade C, Level 2+ D In bradycardia due to calcium channel or beta-blocker toxicity that is refractory to conventional vasopressor therapy, intravenous calcium, glucagon or insulin should be used (pg 57). Grade D, Level 3 B Patients with actual or potential life threatening cardiac arrhythmia, hyperkalaemia or rapidly progressive toxicity from digoxin poisoning should be treated with digoxin-specifi c antibodies (pg 57). Grade B, Level 2++ B Titrated doses of benzodiazepine should be given in hyperadrenergic- induced tachycardia states resulting from poisoning (pg 57). Grade B, Level 1+ D Non-selective beta-blockers, like propranolol, should be avoided in stimulant toxicity as unopposed alpha agonism may worsen accompanying hypertension (pg 57). -

Review of Succimer for Treatment of Lead Poisoning
Review of Succimer for treatment of lead poisoning Glyn N Volans MD, BSc, FRCP. Department of Clinical Pharmacology, School of Medicine at Guy's, King's College & St Thomas' Hospitals, St Thomas' Hospital, London, UK Lakshman Karalliedde MB BS, DA, FRCA Consultant Medical Toxicologist, CHaPD (London), Health Protection Agency UK, Visiting Senior Lecturer, Division of Public Health Sciences, King's College Medical School, King's College , London Senior Research Collaborator, South Asian Clinical Toxicology Research Collaboration, Faculty of Medicine, Peradeniya, Sri Lanka. Heather M Wiseman BSc MSc Medical Toxicology Information Services, Guy’s and St Thomas’ NHS Foundation Trust, London SE1 9RT, UK. Contact details: Heather Wiseman Medical Toxicology Information Services Guy’s & St Thomas’ NHS Foundation Trust Mary Sheridan House Guy’s Hospital Great Maze Pond London SE1 9RT Tel 020 7188 7188 extn 51699 or 020 7188 0600 (admin office) Date 10th March 2010 succimer V 29 Nov 10.doc last saved: 29-Nov-10 11:30 Page 1 of 50 CONTENTS 1 Summary 2. Name of the focal point in WHO submitting or supporting the application 3. Name of the organization(s) consulted and/or supporting the application 4. International Nonproprietary Name (INN, generic name) of the medicine 5. Formulation proposed for inclusion 6. International availability 7. Whether listing is requested as an individual medicine or as an example of a therapeutic group 8. Public health relevance 8.1 Epidemiological information on burden of disease due to lead poisoning 8.2 Assessment of current use 8.2.1 Treatment of children with lead poisoning 8.2.2 Other indications 9. -

Treatment of Self-Poisoned Adults G
Archives of Emergency Medicine, 1985, 2, 203-208 Ipecacuanha induced emesis in the treatment of self-poisoned adults G. GORDON Accident and Emergency Department, Manor Hospital, Nuneaton, Warwickshire, England SUMMARY One hundred consecutive adult patients presenting to an Accident and Emergency Department following intentional self-poisoning were given 50 to 80 ml Paediatric Ipecacuanha Emetic Mixture BP as an emetic, together with two or three glasses of strong orange juice. A satisfactory emetic result was obtained in 99 patients. No toxic effects were noted in these patients, or in the one patient in whom emesis did not occur, and who subsequently refused gastric lavage. The potential toxicity of Ipecacuanha Syrup itself is discussed, and attention drawn to the lower Emetine content of Paediatric Ipecacuanha Emetic Mixture (BP), rather than that of the formulations used in previously published reports. The use of Paediatric Ipecacuanha Emetic Mixture B.P. in adults is effective and safe in this dosage. INTRODUCTION The methods available for retrieval of poisoning agents from the stomach are gastric lavage and emesis. In the United Kingdom at the present time, gastric lavage is the method most commonly used in the treatment of adults. It is an unpleasant and time consuming procedure for both patient and staff, and it is not without risk (Matthew et al., 1966), even in the hands of the experienced nursing staff who usually carry it out. Doubt still remains about its effectiveness (Goulding & Volans, 1977), and the basis for its use rests more on the occasional recovery of large quantities of drug, rather than verification of its routine efficiency by studies in man (Melman & Morelli, 1978). -

