The Off C Al Journal of the Azerba Jan Med Cal Assoc at On
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
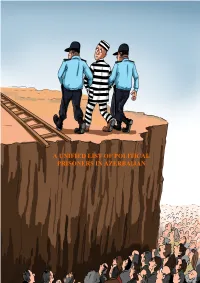
A Unified List of Political Prisoners in Azerbaijan
A UNIFIED LIST OF POLITICAL PRISONERS IN AZERBAIJAN A UNIFIED LIST OF POLITICAL PRISONERS IN AZERBAIJAN Covering the period up to 25 May 2017 Table of Contents INTRODUCTION..........................................................................................................4 DEFINITION OF POLITICAL PRISONERS...............................................................5 POLITICAL PRISONERS.....................................................................................6-106 A. Journalists/Bloggers......................................................................................6-14 B. Writers/Poets…...........................................................................................15-17 C. Human Rights Defenders............................................................................17-18 D. Political and social Activists ………..........................................................18-31 E. Religious Activists......................................................................................31-79 (1) Members of Muslim Unity Movement and those arrested in Nardaran Settlement...........................................................................31-60 (2) Persons detained in connection with the “Freedom for Hijab” protest held on 5 October 2012.........................60-63 (3) Religious Activists arrested in Masalli in 2012...............................63-65 (4) Religious Activists arrested in May 2012........................................65-69 (5) Chairman of Islamic Party of Azerbaijan and persons arrested -

MONGOLIA: Systematic Country Diagnostic Public Disclosure Authorized
MONGOLIA: Systematic Country Diagnostic Public Disclosure Authorized Public Disclosure Authorized Public Disclosure Authorized Public Disclosure Authorized Acknowledgements This Mongolia Strategic Country Diagnostic was led by Samuel Freije-Rodríguez (lead economist, GPV02) and Tuyen Nguyen (resident representative, IFC Mongolia). The following World Bank Group experts participated in different stages of the production of this diagnostics by providing data, analytical briefs, revisions to several versions of the document, as well as participating in several internal and external seminars: Rabia Ali (senior economist, GED02), Anar Aliyev (corporate governance officer, CESEA), Indra Baatarkhuu (communications associate, EAPEC), Erdene Badarch (operations officer, GSU02), Julie M. Bayking (investment officer, CASPE), Davaadalai Batsuuri (economist, GMTP1), Batmunkh Batbold (senior financial sector specialist, GFCP1), Eileen Burke (senior water resources management specialist, GWA02), Burmaa Chadraaval (investment officer, CM4P4), Yang Chen (urban transport specialist, GTD10), Tungalag Chuluun (senior social protection specialist, GSP02), Badamchimeg Dondog (public sector specialist, GGOEA), Jigjidmaa Dugeree (senior private sector specialist, GMTIP), Bolormaa Enkhbat (WBG analyst, GCCSO), Nicolaus von der Goltz (senior country officer, EACCF), Peter Johansen (senior energy specialist, GEE09), Julian Latimer (senior economist, GMTP1), Ulle Lohmus (senior financial sector specialist, GFCPN), Sitaramachandra Machiraju (senior agribusiness specialist, -

Andy Patrick CV
AP Curriculum Vitae Current Position 2013-2016 Principal, Andy Patrick Consulting, San Francisco, CA The consulting practice is focused on strategic planning across all functions of technology start-ups including branding, product development, social media, marketing and sales, revenue growth, organizational development, online product vision, funding, partnerships and business development strategies. Client projects have included: - creating and implementing a partnership program for the largest live online learning platform in the creative industry; - development of a launch plan and funding strategy for an app; - creation of a product road map for an industry-leading SaaS platform; - revamping the business model and marketing plan for an online platform; - comprehensive branding, product development and business modeling for a crowdfunding platform; - mentoring four CEOs. This work leverages twenty years of experience in leadership positions in the Internet, e-commerce, entrepreneurial, photography and creative professional sectors. Career History 2005-2013 Co-Founder, President & CEO, liveBooks, Inc., San Francisco, CA Within one year of launch, liveBooks created a paradigm shift for how creative professionals market themselves. Became the world’s leader in the design and development of online portfolio websites for professional photographers. Responsible for establishing the overall vision and leadership across all functions of the organization including people, branding, marketing, business development, product strategy and technology. Actively involved in establishing an office in Romania. Interviewed and hired over thirty employees in Romania and an additional forty employees in the United States. Profitable in year three on revenues of $4.6M, and in 2008 successfully led a business model transition to SaaS, attracting $7M in outside funding to bridge the transition. -

