Mercury Study Report to Congress
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chemical Forms of Mercury in Human Hair Reveal Sources of Exposure
Chemical Forms of Mercury in Human Hair Reveal Sources of Exposure Alain Manceau, Mironel Enescu, Alexandre Simionovici, Martine Lanson, Maria Gonzalez-Rey, Mauro Rovezzi, Rémi Tucoulou, Pieter Glatzel, Kathryn Nagy, Jean-Paul Bourdineaud To cite this version: Alain Manceau, Mironel Enescu, Alexandre Simionovici, Martine Lanson, Maria Gonzalez-Rey, et al.. Chemical Forms of Mercury in Human Hair Reveal Sources of Exposure. Environmental Science and Technology, American Chemical Society, 2016, 50 (19), pp.10721-10729. 10.1021/acs.est.6b03468. hal-03176383 HAL Id: hal-03176383 https://hal.archives-ouvertes.fr/hal-03176383 Submitted on 22 Mar 2021 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Chemical Forms of Mercury in Human Hair Reveal Sources of Exposure Alain Manceau,*,† Mironel Enescu,‡ Alexandre Simionovici,† Martine Lanson,† Maria Gonzalez-Rey,§ Mauro Rovezzi,∥ Rémi Tucoulou,∥ Pieter Glatzel,∥ Kathryn L. Nagy,*,⊥ Jean-Paul Bourdineaud*,# †ISTerre, Université Grenoble Alpes, CNRS, CS 40700, 38058 Grenoble, France. ‡Laboratoire Chrono Environnement, Université de Franche-Comté, CNRS, 25030 Besançon, France. §Laboratoire EPOC, Université de Bordeaux, CNRS, 33120 Arcachon, France. ∥European Synchrotron Radiation Facility (ESRF), 71 Rue des Martyrs, 38000 Grenoble, France. ⊥Department of Earth and Environmental Sciences, MC-186, 845 West Taylor Street, University of Illinois at Chicago, Chicago, Illinois 60607, United States. -

Ethylene Glycol
NTP-CERHR Monograph on the Potential Human Reproductive and Developmental Effects of Ethylene Glycol January 2004 NIH Publication No. 04-4481 Table of Contents Preface .............................................................................................................................................v Introduction .................................................................................................................................... vi NTP Brief on Ethylene Glycol .........................................................................................................1 References ........................................................................................................................................4 Appendix I. NTP-CERHR Ethylene Glycol / Propylene Glycol Expert Panel Preface ..............................................................................................................................I-1 Expert Panel ......................................................................................................................I-2 Appendix II. Expert Panel Report on Ethylene Glycol ............................................................... II-i Table of Contents ........................................................................................................... II-iii Abbreviations ...................................................................................................................II-v List of Tables ............................................................................................................... -

TOXICOLOGY and EXPOSURE GUIDELINES ______(For Assistance, Please Contact EHS at (402) 472-4925, Or Visit Our Web Site At
(Revised 1/03) TOXICOLOGY AND EXPOSURE GUIDELINES ______________________________________________________________________ (For assistance, please contact EHS at (402) 472-4925, or visit our web site at http://ehs.unl.edu/) "All substances are poisons; there is none which is not a poison. The right dose differentiates a poison and a remedy." This early observation concerning the toxicity of chemicals was made by Paracelsus (1493- 1541). The classic connotation of toxicology was "the science of poisons." Since that time, the science has expanded to encompass several disciplines. Toxicology is the study of the interaction between chemical agents and biological systems. While the subject of toxicology is quite complex, it is necessary to understand the basic concepts in order to make logical decisions concerning the protection of personnel from toxic injuries. Toxicity can be defined as the relative ability of a substance to cause adverse effects in living organisms. This "relative ability is dependent upon several conditions. As Paracelsus suggests, the quantity or the dose of the substance determines whether the effects of the chemical are toxic, nontoxic or beneficial. In addition to dose, other factors may also influence the toxicity of the compound such as the route of entry, duration and frequency of exposure, variations between different species (interspecies) and variations among members of the same species (intraspecies). To apply these principles to hazardous materials response, the routes by which chemicals enter the human body will be considered first. Knowledge of these routes will support the selection of personal protective equipment and the development of safety plans. The second section deals with dose-response relationships. -