GHS Calcium Lactate Gluconate MSDS.Pdf
Safety Data Sheet (Calcium Lactate Gluconate) DATE PREPARED: 7/9/2015 Section 1. Product and Company Identification Product Name Calcium Lactate Gluconate CAS Number 11116-97-5 Parchem - fine & specialty chemicals EMERGENCY RESPONSE NUMBER 415 Huguenot Street CHEMTEL New Rochelle, NY 10801 Toll Free US & Canada: 1 (800) 255-3924 (914) 654-6800 (914) 654-6899 All other Origins: 1 (813) 248-0585 parchem.com [email protected] Collect Calls Accepted Section 2. Hazards Identification Classification of the substance or mixture Classification according to Directive 67/548/EEC or 1999/45/EC as amended: This preparation does not meet the criteria for classification according to Directive 1999/45/EC as amended. Classification according to Regulation (EC) No 1272/2008 as amended: This mixture does not meet the criteria for classification according to Regulation (EC) 1272/2008 as amended. Hazard and precautionary statements Hazard statements: The substance does not meet the criteria for classification. Precautionary statements: Not available. Appearance & Odor: White powder with no odor. Fire & Explosion Hazards Potential for dust explosion may exist. This product is not defined as flammable or combustible. However, the product may decompose under fire conditions to produce toxic oxides of carbon. Depending upon conditions, dusts may be sensitive to static discharge. Avoid possibility of dry powder and friction causing static electricity in presence of flammables (See NFPA-77, Chpt. 6) Primary Route of Exposure: Skin and eye contact are the primary routes of exposure to this product. Inhalation Acute Exposure: Inhalation of dust may cause mild irritation. Skin Contact - Acute: Skin contact is not expected to cause irritation. -

Guideline on Antidote Availability for Emergency Departments January 2017
Royal College of Emergency Medicine and National Poisons Information Service Guideline on Antidote Availability for Emergency Departments January 2017 TOXBASE and/or the BNF should be consulted for further advice on doses and indications for antidote administration and, if necessary, the National Poisons Information Service (NPIS) should be telephoned for more patient-specific advice. Contact details for NPIS are available on TOXBASE. Additional drugs that are used in the poisoned patient that are widely available in ED are not listed in the table – in particular it is important to ensure that insulin, benzodiazepines (diazepam and/or lorazepam), glyceryl trinitrate or isosorbide dinitrate and magnesium are immediately available in the ED. The following drugs should be immediately available in the ED or any area where poisoned patients are initially treated. These drugs should be held in a designated storage facility* The stock held should be sufficient to initiate treatment (stocking guidance is in Appendix 1). Drug Indication Acetylcysteine Paracetamol Activated charcoal Many oral poisons Atropine Organophosphorus or carbamate insecticides Bradycardia Calcium chloride Calcium channel blockers Systemic effects of hydrofluoric acid Calcium gluconate Local infiltration for hydrofluoric acid Calcium gluconate gel Hydrofluoric acid Cyanide antidotes Cyanide Dicobalt edetate The choice of antidote depends on the severity of poisoning, certainty of diagnosis and cause Hydroxocobalamin (Cyanokit®) of poisoning/source of cyanide. Sodium nitrite - Dicobalt edetate is the antidote of choice in severe cases when there is a high clinical Sodium thiosulphate suspicion of cyanide poisoning e.g. after cyanide salt exposure. - Hydroxocobalamin (Cyanokit®) should be considered in smoke inhalation victims who have a severe lactic acidosis, are comatose, in cardiac arrest or have significant cardiovascular compromise - Sodium nitrite may be used if dicobalt edetate is not available. -

XELJANZ (Tofacitinib)
HIGHLIGHTS OF PRESCRIBING INFORMATION Psoriatic Arthritis (in combination with nonbiologic DMARDs) These highlights do not include all the information needed to use XELJANZ 5 mg twice daily or XELJANZ XR 11 mg once daily. (2.2) XELJANZ/XELJANZ XR safely and effectively. See full prescribing Recommended dosage in patients with moderate and severe renal information for XELJANZ. impairment or moderate hepatic impairment is XELJANZ 5 mg once daily. (2, 8.7, 8.8) ® XELJANZ (tofacitinib) tablets, for oral use Ulcerative Colitis ® XELJANZ XR (tofacitinib) extended-release tablets, for oral use XELJANZ 10 mg twice daily for at least 8 weeks; then 5 or 10 mg Initial U.S. Approval: 2012 twice daily. Discontinue after 16 weeks of 10 mg twice daily, if adequate therapeutic benefit is not achieved. Use the lowest effective dose to WARNING: SERIOUS INFECTIONS AND MALIGNANCY maintain response. (2.3) See full prescribing information for complete boxed warning. Recommended dosage in patients with moderate and severe renal impairment or moderate hepatic impairment: half the total daily dosage Serious infections leading to hospitalization or death, including recommended for patients with normal renal and hepatic function. (2, 8.7, tuberculosis and bacterial, invasive fungal, viral, and other 8.8) opportunistic infections, have occurred in patients receiving Dosage Adjustment XELJANZ. (5.1) See the full prescribing information for dosage adjustments by indication If a serious infection develops, interrupt XELJANZ/XELJANZ XR for patients receiving CYP2C19 and/or CYP3A4 inhibitors; in patients until the infection is controlled. (5.1) with moderate or severe renal impairment or moderate hepatic Prior to starting XELJANZ/XELJANZ XR, perform a test for latent impairment; and patients with lymphopenia, neutropenia, or anemia. -