The West's Limited Legacy
Number 118 • Mar / Apr 2012 • $8.95 Jacob Heilbrunn Beinart’s Woeful Warning John Campbell Struggle in Nigeria Symposium Wilson’s Ghost David M. Shribman The Varied Life of Ike www.nationalinterest.org Gian P. Gentile Who Lost Vietnam? Afghanistan Past and Future: THE NATIONAL INTEREST The West’s Limited Legacy ◊ NUMBER118 ◊ MAR / APR 2012 A Stubborn Land by Michael Hart Britain’s Afghan Agony by Seth G. Jones a) more oil b) more natural gas c) more wind d) more solar e) more biofuels f) energy efficiency g) all of the above To enhance America’s energy and economic security, we must secure more of the energy we consume. That means expanding the use of wind, solar and biofuels, as well as opening new offshore areas to oil and gas production. Through efficiency and increased domestic production, we can reduce the flow of dollars overseas and invest those funds at home to create new jobs and billions in new government revenue. BP is the nation’s largest energy investor, and we’d like to do more. Learn more at bp.com/us. beyoned p troleum® © 2009 BP Products North America Inc. Untitled-1 1 8/7/09 2:34:08 PM Client: BP Safety: 6” x 9” Mechanical Scale: 100% Campaign: BP Energy Security Trim: 7” x 10” Format: Full Page 4/C Ad #: BP-09-1N R2 Bleed: 7.5” x 10.5” Printer: Ad Title: Tickmark - More of the above (with copy) Media Vendor / Publication: Version/Revision #: V2 The National Interest / Foreign Affairs Date Modified: March 31, 2009 Operator: rt/AC/rt Schawk Docket #:886691-05 Number 118 . -

2009 Trial Monitoring Report Azerbaijan N a J I a B R E Z A
2009 TRIAL MONITORING REPORT AZERBAIJAN REPOR 2009 TRIAL T AZERBAIJAN MONIT ORING 2009 TRIAL MONITORING REPORT AZERBAIJAN © OSCE Office in Baku - i - Table of Contents Acknowledgments ........................................................................................................................................ ii List of Abbreviations.................................................................................................................................... 1 Introduction .................................................................................................................................................. 2 Scope of the Report. Methodology............................................................................................................... 6 I. Observance of Fair Trial and Rights of the Defendants....................................................................... 9 1.1. The Right to a Public Hearing..................................................................................................... 9 1.2. Presence at Hearings: Defendant, Defence Counsel and Prosecutor ........................................ 11 1.3. The Right to be Informed of the Charges and the Right not to Incriminate Oneself ................ 13 1.4. Duty to Effectively Investigate Allegations of Ill-Treatment ................................................... 21 1.5. The Right to an Independent and Impartial Tribunal................................................................ 25 1.6. The Right to be Presumed Innocent......................................................................................... -

Download Our 2018 Report (11.3 MB PDF)
OUR DREAM OUR VISION OUR SOLUTION To benefit the community at large by To encourage a healthy To create an interdisciplinary fostering greater social harmony and exchange of ideas inspired Iranian Studies degree offered IRANIAN STUDIES AT USC progress through an accurate and objective by academia across by USC with support from the understanding of Iran and Iranian Culture. Southern California cultures. Farhang Foundation community. TABLE OF CONTENTS OVERVIEW 38 Iran Through Books at the 2016 L.A. Times Festival of Books The Iranian Studies Initiative has brought together a 6 Why Iranian Studies? 39 Iranian Music Workshop (Tasnif) by Kourosh Taghavi 7 Why Now? 40 Maryama Band: Secret Diaries of a Middle Eastern Mermaid forward-thinking university and a vibrant community. 8 Why Farhang Foundation? 41 A Tribute to Abbas Kiarostami 9 Why USC? 42 Photographic Self-Representation in Iran: A Lecture It has energized and invigorated our program and by Prof. Ali Behdad ACCOMPLISHMENTS 43 Fifth Annual PACSA Celebration Night with Musical 10 Timeline Guest Karmandan allowed us to imagine new horizons for Iranian 12 Class Schedule 44 The Intersection of Past & Present in Iranian Art: A Lecture by Dr. Linda Komaroff 13 Student Enrollment 45 Creative Writing Workshop: Hossein Abkenar Studies at USC and beyond. The commitment and 14 Project Phases 46 USC Iranian Studies Major Program Signing Celebration 15 Meet Two of Our Seniors 48 Iran Through Books at the 2017 L.A. Times Festival of Books dedication of those involved bodes well for the future. EVENTS -