A Short History of Occupational Disease: 2. Asbestos, Chemicals
Ulster Med J 2021;90(1):32-34 Medical History A SHORT HISTORY OF OCCUPATIONAL DISEASE: 2. ASBESTOS, CHEMICALS, RADIUM AND BEYOND Petts D, Wren MWD, Nation BR, Guthrie G, Kyle B, Peters L, Mortlock S, Clarke S, Burt C. ABSTRACT OCCUPATIONAL CANCER Historically, the weighing out and manipulation of dangerous Towards the end of the 18th century, a possible causal link chemicals frequently occurred without adequate protection between chemicals and cancer was reported by two London from inhalation or accidental ingestion. The use of gloves, surgeons. In 1761, John Hill reported an association between eye protection using goggles, masks or visors was scant. snuff, a tobacco product, and nasopharyngeal cancer, From Canary Girls and chimney sweeps to miners, stone and, in 1775, Percival Pott described a high incidence of cutters and silo fillers, these are classic exemplars of the subtle scrotal cancer in chimney sweeps. Pott, a surgeon at St (and in some cases not so subtle) effects that substances, Bartholomew’s Hospital in London, published his findings,6 environments and practices can have on individual health. which he attributed to contamination with soot. This excellent INTRODUCTION epidemiological study is considered to be the first report of a potential carcinogen. Pott’s work led to the foundation of It has been known for many centuries that certain diseases occupational medicine and to the Chimney Sweep Act of were associated with particular occupations (i.e. wool- 1788. In 1895, Ludwig Reyn reported that aromatic amines sorters disease in the textile industry, cowpox in milk maids used in certain dye industries in Germany were linked and respiratory problems in miners and stone workers). -

Lead Poisoning
3 Dec 2003 21:51 AR AR206-ME55-13.tex AR206-ME55-13.sgm LaTeX2e(2002/01/18) P1: GBC 10.1146/annurev.med.55.091902.103653 Annu. Rev. Med. 2004. 55:209–22 doi: 10.1146/annurev.med.55.091902.103653 Copyright c 2004 by Annual Reviews. All rights reserved First published online as a Review in Advance on Aug. 18, 2003 LEAD POISONING Herbert Needleman Professor of Psychiatry and Pediatrics, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania 15213; email: [email protected] ■ Abstract Understanding of lead toxicity has advanced substantially over the past three decades, and focus has shifted from high-dose effects in clinically symptomatic individuals to the consequences of exposure at lower doses that cause no symptoms, particularly in children and fetuses. The availability of more sensitive analytic methods has made it possible to measure lead at much lower concentrations. This advance, along with more refined epidemiological techniques and better outcome measures, has lowered the least observable effect level until it approaches zero. As a consequence, the segment of the population who are diagnosed with exposure to toxic levels has expanded. At the same time, environmental efforts, most importantly the removal of lead from gasoline, have dramatically reduced the amount of lead in the biosphere. The remaining major source of lead is older housing stock. Although the cost of lead paint abatement is measured in billions of dollars, the monetized benefits of such a Herculean task have been shown to far outweigh the costs. INTRODUCTION In recent years, the focus in lead poisoning has shifted away from adults exposed to high doses in industrial settings to the larger population of asymptomatic chil- dren with lesser exposures. -
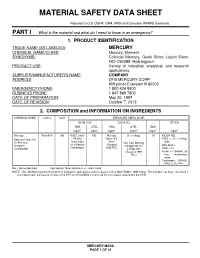
Material Safety Data Sheet
MATERIAL SAFETY DATA SHEET Prepared to U.S. OSHA, CMA, ANSI and Canadian WHMIS Standards PART I What is the material and what do I need to know in an emergency? 1. PRODUCT IDENTIFICATION TRADE NAME (AS LABELED) : MERCURY CHEMICAL NAME/CLASS : Mercury; Element SYNONYMS: Colloidal Mercury, Quick Silver; Liquid Silver; NCI-C60399; Hydrargyrum PRODUCT USE : Variety of industrial, analytical, and research applications. SUPPLIER/MANUFACTURER'S NAME : COMPANY ADDRESS : DFG MERCURY CORP 909 pitner Evanston Ill 60202 EMERGENCY PHONE : 1 800 424 9300 BUSINESS PHONE : 1 847 869 7800 DATE OF PREPARATION : May 20, 1997 DATE OF REVISION : October 7, 2013 2. COMPOSITION and INFORMATION ON INGREDIENTS CHEMICAL NAME CAS # %w/w EXPOSURE LIMITS IN AIR ACGIH-TLV OSHA-PEL OTHER TWA STEL TWA STEL IDLH mg/m 3 mg/m 3 mg/m 3 mg/m 3 mg/m 3 mg/m 3 Mercury 7439-97-6 100 0.025, (skin) NE Mercury 0.1 (ceiling) 10 NIOSH REL: Exposure limits are A4 (Not Vapor: 0.5, STEL = 0.1 (ceiling, for Mercury, Classifiable Skin; Non-alkyl Mercury skin) Inorganic as a Human (Vacated Compounds: 0.1 DFG MAKs: Compounds Carcinogen) 1989 PEL) Ceiling, skin TWA = 0.1 (Vacated 1989 PEAK = 10 •MAK 30 PEL) min., momentary value Carcinogen: EPA-D; IARC-3, TLV-A4 NE = Not Established. See Section 16 for Definitions of Terms Used. NOTE: ALL WHMIS required information is included in appropriate sections based on the ANSI Z400.1-1998 format. This product has been classified in accordance with the hazard criteria of the CPR and the MSDS contains all the information required by the CPR. -

