Afifa Irani Thesis for ETD.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Placement of Children with Relatives
STATE STATUTES Current Through January 2018 WHAT’S INSIDE Placement of Children With Giving preference to relatives for out-of-home Relatives placements When a child is removed from the home and placed Approving relative in out-of-home care, relatives are the preferred placements resource because this placement type maintains the child’s connections with his or her family. In fact, in Placement of siblings order for states to receive federal payments for foster care and adoption assistance, federal law under title Adoption by relatives IV-E of the Social Security Act requires that they Summaries of state laws “consider giving preference to an adult relative over a nonrelated caregiver when determining a placement for a child, provided that the relative caregiver meets all relevant state child protection standards.”1 Title To find statute information for a IV-E further requires all states2 operating a title particular state, IV-E program to exercise due diligence to identify go to and provide notice to all grandparents, all parents of a sibling of the child, where such parent has legal https://www.childwelfare. gov/topics/systemwide/ custody of the sibling, and other adult relatives of the laws-policies/state/. child (including any other adult relatives suggested by the parents) that (1) the child has been or is being removed from the custody of his or her parents, (2) the options the relative has to participate in the care and placement of the child, and (3) the requirements to become a foster parent to the child.3 1 42 U.S.C. -

The Major Influences of the Boundless-Extended Family System on The
Fayetteville State University DigitalCommons@Fayetteville State University Faculty Working Papers from the School of School of Education Education Summer 2008 The aM jor Influences of the Boundless-Extended Family System on the Professional Experiences of Black Zimbabwean Women Leaders in Higher Education Miriam Chitiga Fayetteville State University, [email protected] Follow this and additional works at: http://digitalcommons.uncfsu.edu/soe_faculty_wp Part of the Higher Education Commons Recommended Citation Chitiga, Miriam, "The aM jor Influences of the Boundless-Extended Family System on the Professional Experiences of Black Zimbabwean Women Leaders in Higher Education" (2008). Faculty Working Papers from the School of Education. Paper 25. http://digitalcommons.uncfsu.edu/soe_faculty_wp/25 This Article is brought to you for free and open access by the School of Education at DigitalCommons@Fayetteville State University. It has been accepted for inclusion in Faculty Working Papers from the School of Education by an authorized administrator of DigitalCommons@Fayetteville State University. For more information, please contact [email protected]. Forum on Public Policy The Major Influences of the Boundless-Extended Family System on the Professional Experiences of Black Zimbabwean Women Leaders in Higher Education Miriam Miranda Chitiga, Claflin University, Orangeburg, South Carolina Abstract The article examines the major influences of the black Zimbabwean boundless- extended family system on the professional trajectories of women leaders working within the higher education system of Zimbabwe. The study is based on in-depth interviews conducted with thirty female leaders who shared information about their major family responsibilities. Using an analytical framework that facilitates a critical analysis of the evidence, the paper discusses the persisting significance of the interdependent systems of social stratification, namely race, nationality, gender, sexual orientation, and class in the private and public spheres of the female leaders. -

Major Trends Affecting Families in Central America and the Caribbean
Major Trends Affecting Families in Central America and the Caribbean Prepared by: Dr. Godfrey St. Bernard The University of the West Indies St. Augustine Trinidad and Tobago Phone Contacts: 1-868-776-4768 (mobile) 1-868-640-5584 (home) 1-868-662-2002 ext. 2148 (office) E-mail Contacts: [email protected] [email protected] Prepared for: United Nations Division of Social Policy and Development Department of Economic and Social Affairs Program on the Family Date: May 23, 2003 Introduction Though an elusive concept, the family is a social institution that binds two or more individuals into a primary group to the extent that the members of the group are related to one another on the basis of blood relationships, affinity or some other symbolic network of association. It is an essential pillar upon which all societies are built and with such a character, has transcended time and space. Often times, it has been mooted that the most constant thing in life is change, a phenomenon that is characteristic of the family irrespective of space and time. The dynamic character of family structures, - including members’ status, their associated roles, functions and interpersonal relationships, - has an important impact on a host of other social institutional spheres, prospective economic fortunes, political decision-making and sustainable futures. Assuming that the ultimate goal of all societies is to enhance quality of life, the family constitutes a worthy unit of inquiry. Whether from a social or economic standpoint, the family is critical in stimulating the well being of a people. The family has been and will continue to be subjected to myriad social, economic, cultural, political and environmental forces that shape it. -