UNICEF Turkey Humanitarian Situation Report February 2019
UNICEF Turkey Humanitarian Situation Report February 2019 TURKEY CO Humanitarian Situation Report #30 © UNICEF/Yurtsever 1 – 28 FEBRUARY 2019 SITUATION IN NUMBERS February 2019 Highlights • In February, UNICEF supported the Turkish government’s efforts to 1,684,739 children affected out of prevent and address child marriage, with a focus on capacity building. Approximately 460 staff and service providers from the government, 4,007,934 armed forces, women’s shelters and violence prevention centres were people affected trained on how to better identify and respond to child marriage cases. UNICEF 2018 Appeal • UNICEF also focused on expanding access to non-formal education for US $239.7 million out-of-school refugee children. Nearly 1,100 children registered for the Accelerated Learning Programme and more than 400 registered for Funding Status Turkish language courses. Outreach campaigns also identified 10,500 in millions of USD children (40% of whom were out of school) and referred them to relevant education opportunities. $2 (1%) • UNICEF Turkey is 46% funded (as of 15 March 2019) under the 2019 3RP appeal (including carry-over from the previous year), with only US $2 $108.3 $239.7 (45%) million received in 2019. US $10 million is urgently required to fund $129.4 required (55%) essential interventions for vulnerable refugee children in education and child protection. Situation Overview & Humanitarian Needs Turkey remains home to the largest registered refugee population in the world. Over 4 million refugees and asylum-seekers are registered in Turkey, Funds received Carry-forward amount Gap of whom nearly 1.7 million are children.1 More than 3.6 million Syrians – including over 1.5 million children – are under temporary protection, 96 per cent of whom live in host communities across the country. -

Caucasus Strategic Perspectives
HIGHLIGHT OF JOURNAL The role of ideology in mass atrocities: The case of the conflict between Armenia and Azerbaijan Vugar Gurbanov CAUCASUS STRATEGIC PERSPECTIVES Volume 1 • Issue 2 • Winter 2020 Armenia and Azerbaijan: CAUCASUS Between Failed Peace and War STRATEGIC PERSPECTIVES - ARTICLES COMMENTARIES Geopolitics and the Second Karabakh War The Gordian Knot of the Armenia–Azerbaijan Damjan Krnjevic Miskovic Conflict and the Second Karabakh War: Conclusions and Reflections Western Blind Spot in the South Caucasus: Esmira Jafarova Chronicle of a War Foretold Robert M. Cutler Turkey’s Presence, Involvement and Engagement in the Armenia–Azerbaijan Conflict: A Reflection on Volume 1 • Issue 2 Winter 2020 Economic Potential of the Liberated Azerbaijani–Turkish Relations Territories of Azerbaijan: A Brief Overview Ayça Ergun Rovshan Ibrahimov Violations of International Humanitarian Armenia–Azerbaijan Conflict: Law by Armenia in the Second Karabakh war The Failure of Multilateral Diplomacy Nizami Safarov and Najiba Mustafayeva Murad Muradov Ukrainian Discourse on the Assessing Damage Caused by Illegal Armenia–Azerbaijan Conflict Activities of Armenia to Azerbaijan in the Liberated Anna Korzeniowska-Bihun (Formerly Occupied) Territories Javid Alyarli and Arzu Abbasova International Response to the Second Karabakh War Nina Miholjcic BOOK REVIEW SERIES: Exculpation of Armenian terrorism under guise of the ‘Armenian martyr’ reviewed by Murad Muradov Sama Baghirova “The Light that Failed: A Reckoning” (authored by Ivan Krastev and Stephen Holmes) JOURNALISTIC DISPATCH * reviewed by Mahammad Mammadov Dispatch from the Conflict Zone during “The Brussels Effect: How the European Union Azerbaijan’s Patriotic War Rules the World” (authored by Anu Bradford) Elmira Musazadeh Volume 1 • Issue 2 • Winter 2020 Armenia and Azerbaijan: Between Failed Peace and War CAUCASUS STRATEGIC PERSPECTIVES Vol. -