Complete Issue (PDF)
Abstracts Eliminating Occupational Disease: areas in the country. The study studied 40 small scale industries, and collected 40 water samples (potable) for cyanide and mer- Translating Research into Action cury which are used in mining. Questionnaire-guided interviews EPICOH 2017 and work analysis covering mining practices and risk exposures were conducted, as well as chemical analysis through gas chro- 28–31 August 2017, Edinburgh, UK matography. Results of the study showed unsafe conditions in the industries such as risk of fall during erection and dismantling of scaffolds, guard rails were not provided in scaffoldings, man- Poster Presentation ual extraction of underground ores, use of explosives, poor visi- bility in looking for ores to take out to surface, exposure to Pesticides noise from explosives, and to dust from the demolished struc- tures. Mine waste was drained into soil or ground and/or rivers and streams. The most common health problems among miners 0007 ASSESSMENT OF PESTICIDE EXPOSURE AND were hypertension (62%), followed by hypertensive cardiovascu- OCCUPATIONAL SAFETY AND HEALTH OF FARMERS IN lar disease due to left wall ischemia (14%). Health symptoms THE PHILIPPINES such as dermatitis, and peripheral neuropathy were noted and Jinky Leilanie Lu. National Institutes of Health, Institute of Health Policy and Development these can be considered as manifestations of chronic cyanide poi- Studies, University of the Philippines Manila, Manila, The Philippines soning, further, aggravated by improper use of protective equip- ment. For the environmental samples of potable water, 88% and 10.1136/oemed-2017-104636.1 98% were positive with mercury and cyanide respectively. About 52% of drinking water samples exceeded the TLV for mercury Aims This is a study conducted among 534 farmers in an while 2% exceeded the TLV for cyanide. -

