Call for Evidence Replies for Mitochondrial Review.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Placement of Children with Relatives
STATE STATUTES Current Through January 2018 WHAT’S INSIDE Placement of Children With Giving preference to relatives for out-of-home Relatives placements When a child is removed from the home and placed Approving relative in out-of-home care, relatives are the preferred placements resource because this placement type maintains the child’s connections with his or her family. In fact, in Placement of siblings order for states to receive federal payments for foster care and adoption assistance, federal law under title Adoption by relatives IV-E of the Social Security Act requires that they Summaries of state laws “consider giving preference to an adult relative over a nonrelated caregiver when determining a placement for a child, provided that the relative caregiver meets all relevant state child protection standards.”1 Title To find statute information for a IV-E further requires all states2 operating a title particular state, IV-E program to exercise due diligence to identify go to and provide notice to all grandparents, all parents of a sibling of the child, where such parent has legal https://www.childwelfare. gov/topics/systemwide/ custody of the sibling, and other adult relatives of the laws-policies/state/. child (including any other adult relatives suggested by the parents) that (1) the child has been or is being removed from the custody of his or her parents, (2) the options the relative has to participate in the care and placement of the child, and (3) the requirements to become a foster parent to the child.3 1 42 U.S.C. -

Kin Relationships
In H. T. Reis & S. Sprecher (Eds.), Encyclopedia of human relationships (pp. 951-954). Thousand Oaks, CA: Sage. Kin Relationships Kin relationships are traditionally defined as ties based on blood and marriage. They include lineal generational bonds (children, parents, grandparents, and great- grandparents), collateral bonds (siblings, cousins, nieces and nephews, and aunts and uncles), and ties with in-laws. An often-made distinction is that between primary kin (members of the families of origin and procreation) and secondary kin (other family members). The former are what people generally refer to as “immediate family,” and the latter are generally labeled “extended family.” Marriage, as a principle of kinship, differs from blood in that it can be terminated. Given the potential for marital break-up, blood is recognized as the more important principle of kinship. This entry questions the appropriateness of traditional definitions of kinship for “new” family forms, describes distinctive features of kin relationships, and explores varying perspectives on the functions of kin relationships. Questions About Definition Changes over the last thirty years in patterns of family formation and dissolution have given rise to questions about the definition of kin relationships. Guises of kinship have emerged to which the criteria of blood and marriage do not apply. Assisted reproduction is a first example. Births resulting from infertility treatments such as gestational surrogacy and in vitro fertilization with ovum donation challenge the biogenetic basis for kinship. A similar question arises for adoption, which has a history 2 going back to antiquity. Partnerships formed outside of marriage are a second example. Strictly speaking, the family ties of nonmarried cohabitees do not fall into the category of kin, notwithstanding the greater acceptance over time of consensual unions both formally and informally. -

Dna by the Entirety
DNA BY THE ENTIRETY Natalie Ram The law fails to accommodate the inconvenient fact that an individual’s identifiable genetic information is involuntarily and immutably shared with her close genetic relatives. Legal institutions have established that individuals have a cognizable interest in control- ling genetic information that is identifying to them. The Supreme Court recognized in Maryland v. King that the Fourth Amendment is impli- cated when arrestees’ DNA is analyzed, and the Genetic Information Nondiscrimination Act protects individuals from genetic discrimination in the employment and health-insurance markets. But genetic infor- mation is not like other forms of private or personal information because it is shared—immutably and involuntarily—in ways that are identifying of both the source and that person’s close genetic relatives. Standard approaches to addressing interests in genetic information have largely failed to recognize this characteristic, treating such infor- mation as individualistic. While many legal frames may be brought to bear on this problem, this Article focuses on the law of property. Specifically, looking to the law of tenancy by the entirety, this Article proposes one possible frame- work for grappling with the overlapping interests implicated in genetic identification and analysis. Tenancy by the entirety, like interests in shared identifiable genetic information, calls for the difficult task of conceptualizing two persons as one. The law of tenancy by the entirety thus provides a useful analytical framework for considering how legal institutions might take interests in shared identifiable genetic infor- mation into account. This Article examines how this framework may shape policy approaches in three domains: forensic identification, genetic research, and personal genetic testing. -