Annenberg Space for Photography Announces Upcoming Iris Nights Lecture Series and Skylight Studios Installation for New Exhibition
ANNENBERG SPACE FOR PHOTOGRAPHY ANNOUNCES UPCOMING IRIS NIGHTS LECTURE SERIES AND SKYLIGHT STUDIOS INSTALLATION FOR NEW EXHIBITION April 23 – August 21, 2016 LOS ANGELES, CA (April 21, 2016)— The Annenberg Space for Photography has announced a series of special events and programming presented in conjunction with the exhibition REFUGEE, on view at the Photography Space from April 23 through August 21, 2016. For REFUGEE, the Annenberg Foundation commissioned five internationally acclaimed photographers—Lynsey Addario, Omar Victor Diop, Graciela Iturbide, Martin Schoeller and Tom Stoddart—to document the lives of the forcibly displaced on five continents. The programming includes a livestreamed panel discussion featuring REFUGEE exhibition photographers, the popular IRIS Nights Lecture Series and the New Americans installation at Skylight Studios. LIVESTREAM OF CRISIS IN FOCUS PANEL DISCUSSION In Crisis in Focus, three of REFUGEE’s photographers will discuss their experiences while on assignment for the exhibition. Lynsey Addario will discuss documenting the Rohingya people — a disenfranchised Muslim population in the predominantly Buddhist nation of Myanmar. Omar Victor Diop will share his experiences photographing refugees from the Central African Republic who were forced to flee to Cameroon. Martin Schoeller will describe working with refugees who have recently resettled in the U.S. UN Deputy High Commissioner for Refugees Kelly Clements will open the discussion with a brief overview of the crisis, and NPR's Eleanor Beardsley will moderate the panel. REFUGEE photographer Tom Stoddart and the exhibition documentary filmmakers from Tiger Nest Films will also participate in a Q & A following the panel. Crisis in Focus will be livestreamed Friday, April 22 at 12:45PM PT. -

500 Most Influential Muslims of 2009
THE 500 MOST INFLUENTIAL MUSLIMS = 2009 first edition - 2009 THE 500 MOST INFLUENTIAL MUSLIMS IN THE WORLD = 2009 first edition (1M) - 2009 Chief Editors Prof John Esposito and Prof Ibrahim Kalin Edited and Prepared by Ed Marques, Usra Ghazi Designed by Salam Almoghraby Consultants Dr Hamza Abed al Karim Hammad, Siti Sarah Muwahidah With thanks to Omar Edaibat, Usma Farman, Dalal Hisham Jebril, Hamza Jilani, Szonja Ludvig, Adel Rayan, Mohammad Husni Naghawi and Mosaic Network, UK. all photos copyright of reuters except where stated All rights reserved. No part of this book may be used or reproduced in any manner without the prior consent of the publisher. © the royal islamic strategic studies centre, 2009 أ �� ة � � ن ة � �ش� ة الم�م��لك�� ا �ل� ر د ��ة�� ا ل�ها �مة�� ة � � � أ ة � ة ة � � ن ة �� ا �ل� ���د ا �ل�د �ى د ا � � ال�مك� �� ا �ل� ل�ط� �� ر م أ ة ع ر ن و ة (2009/9/4068) ة � � ن � � � ة �ة ن ن ة � ن ن � � ّ ن � ن ن ة�����ح�م� ال�م�أ ��ل� كل� �م� ال�م��س�أ � ���� ا ��لها �ل� ���� �ع ن م�حة� � �م�ط��ه�� � �ل� ���ه�� �ه�� ا ال�م�ط��� �ل و أ �ل و وة وة � أ أوى و ة نأر ن � أ ة ���ة ة � � ن ة � ة � ة ن � . �ع� ر ا �ةى د ا �ر � الم ك��ن �� ا �ل�و ل�ط�ة�� ا �و ا �ةى ن��ه�� �ح �ل�و�مة�� ا �ر�ى ISBN 978-9957-428-37-2 املركز امللكي للبحوث والدراسات اﻹسﻻمية )مبدأ( the royal islamic strategic studies centre The Prince Alwaleed Bin Talal Center for Muslim-Christian Understanding Edmund A. -