1: Gastro-Intestinal System
1 1: GASTRO-INTESTINAL SYSTEM Antacids .......................................................... 1 Stimulant laxatives ...................................46 Compound alginate products .................. 3 Docuate sodium .......................................49 Simeticone ................................................... 4 Lactulose ....................................................50 Antimuscarinics .......................................... 5 Macrogols (polyethylene glycols) ..........51 Glycopyrronium .......................................13 Magnesium salts ........................................53 Hyoscine butylbromide ...........................16 Rectal products for constipation ..........55 Hyoscine hydrobromide .........................19 Products for haemorrhoids .................56 Propantheline ............................................21 Pancreatin ...................................................58 Orphenadrine ...........................................23 Prokinetics ..................................................24 Quick Clinical Guides: H2-receptor antagonists .......................27 Death rattle (noisy rattling breathing) 12 Proton pump inhibitors ........................30 Opioid-induced constipation .................42 Loperamide ................................................35 Bowel management in paraplegia Laxatives ......................................................38 and tetraplegia .....................................44 Ispaghula (Psyllium husk) ........................45 ANTACIDS Indications: -

Wednesday May 26, 1999
5±26±99 Vol. 64 No. 101 Wednesday Pages 28333±28712 May 26, 1999 federal register 1 VerDate 06-MAY-99 21:29 May 25, 1999 Jkt 183247 PO 00000 Frm 00001 Fmt 4710 Sfmt 4710 E:\FR\FM\26MYWS.XXX pfrm03 PsN: 26MYWS II Federal Register / Vol. 64, No. 101 / Wednesday, May 26, 1999 The FEDERAL REGISTER is published daily, Monday through SUBSCRIPTIONS AND COPIES Friday, except official holidays, by the Office of the Federal Register, National Archives and Records Administration, PUBLIC Washington, DC 20408, under the Federal Register Act (44 U.S.C. Subscriptions: Ch. 15) and the regulations of the Administrative Committee of Paper or fiche 202±512±1800 the Federal Register (1 CFR Ch. I). The Superintendent of Assistance with public subscriptions 512±1806 Documents, U.S. Government Printing Office, Washington, DC 20402 is the exclusive distributor of the official edition. General online information 202±512±1530; 1±888±293±6498 Single copies/back copies: The Federal Register provides a uniform system for making available to the public regulations and legal notices issued by Paper or fiche 512±1800 Federal agencies. These include Presidential proclamations and Assistance with public single copies 512±1803 Executive Orders, Federal agency documents having general FEDERAL AGENCIES applicability and legal effect, documents required to be published Subscriptions: by act of Congress, and other Federal agency documents of public Paper or fiche 523±5243 interest. Assistance with Federal agency subscriptions 523±5243 Documents are on file for public inspection in the Office of the Federal Register the day before they are published, unless the issuing agency requests earlier filing. -
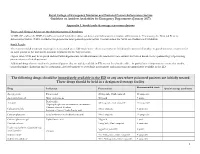
RCEM NPIS Antidote Guideline Appx 1
Royal College of Emergency Medicine and National Poisons Information Service Guideline on Antidote Availability for Emergency Departments (January 2017) Appendix 1. Stock levels & storage recommendations Doses and Clinical Advice on the Administration of Antidotes TOXBASE and/or the BNF should be consulted for further advice on doses and indications for antidote administration. If necessary, the National Poisons Information Service (NPIS) should be telephoned for more patient-specific advice. Contact details for NPIS are available on TOXBASE. Stock Levels The recommended minimum stocking levels (rounded up to full “pack-sizes” where necessary) are based on the amount of antidote required to initiate treatment for an adult patient in the ED and to continue treatment for the first 24 hours. Higher stock levels may be required and individual departments should determine the amount of each antidote they stock based on the epidemiology of poisoning presentations to their department. Additional drugs that are used in the poisoned patient that are widely available in ED are not listed in the table – in particular it is important to ensure that insulin, benzodiazepines (diazepam and/or lorazepam), glyceryl trinitrate or isosorbide mononitrate and magnesium are immediately available in the ED. The following drugs should be immediately available in the ED or any area where poisoned patients are initially treated These drugs should be held in a designated storage facility Recommended stock Drug Indication Presentation Special storage conditions