At Work in the World
Perspectives in Medical Humanities At Work in the World Proceedings of the Fourth International Conference on the History of Occupational and Environmental Health Edited by Paul D. Blanc, MD and Brian Dolan, PhD Page Intentionally Left Blank At Work in the World Proceedings of the Fourth International Conference on the History of Occupational and Environmental Health Perspectives in Medical Humanities Perspectives in Medical Humanities publishes scholarship produced or reviewed under the auspices of the University of California Medical Humanities Consortium, a multi-campus collaborative of faculty, students and trainees in the humanities, medi- cine, and health sciences. Our series invites scholars from the humanities and health care professions to share narratives and analysis on health, healing, and the contexts of our beliefs and practices that impact biomedical inquiry. General Editor Brian Dolan, PhD, Professor of Social Medicine and Medical Humanities, University of California, San Francisco (ucsf) Recent Monograph Titles Health Citizenship: Essays in Social Medicine and Biomedical Politics By Dorothy Porter (Fall 2011) Paths to Innovation: Discovering Recombinant DNA, Oncogenes and Prions, In One Medical School, Over One Decade By Henry Bourne (Fall 2011) The Remarkables: Endocrine Abnormalities in Art By Carol Clark and Orlo Clark (Winter 2011) Clowns and Jokers Can Heal Us: Comedy and Medicine By Albert Howard Carter iii (Winter 2011) www.medicalhumanities.ucsf.edu [email protected] This series is made possible by the generous support of the Dean of the School of Medicine at ucsf, the Center for Humanities and Health Sciences at ucsf, and a Multi-Campus Research Program grant from the University of California Office of the President. -
Survey of Mercury and Mercury Compounds
Survey of mercury and mercury compounds Part of the LOUS-review Environmental Project No. 1544, 2014 Title: Authors and contributors: Survey of mercury and mercury compounds Jakob Maag Jesper Kjølholt Sonja Hagen Mikkelsen Christian Nyander Jeppesen Anna Juliana Clausen and Mie Ostenfeldt COWI A/S, Denmark Published by: The Danish Environmental Protection Agency Strandgade 29 1401 Copenhagen K Denmark www.mst.dk/english Year: ISBN no. 2014 978-87-93026-98-8 Disclaimer: When the occasion arises, the Danish Environmental Protection Agency will publish reports and papers concerning research and development projects within the environmental sector, financed by study grants provided by the Danish Environmental Protection Agency. It should be noted that such publications do not necessarily reflect the position or opinion of the Danish Environmental Protection Agency. However, publication does indicate that, in the opinion of the Danish Environmental Protection Agency, the content represents an important contribution to the debate surrounding Danish environmental policy. While the information provided in this report is believed to be accurate, the Danish Environmental Protection Agency disclaims any responsibility for possible inaccuracies or omissions and consequences that may flow from them. Neither the Danish Environmental Protection Agency nor COWI or any individual involved in the preparation of this publication shall be liable for any injury, loss, damage or prejudice of any kind that may be caused by persons who have acted based on their understanding of the information contained in this publication. Sources must be acknowledged. 2 Survey of mercury and mercury compounds Contents Preface ...................................................................................................................... 5 Summary and conclusions ......................................................................................... 7 Sammenfatning og konklusion ................................................................................ 14 1. -

From Murder to Mechanisms 7000 Years of Toxicology's Evolution
From Murder to Mechanisms 7000 Years of Toxicology’s Evolution 7000 Years of Toxicology’s Evolution Michael A. Gallo, PhD, DABT (ret), Emeritus Fellow ATS Professor Emeritus Environmental and Occupational Health Sciences Institute Rutgers-Robert Wood Johnson Medical School Piscataway, New Jersey Toxicants: Friends or Foes? “The dose makes the poison” Paracelsus 1493-1541 Objectives This presentation provides a history of toxicology with a few classic examples. The Family of Toxicology Poisons Signs, Symptoms, Adverse Reactions & Antidotes Drugs Patent Medicines and Chemotherapeutics Food Natural toxicants Industrial Chemicals Occupational and Environmental Toxicity Safety Evaluation Hazard Identification Tools to Elucidate Biology Toxicology the Borrowing Science • Pharmacology • Pathology • Physiology • Biochemistry • Synthetic Chemistry • Analytical Chemistry • Molecular and Cellular Biology • High Resolution Imaging Earliest Humans* • Use of natural toxins • Oral history evolved • Animal venoms • Toxic metals • Plant extracts – Hunting* – Warfare – Assassination * still used by indigenous people in S. America, Borneo, Pacific Islanders Ebers Papyrus ~1500 BCE • Hemlock • Aconite (buttercup family) • Opium • Lead • Copper • Antimony • Venoms Hippocrates and Friends • Defined effective dosages of toxin • Described bioavailability • Theophastus (370-286 BCE) – De Historia Plantanum • Socrates- Hemlock • Dioscorides (Nero)poison classes through 19th • Discovery of BellaDonna (scopolamine) • Discovery of Digitalis (foxglove)Dioscorides -