Kin Relationships
In H. T. Reis & S. Sprecher (Eds.), Encyclopedia of human relationships (pp. 951-954). Thousand Oaks, CA: Sage. Kin Relationships Kin relationships are traditionally defined as ties based on blood and marriage. They include lineal generational bonds (children, parents, grandparents, and great- grandparents), collateral bonds (siblings, cousins, nieces and nephews, and aunts and uncles), and ties with in-laws. An often-made distinction is that between primary kin (members of the families of origin and procreation) and secondary kin (other family members). The former are what people generally refer to as “immediate family,” and the latter are generally labeled “extended family.” Marriage, as a principle of kinship, differs from blood in that it can be terminated. Given the potential for marital break-up, blood is recognized as the more important principle of kinship. This entry questions the appropriateness of traditional definitions of kinship for “new” family forms, describes distinctive features of kin relationships, and explores varying perspectives on the functions of kin relationships. Questions About Definition Changes over the last thirty years in patterns of family formation and dissolution have given rise to questions about the definition of kin relationships. Guises of kinship have emerged to which the criteria of blood and marriage do not apply. Assisted reproduction is a first example. Births resulting from infertility treatments such as gestational surrogacy and in vitro fertilization with ovum donation challenge the biogenetic basis for kinship. A similar question arises for adoption, which has a history 2 going back to antiquity. Partnerships formed outside of marriage are a second example. Strictly speaking, the family ties of nonmarried cohabitees do not fall into the category of kin, notwithstanding the greater acceptance over time of consensual unions both formally and informally. -

Dna by the Entirety
DNA BY THE ENTIRETY Natalie Ram The law fails to accommodate the inconvenient fact that an individual’s identifiable genetic information is involuntarily and immutably shared with her close genetic relatives. Legal institutions have established that individuals have a cognizable interest in control- ling genetic information that is identifying to them. The Supreme Court recognized in Maryland v. King that the Fourth Amendment is impli- cated when arrestees’ DNA is analyzed, and the Genetic Information Nondiscrimination Act protects individuals from genetic discrimination in the employment and health-insurance markets. But genetic infor- mation is not like other forms of private or personal information because it is shared—immutably and involuntarily—in ways that are identifying of both the source and that person’s close genetic relatives. Standard approaches to addressing interests in genetic information have largely failed to recognize this characteristic, treating such infor- mation as individualistic. While many legal frames may be brought to bear on this problem, this Article focuses on the law of property. Specifically, looking to the law of tenancy by the entirety, this Article proposes one possible frame- work for grappling with the overlapping interests implicated in genetic identification and analysis. Tenancy by the entirety, like interests in shared identifiable genetic information, calls for the difficult task of conceptualizing two persons as one. The law of tenancy by the entirety thus provides a useful analytical framework for considering how legal institutions might take interests in shared identifiable genetic infor- mation into account. This Article examines how this framework may shape policy approaches in three domains: forensic identification, genetic research, and personal genetic testing. -

Family Formation and the Home Pamela Laufer-Ukeles University of Dayton School of Law
Kentucky Law Journal Volume 104 | Issue 3 Article 4 2016 Family Formation and the Home Pamela Laufer-Ukeles University of Dayton School of Law Shelly Kreiczer-Levy College of Law and Business in Ramat Gan Follow this and additional works at: https://uknowledge.uky.edu/klj Part of the Family Law Commons Right click to open a feedback form in a new tab to let us know how this document benefits you. Recommended Citation Laufer-Ukeles, Pamela and Kreiczer-Levy, Shelly (2016) "Family Formation and the Home," Kentucky Law Journal: Vol. 104 : Iss. 3 , Article 4. Available at: https://uknowledge.uky.edu/klj/vol104/iss3/4 This Article is brought to you for free and open access by the Law Journals at UKnowledge. It has been accepted for inclusion in Kentucky Law Journal by an authorized editor of UKnowledge. For more information, please contact [email protected]. Family Formation and the Home Pamela Laufer-Ukeles' & Shelly Kreiczer-Levj INTRODUCTION' In this article, we consider the relevance of home sharing in family formation. When couples or groups of persons are recognized as families, they are afforded significant benefits and given certain obligations by the law.4 Families have their own category of laws, rights, and obligations.' Currently, the law of family formation and recognition is in a state of flux. Although in some respects the defining legal lines of the family have been well settled for centuries around blood and the formal legal ties of marriage and parenthood, in significant ways, the family form has been fundamentally altered over the past few decades. -