Family Formation and the Home Pamela Laufer-Ukeles University of Dayton School of Law
Kentucky Law Journal Volume 104 | Issue 3 Article 4 2016 Family Formation and the Home Pamela Laufer-Ukeles University of Dayton School of Law Shelly Kreiczer-Levy College of Law and Business in Ramat Gan Follow this and additional works at: https://uknowledge.uky.edu/klj Part of the Family Law Commons Right click to open a feedback form in a new tab to let us know how this document benefits you. Recommended Citation Laufer-Ukeles, Pamela and Kreiczer-Levy, Shelly (2016) "Family Formation and the Home," Kentucky Law Journal: Vol. 104 : Iss. 3 , Article 4. Available at: https://uknowledge.uky.edu/klj/vol104/iss3/4 This Article is brought to you for free and open access by the Law Journals at UKnowledge. It has been accepted for inclusion in Kentucky Law Journal by an authorized editor of UKnowledge. For more information, please contact [email protected]. Family Formation and the Home Pamela Laufer-Ukeles' & Shelly Kreiczer-Levj INTRODUCTION' In this article, we consider the relevance of home sharing in family formation. When couples or groups of persons are recognized as families, they are afforded significant benefits and given certain obligations by the law.4 Families have their own category of laws, rights, and obligations.' Currently, the law of family formation and recognition is in a state of flux. Although in some respects the defining legal lines of the family have been well settled for centuries around blood and the formal legal ties of marriage and parenthood, in significant ways, the family form has been fundamentally altered over the past few decades. -
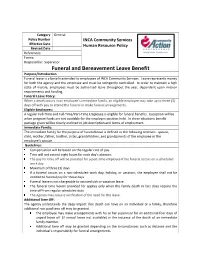
Funeral and Bereavement Leave Benefit Purpose/Introduction Funeral Leave Is a Benefit Extended to Employees of INCA Community Services
Category General Policy Number INCA Community Services Effective Date Human Resource Policy Revised Date References: Forms: Responsible: Supervisor Funeral and Bereavement Leave Benefit Purpose/Introduction Funeral leave is a benefit extended to employees of INCA Community Services. Leave represents money for both the agency and the employee and must be stringently controlled. In order to maintain a high state of morale, employees must be authorized leave throughout the year, dependent upon mission requirements and funding. Funeral Leave Policy: When a death occurs in an employee’s immediate family, an eligible employee may take up to three (3) days off with pay to attend the funeral or make funeral arrangements. Eligible Employees: A regular Full-Time and Full-Time/Part-Time Employee is eligible for funeral benefits. Exception will be when program funds are not available for the employee position held. In these situations benefit package given will be clearly outlined in job description and terms of employment. Immediate Family: The immediate family for the purpose of funeral leave is defined as the following relatives: spouse, child, mother, father, brother, sister, grandchildren, and grandparents of the employee or the employee’s spouse. Guidelines: Compensation will be based on the regular rate of pay. Time will not exceed eight hours for each day’s absence. The pay for time off will be prorated for a part-time employee if the funeral occurs on a scheduled work day. Maximum of three (3) days. If a funeral occurs on a non-scheduled work day, holiday, or vacation, the employee shall not be entitled to funeral pay for those days. -

The Reproductive Decision-Making of Women with Mitochondrial Disease
Julia Tonge Uncertain Existence: The reproductive decision-making of women with Mitochondrial Disease. Thesis submitted in fulfilment of the requirements for the degree of Doctor of Philosophy Institute of Neuroscience, Newcastle University October 2017 Abstract The aim of this thesis was to understand the process of reproductive decision- making in women with maternally inherited mitochondrial disease. It demonstrates the uncertainty fundamental to the experiences of women with mitochondrial DNA mutations (a subsection of women with mitochondrial disease). This uncertainty manifests in the personal accounts of their condition, as well as in relation to their reproductive decision-making. Twenty semi-structured qualitative interviews were conducted with eighteen women with mitochondrial DNA mutations, sampled via their connection to a mitochondrial disease specialist service in North East England. Retrospective, prospective and hypothetical questions were utilised in data collection. The data generated from the study, which was informed by constructivist grounded theory, can be organised into two central areas, both of which can be related back to uncertainty. The first area relates to how women harbour the desire for a healthy biologically related child. The second area features decision-making, which within the context of maternally inherited mitochondrial disease, is essentially the process by which women consolidate their desires for healthy children, and how they negotiate risk. The women’s accounts highlight social aspects of uncertainty that features in their reproductive decision-making, in contrast to the current literature that focuses on more clinical aspects of uncertainty. In addition, they also demonstrate how educational and employment institutions struggle to manage the uncertainty inherent in mitochondrial disease. -