The Thimerosal Controversy
The Thimerosal Controversy Aimee Sutherland, VRG Research Assistant April 2013 Background In the early 1920s, a major public health concern was vaccine contamination with bacteria and other germs, which could result in the death of children receiving the vaccines from tainted vials. In the book “The Hazards of Immunization”, Sir Graham S. Wilson depicts an occurrence of contamination that happened in Australia in 1928 in which twelve out of twenty-one children died after receiving the vaccine for diphtheria due to multiple staphylococcal abscesses and toxemia (FDA). This incident spurred the development of preservatives for multi-dose vials of vaccine. In 1928, Eli Lilly was the first pharmaceutical company to introduce thimerosal, an organomercury compound that is approximately 50% mercury by weight, as a preservative that would thwart microbial growth (FDA). After its introduction as a germocide, thimerosal was often challenged for its efficacy rather than its safety. The American Medical Association (AMA) published an article that questioned the effectiveness of the organomercury compounds over the inorganic mercury ones (Baker, 245). In 1938 manufacturers were required to submit safety-testing information to the Food and Drug Administration (FDA). Although preservatives had already been incorporated into many vaccines, it was not until 1968 that preservatives were required for multi-dose vials in the United States Code of Federal Regulations (FDA). In 1970s the American population, increasingly concerned about environmental contamination with heavy metals, began to have reservations about the safety of organomercury and the controversy regarding thimerosal ensued after. The Controversy In 1990s, the use of thimerosal as a preservative became controversial and was targeted as a possible cause of autism because of its mercury content. -

3.5 3.6 Rangan Metals Metalloids New Orleans
Metals/Metalloids Metals and Metalloids Cyrus Rangan MD, FAAP, ACMT Los Angeles County Department of Public Health California Poison Control System Childrens Hospital Los Angeles 1 Treatment of Metal Poisoning Old School Approaches “The treatment of acute [insert metal here]-poisoning consists in the evacuation of the stomach, if necessary, the exhibition of the sulphate of sodium or of magnesium, and the meeting of the indications as they arise. The Epsom and Glauber’s salts act as chemical antidotes, by precipitating the insoluble sulphate of [insert metal here], and also, if in excess, empty the bowel of the compound formed. To allay gastrointestinal irritation, albuminous drinks should be given and opium freely exhibited…” Wood, HC: Therapeutics Materia Medica and Toxicology, 1879 2 Treatment of Metal Poisoning Old School Approaches “If possible, the rapid administration of 2 oz. (6-7 heaping teaspoonfuls) of Magnesium sulfate (Epsom Salts) or Sodium sulfate (Glauber’s Salt) in plenty of water. Alum (aluminum potassium sulfate) will also be useful in 4 gm (60 gr.) doses (dissolved) repeated. Very dilute Sulfuric acid may be employed (30 cc of a 10 % solution diluted to 1 quart). All soluble sulfates precipitate [metal] as an insoluble sulfate…” Lucas, GW: The Symptoms and Treatment of Acute Poisoning; 1953 3 1 Metals/Metalloids Overview of Metals • Iron • Lead • Arsenic • Mercury • … a whole bunch of other ones 4 What’s a Metal? What’s a Metalloid? 5 Iron Poisoning Introduction • Essential for normal tissue and organ function • In toxic doses, iron salts (ferrous sulfate, fumarate or gluconate) cause corrosive gastrointestinal effects followed by hypotension, metabolic acidosis, and multisystem failure.