Racial and Ethnic Differences in Extended Family, Friendship, Fictive Kin, and Congregational Informal Support Networks
ROBERT JOSEPH TAYLOR University of Michigan ∗ LINDA M. CHATTERS University of Michigan ∗∗ AMANDA TOLER WOODWARD Michigan State University ∗∗∗ EDNA BROWN University of Connecticut Racial and Ethnic Differences in Extended Family, Friendship, Fictive Kin, and Congregational Informal Support Networks This study examined differences in kin and Black Caribbeans had larger fictive kin networks nonkin networks among African Americans, than non-Hispanic Whites, but non-Hispanic Caribbean Blacks (Black Caribbeans), and non- Whites with fictive kin received support from Hispanic Whites. Data are taken from the them more frequently than African Americans National Survey of American Life, a nation- and Black Caribbeans. The discussion notes ally representative study of African Americans, the importance of examining kin and nonkin net- Black Caribbeans, and non-Hispanic Whites. works, as well as investigating ethnic differences Selected measures of informal support from within the Black American population. family, friendship, fictive kin, and congregation/ church networks were utilized. African Ameri- Involvement with kin and nonkin is an cans were more involved in congregation net- essential component of daily life for the vast works, whereas non-Hispanic Whites were more majority of Americans. Family and friendship involved in friendship networks. African Ameri- support networks are important for coping cans were more likely to give support to extended with the ongoing stresses of daily life (e.g., family members and to have daily interaction Benin & Keith, 1995), providing a place to with family members. African Americans and live when confronting homelessness (Taylor, Chatters, & Celious, 2003), and in coping with physical and mental health problems School of Social Work, 1080 South University Avenue, Ann (Cohen, Underwood, & Gottlieb, 2000; Lincoln, Arbor, MI 48109-1106 ([email protected]). -
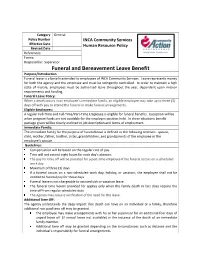
Funeral and Bereavement Leave Benefit Purpose/Introduction Funeral Leave Is a Benefit Extended to Employees of INCA Community Services
Category General Policy Number INCA Community Services Effective Date Human Resource Policy Revised Date References: Forms: Responsible: Supervisor Funeral and Bereavement Leave Benefit Purpose/Introduction Funeral leave is a benefit extended to employees of INCA Community Services. Leave represents money for both the agency and the employee and must be stringently controlled. In order to maintain a high state of morale, employees must be authorized leave throughout the year, dependent upon mission requirements and funding. Funeral Leave Policy: When a death occurs in an employee’s immediate family, an eligible employee may take up to three (3) days off with pay to attend the funeral or make funeral arrangements. Eligible Employees: A regular Full-Time and Full-Time/Part-Time Employee is eligible for funeral benefits. Exception will be when program funds are not available for the employee position held. In these situations benefit package given will be clearly outlined in job description and terms of employment. Immediate Family: The immediate family for the purpose of funeral leave is defined as the following relatives: spouse, child, mother, father, brother, sister, grandchildren, and grandparents of the employee or the employee’s spouse. Guidelines: Compensation will be based on the regular rate of pay. Time will not exceed eight hours for each day’s absence. The pay for time off will be prorated for a part-time employee if the funeral occurs on a scheduled work day. Maximum of three (3) days. If a funeral occurs on a non-scheduled work day, holiday, or vacation, the employee shall not be entitled to funeral pay for those days. -

The Reproductive Decision-Making of Women with Mitochondrial Disease
Julia Tonge Uncertain Existence: The reproductive decision-making of women with Mitochondrial Disease. Thesis submitted in fulfilment of the requirements for the degree of Doctor of Philosophy Institute of Neuroscience, Newcastle University October 2017 Abstract The aim of this thesis was to understand the process of reproductive decision- making in women with maternally inherited mitochondrial disease. It demonstrates the uncertainty fundamental to the experiences of women with mitochondrial DNA mutations (a subsection of women with mitochondrial disease). This uncertainty manifests in the personal accounts of their condition, as well as in relation to their reproductive decision-making. Twenty semi-structured qualitative interviews were conducted with eighteen women with mitochondrial DNA mutations, sampled via their connection to a mitochondrial disease specialist service in North East England. Retrospective, prospective and hypothetical questions were utilised in data collection. The data generated from the study, which was informed by constructivist grounded theory, can be organised into two central areas, both of which can be related back to uncertainty. The first area relates to how women harbour the desire for a healthy biologically related child. The second area features decision-making, which within the context of maternally inherited mitochondrial disease, is essentially the process by which women consolidate their desires for healthy children, and how they negotiate risk. The women’s accounts highlight social aspects of uncertainty that features in their reproductive decision-making, in contrast to the current literature that focuses on more clinical aspects of uncertainty. In addition, they also demonstrate how educational and employment institutions struggle to manage the uncertainty inherent in mitochondrial disease. -