Bereavement Leave
STATE OF CALIFORNIA - DEPARTMENT OF GENERAL SERVICE PERSONNEL OPERATIONS MANUAL SUBJECT: BEREAVEMENT LEAVE REPRESENTED EMPLOYEES Bereavement leave allows for up to three (3) eight-hour days (24 hours) per occurrence or three (3) eight-hour days (24 hours) in a fiscal year based on the family member. The following chart describes the family member and bereavement leave allowed per bargaining unit. Bargaining Unit Eligible family member - three (3) eight-hour days Eligible family member - three (3) (24 hours) per occurrence eight-hour days (24 hours) in a fiscal year 1, 4, 11, 14, 15 • Parent • Aunt • Stepparent • Uncle • Spouse • Niece • Domestic Partner • Nephew • Child • immediate family members of • Grandchild Domestic Partners • Grandparent • Brother • Sister • Stepchild • Mother-in-Law • Father-in-Law • Daughter-in-Law • Son-in-Law • Sister-in-Law • Brother-in-Law • any person residing in the immediate household 2 • Parent • Grandchild • Stepparent • Grandparent • Spouse • Aunt • Domestic Partner • Uncle • Child • Niece • Sister • Nephew • Brother • Mother-in-Law • Stepchild • Father-in-Law • any person residing in the immediate household • Daughter-in-Law • Son-in-Law • Sister-in-Law • Brother-in-Law • immediate family member 7 • Parent • Grandchild • Stepparent • Grandparent • Spouse • Aunt • Domestic Partner • Uncle STATE OF CALIFORNIA - DEPARTMENT OF GENERAL SERVICE PERSONNEL OPERATIONS MANUAL Bargaining Unit Eligible family member - three (3) eight-hour days Eligible family member - three (3) (24 hours) per occurrence eight-hour -

R. Brumbaugh Kinship Analysis: Methods, Results and the Sirionó Demonstration Case
R. Brumbaugh Kinship analysis: methods, results and the Sirionó demonstration case In: Bijdragen tot de Taal-, Land- en Volkenkunde 134 (1978), no: 1, Leiden, 1-29 This PDF-file was downloaded from http://www.kitlv-journals.nl Downloaded from Brill.com10/02/2021 02:22:46PM via free access ROBERT C. BRUMBAUGH KINSHIP ANALYSIS : METHODS, RESULTS,AND THE SIRIONO DEMONSTRATION CASE A likely exarnple of 'cultural devolution', the Sirionó hunters and gatherers of Bolivia were best known for the whistle-talk they have developed until Needham (1962) drew attention to their kinship system, which he cited as a rare case of matrilineal prescriptive alliance. His interpretation was subsequently weakened as it becarne clear that there is no evidence in the Sirionó ethnography (Holmberg 1950) for social correlates which are an essential part of the 'prescriptive alliance' scheme (Needham 1962, 1964). -Meanwhile Scheffler and Lounsbury had chosen the Sirionó system as the demonstration case for a new approach to kinship, called 'trans- formational analysis', which aims to discover the underlying cognitive structure of the system through semantic analysis. The Sirionó case study (1971) contrasted the results of this method with the failure of Needharn's model; and since prescriptive alliance theory itself is Need- ham's modified version of Lévi-Strauss' kinship theory (which I will cal1 'structural' theory), the case seemed to vindicate their semantic approach where 'structuralism' had already proved inadequate. The purpose of this paper is to compare -

Domestic and International Adoption: Strategies to Improve Behavioral Health Outcomes for Youth and Their Families ACKNOWLEDGMENTS
JANUARY 28, 2015 Domestic and International Adoption: Strategies to Improve Behavioral Health Outcomes for Youth and Their Families ACKNOWLEDGMENTS We would like to thank the following people for their participation in the planning committee for the Domestic and International Adoption: Strategies to Improve Behavioral Health Outcomes for Youth and Their Families meeting. • Terry Baugh, Kidsave • Heather Burke, Centers for Disease Control and Prevention • Wilson Compton, National Institute on Drug Abuse, National Institutes of Health • Angela Drumm, American Institutes for Research • Kelly Fisher, Administration for Children and Families • Robert Freeman, National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health • Amy Goldstein, National Institute of Mental Health, National Institutes of Health • Valerie Maholmes, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health • Sonali Patel, Administration for Children and Families • Eve Reider, National Institute on Drug Abuse, National Institutes of Health • Elizabeth Robertson, National Institute on Drug Abuse, National Institutes of Health • Lisa Rubenstein, Substance Abuse and Mental Health Services Administration • Kate Stepleton, Administration for Children and Families • Phil Wang, National Institute of Mental Health, National Institutes of Health • Mary Bruce Webb, Administration for Children and Families BACKGROUND On August 29–30, 2012, the Substance Abuse and Mental Health Services Administration (SAMHSA) -