Download File
UNICEF Turkey Humanitarian Situation Report January 2019 TURKEY CO Humanitarian Situation Report #29 @UNICEF© Turkey/2017/Rich UNICEF/Feyzioglu 1 – 31 JANUARY 2019 SITUATION IN NUMBERS January 2019 Highlights • At the start of 2019, Turkey continues to host the largest registered 1,778,148 children affected out of refugee population in the world with over 4 million refugees and asylum- seekers registered, of whom over 1.7 million are children. 4,012,571 people affected • UNICEF supported the Ministry of Family, Labour and Social Services (MoFLSS) on implementation of the Child Development and Support Programme. A total of 71 MoFLSS technical staff were trained as master UNICEF 2018 Appeal trainers and will in turn train additional 1,000 social service personnel, US $239.7 million working in 1,200 child care homes caring for approximately 12,000 Turkish and refugee children. • In January 2019, 487,089 refugee children benefitted from the Conditional Cash Transfer for Education (CCTE) payment, including Funding Status 1,066 children enrolled in the Accelerated Learning Programme. Families in millions of USD also received a TL 100 "Back to School" top-up payment to help them meet additional expenses at the beginning of the new semester $0 (0%) Situation Overview & Humanitarian Needs At the start of 2019, Turkey continues to host the largest registered refugee $108.3 $239.7 (45%) $131.4 required population in the world, with over 4 million refugees and asylum-seekers (55%) registered in Turkey, of whom over 1.7 million are children. Over 3.6 million Syrians – including 1.6 million children – are under temporary protection, 96 per cent of whom live in host communities across the country.1 Turkey also continues to host a sizable non-Syrian refugee community. -

Webographie Pp
Reza Philanthrope, idéaliste, humaniste, architecte dans l’âme et célèbre photojournaliste notamment pour le National Geographic, Reza parcourt le monde depuis plus de trente ans. «Le monde est mon champ de vision. De la guerre à la paix, de l’ineffable aux instants de poésie, mes images se veulent des témoignages de notre humanité sur les routes du monde.» Reza Sommaire Webographie pp. 01 - 04 Bibliographie : réseau des bibliothèques de Toulouse pp. 05 - 07 Webographie Reza : site officiel http://reza.photo/#1 La photographie pour changer le monde | Reza (A écouter): Philanthrope, idéaliste, humaniste, architecte dans l’âme et célèbre photojournaliste, Reza parcourt le monde depuis plus de trente ans. Ses témoignages visuels sont diffusés dans les médias internationaux, mais aussi sous forme de livres, d’expositions et de documentaires.Plus qu’un photographe, Reza met l’éducation visuelle informelle des jeunes et des femmes de sociétés civiles fragilisées au service d’un monde meilleur, formant les populations aux métiers de l'information et de la communication, et menant des actions de formation au langage de l'image sous différentes formes (concrète et virtuelle) à l’international, à travers son association Les Ateliers Reza.Reza expose dans le monde entier. Il vit à Paris depuis 38 ans. https://www.youtube.com/watch?v=LrYwAP95V_k Novembre 2020 1 Parvaz, l'envol de Reza (A écouter): Dans les années 70, le jeune lycéen iranien Reza dénonce une injustice dans le journal de son établissement. Convoqué au commissariat, il est interrogé et même frappé pour avoir osé dire la vérité. Le journal s'appelle Parvaz ("L'Envol").