Bereavement Leave
STATE OF CALIFORNIA - DEPARTMENT OF GENERAL SERVICE PERSONNEL OPERATIONS MANUAL SUBJECT: BEREAVEMENT LEAVE REPRESENTED EMPLOYEES Bereavement leave allows for up to three (3) eight-hour days (24 hours) per occurrence or three (3) eight-hour days (24 hours) in a fiscal year based on the family member. The following chart describes the family member and bereavement leave allowed per bargaining unit. Bargaining Unit Eligible family member - three (3) eight-hour days Eligible family member - three (3) (24 hours) per occurrence eight-hour days (24 hours) in a fiscal year 1, 4, 11, 14, 15 • Parent • Aunt • Stepparent • Uncle • Spouse • Niece • Domestic Partner • Nephew • Child • immediate family members of • Grandchild Domestic Partners • Grandparent • Brother • Sister • Stepchild • Mother-in-Law • Father-in-Law • Daughter-in-Law • Son-in-Law • Sister-in-Law • Brother-in-Law • any person residing in the immediate household 2 • Parent • Grandchild • Stepparent • Grandparent • Spouse • Aunt • Domestic Partner • Uncle • Child • Niece • Sister • Nephew • Brother • Mother-in-Law • Stepchild • Father-in-Law • any person residing in the immediate household • Daughter-in-Law • Son-in-Law • Sister-in-Law • Brother-in-Law • immediate family member 7 • Parent • Grandchild • Stepparent • Grandparent • Spouse • Aunt • Domestic Partner • Uncle STATE OF CALIFORNIA - DEPARTMENT OF GENERAL SERVICE PERSONNEL OPERATIONS MANUAL Bargaining Unit Eligible family member - three (3) eight-hour days Eligible family member - three (3) (24 hours) per occurrence eight-hour -

Intergenerational Estrangement Between Older Parents And
Every family: Intergenerational estrangement between older parents and their adult-children Kylie Beth Agllias BSW (Hons), UoN, AUST. A thesis submitted for the degree of Doctor of Philosophy (Social Work) University of Newcastle School of Humanities and Social Science May 2011 Declaration This thesis contains no material which has been accepted for the award of any other degree or diploma in any university or other tertiary institution and, to the best of my knowledge and belief, contains no material previously published or written by another person, except where due reference has been made in the text. I give consent to this copy of my thesis, when deposited in the University Library, being made available for loan and photocopying subject to the provisions of the Copyright Act 1968. Signed:............................................................. Date:.................................................. i Acknowledgements A mind that is stretched to a new idea never returns to its original dimension (Oliver W. Holmes) Some suggest the proof of a good thesis is when the examiner knows the student learnt something. However, the main lessons are the ones witnessed by supervisors, family, and friends, the lessons most often excluded from the text. I would like to thank the following people who witnessed and supported my doctoral journey and the associated life lessons: To my doctoral supervisors, mentors and colleagues, Professor Mel Gray and Doctor Jill Gibbons, I cannot thank you enough for your encouragement, guidance, and faith. You ‘saw me’ well before I knew myself. To my wonderfully generous, loving, amusing, and busy family, James, Kara, Paige, and Tyson, I love you. You are my world. -

How ASD Influences the Extended Family and Society
St. Catherine University SOPHIA Nursing Faculty Scholarship Nursing 12-2019 How ASD influences the extended family and society. Jocelyn Gorlin [email protected] Follow this and additional works at: https://sophia.stkate.edu/nursing_fac Part of the Pediatric Nursing Commons Recommended Citation *Gorlin, J. B. (2019). How ASD influences the extended family and society. In B. Turns, J. Ramisch, & J. Whiting (Eds.) Systemically Treating Autism: A Clinician’s Guide for Empowering Families. London and New York: Routledge Press. This Contribution to Book is brought to you for free and open access by the Nursing at SOPHIA. It has been accepted for inclusion in Nursing Faculty Scholarship by an authorized administrator of SOPHIA. For more information, please contact [email protected]. Systemically Treating Autism: A Guide for Empowering Families Routledge: Brie Turns, Julie Ramisch, and Jason Whiting Chapter 6: How ASD Influences the Extended Family and Society Jocelyn Bessette Gorlin PhD, MSN, CPNP Because families are nestled within the context of the extended families and society, when a child has ASD it affects much more than the nuclear family. This chapter reviews research that illuminates the effect of ASD on those who extend outside the immediate family and how this in turn influences the family. Specific questions include: 1. How do extended family members impact the family of the child with autism; and 2. How does the public including school personnel affect the family of the child with autism? Theoretical Framework of Autism Family Research: Much of the research on the families of children with autism and related disorders is founded on an ecological and quality of life (QOL) theoretical framework.