Paid Leave Due to a Serious Illness in the Immediate Family Policy
Paid Leave Due to a Serious Illness in the Immediate Family Policy Effective date: 01/01/2003 Revision date: 12/01/2019 Purpose The purpose of the Paid Leave Due to a Serious Illness in the Immediate Family Policy (“Policy”) is to provide eligible employees paid time off to attend to a serious illness or health condition for an employee’s Immediate Family Member. The Policy does not apply to time off for usual childhood or adult illness of an Immediate Family Member. Eligibility The Policy applies to all regular full-time and regular part-time employees on the U.S. payroll. Temporary or intermittent employees are not eligible for leave provided by the Policy. To assist with employee eligibility determination, refer to U.S. Employment Status Policy. Note: Employees represented by a collective bargaining agreement are eligible where provided for under the terms of an applicable collective bargaining agreement. Definitions Immediate Family Member is defined as the employee’s: • Spouse: One of the parties of a legal marriage, including common law marriage, where it is recognized. • Domestic Partner: As defined by applicable state law or the Company’s benefit plans. • Son or daughter: A biological, adopted, or foster child, a stepchild or a legal ward of the employee or the employee’s spouse/domestic partner, or a child of whom the employee or the employee’s spouse/domestic partner has legal responsibility (loco parentis). • Parents: A biological, adoptive, step or foster father or mother, or any other individual who has the legal responsibility (loco parentis) to the employee or employee’s spouse/domestic partner when the employee or employee’s spouse/domestic partner was a son or daughter as defined above. -

Families and the Church in the 21St Century: the Meaning of Kinship Bonds
Families and the church in the 21st century: the meaning of kinship bonds REVISED VERSION May 2014 1 FAMILIES AND THE CHURCH IN THE 21ST CENTURY: THE MEANING OF KINSHIP BONDS 1. Introduction The realities of family relationships within Scottish society have changed profoundly over the past few decades. This report seeks to encourage the church to be aware of the effects these changes may have on the communities which we serve. Over the past half century there has been a dramatic change in family structure. There is a trend away from marriage resulting in a minority of people in Scotland being married. (The 2011 census showed that just over 45% of people aged 16 and over in Scotland are married). About a third of children in Scotland are in single parent families. Other family structures include complex step- parent relationships and there is an increasing reliance on grandparents for day to day childcare, not just occasional babysitting. The expanding availability of methods of assisted conception means that children born as a result of these methods may have parents responsible for their care who are distinct from their biological parents. Meanwhile, children currently offered for adoption are no longer typically healthy infants given up at birth, but may be toddlers and older children from homes affected by alcohol, drugs or other complex social problems. 2. ‘A Child of our Own’ Parents’ desire to have children of their own, or at least as much ‘of their own’ as possible, is the driving force behind the growth and popularity of fertility clinics. -

To Grieve the Death of the Child. Employees May Use Accrued Leave Benefits to Remain in Pay Status While Taking Leave Under This Act
University of Illinois Policy and Rules POLICY 11 APPROVED AND UNAPPROVED ABSENCES Rule 11.05 - Funeral Leave Employees in trainee, learner, apprentice, provisional, or status appointments will be granted upon request paid leave of three (3) scheduled work days to attend the funeral and for travel and bereavement time, upon the death of a member of the employee’s immediate family or upon the death of a member of the household; and one (1) day to attend the funeral or memorial service of a relative other than the above who is not a member of the employee’s household. Under the Illinois Child Bereavement Leave Act, employees otherwise eligible for Family and Medical Leave under Rule 11.07 are eligible for an additional seven (7) unpaid days to attend the funeral, or an alternative to a funeral; to make arrangements necessitated by the death of the child; or to grieve the death of the child. Employees may use accrued leave benefits to remain in pay status while taking leave under this Act. The Act does not create a right for an employee to take unpaid leave that exceeds the unpaid leave time available under FMLA; therefore, employees who have exhausted their 12-week FMLA entitlement may not take the additional seven days under this Act. Leave provided under this Act must be used within 60 days after the employee receives notice of the death of his/her child. If an employee suffers the death of more than one child in any 12-month period, the employee is entitled to take up to six weeks of unpaid bereavement leave in the 12-month period.