Cvs Caremark ® Maintenance Drug List
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Long-Term Statin Use and Risk of Ductal and Lobular Breast Cancer Among Women 55 to 74 Years of Age
Published OnlineFirst July 5, 2013; DOI: 10.1158/1055-9965.EPI-13-0414 Cancer Epidemiology, Research Article Biomarkers & Prevention Long-Term Statin Use and Risk of Ductal and Lobular Breast Cancer among Women 55 to 74 Years of Age Jean A. McDougall1, Kathleen E. Malone1, Janet R. Daling1, Kara L. Cushing-Haugen1, Peggy L. Porter1,2, and Christopher I. Li1 Abstract Background: Mechanistic studies largely support the chemopreventive potential of statins. However, results of epidemiologic studies investigating statin use and breast cancer risk have been inconsistent and lacked the ability to evaluate long-term statin use. Methods: We used data from a population-based case–control study of breast cancer conducted in the Seattle–Puget Sound region to investigate the relationship between long-term statin use and breast cancer risk. Nine hundred sixteen invasive ductal carcinoma (IDC) and 1,068 invasive lobular carcinoma (ILC) cases in patients 55 to 74 years of age diagnosed between 2000 and 2008 were compared with 902 control women. All participants were interviewed in-person and data on hypercholesterolemia and all episodes of lipid-lowering medication use were collected through a structured questionnaire. We assessed the relationship between statin use and IDC and ILC risk using polytomous logistic regression. Results: Current users of statins for 10 years or longer had a 1.83-fold increased risk of IDC [95% confidence interval (CI): 1.14–2.93] and a 1.97-fold increased risk of ILC (95% CI: 1.25–3.12) compared with never users of statins. Among women diagnosed with hypercholesterolemia, current users of statins for 10 years or longer had more than double the risk of both IDC (OR: 2.04, 95% CI: 1.17–3.57) and ILC (OR: 2.43, 95% CI: 1.40–4.21) compared with never users. -

Intraocular Pressure Rise After Phacoemulsification Prophylactic
British Journal of Ophthalmology 1995; 79: 809-813 809 Intraocular pressure rise after phacoemulsification Br J Ophthalmol: first published as 10.1136/bjo.79.9.809 on 1 September 1995. Downloaded from with posterior chamber lens implantation: effect of prophylactic medication, wound closure, and surgeon's experience Thomas G Bomer, Wolf-Dietrich A Lagreze, Jens Funk Abstract pressure rises usually occur between 6 and 8 Aims-A prospective clinical trial was hours after surgery.6 carried out to evaluate the effect of Various antiglaucomatous agents have been prophylactic medication, the technique of used to prevent the intraocular pressure rise wound closure, and the surgeon's experi- after cataract extraction. Oral acetazolamide15 16 ence on the intraocular pressure rise after and topical timolol'6-19 lowered the pressure cataract extraction. rise in the early period after intracapsular and Methods-In 100 eyes, the intraocular extracapsular cataract extraction. Levobunolol pressure was measured before as well as proved to be superior to timolol 4-7 hours 2-4, 5-7, and 22-24 hours after phaco- after extracapsular cataract extraction.20 Apra- emulsification and posterior chamber lens clonidine lowered the intraocular pressure rise implantation. Each of 25 patients received after uncomplicated phacoemulsification21 and either 1% topical apraclonidine, 0.5%/o extracapsular cataract extraction22 23 when topical levobunolol, 500 mg oral acetazo- given 30 minutes to 1 hour before surgery, lamide, or placebo. Forty four eyes were whereas immediate postoperative treatment operated with sclerocorneal sutureless with apraclonidine was ineffective.22 24 Miotics tunnel and 56 eyes with corneoscleral are frequently used to promote miosis and incision and suture. -

Brimonidine Tartrate; Brinzolamide
Contains Nonbinding Recommendations Draft Guidance on Brimonidine Tartrate ; Brinzolamide This draft guidance, when finalized, will represent the current thinking of the Food and Drug Administration (FDA, or the Agency) on this topic. It does not establish any rights for any person and is not binding on FDA or the public. You can use an alternative approach if it satisfies the requirements of the applicable statutes and regulations. To discuss an alternative approach, contact the Office of Generic Drugs. Active Ingredient: Brimonidine tartrate; Brinzolamide Dosage Form; Route: Suspension/drops; ophthalmic Strength: 0.2%; 1% Recommended Studies: One study Type of study: Bioequivalence (BE) study with clinical endpoint Design: Randomized (1:1), double-masked, parallel, two-arm, in vivo Strength: 0.2%; 1% Subjects: Males and females with chronic open angle glaucoma or ocular hypertension in both eyes. Additional comments: Specific recommendations are provided below. ______________________________________________________________________________ Analytes to measure (in appropriate biological fluid): Not applicable Bioequivalence based on (95% CI): Clinical endpoint Additional comments regarding the BE study with clinical endpoint: 1. The Office of Generic Drugs (OGD) recommends conducting a BE study with a clinical endpoint in the treatment of open angle glaucoma and ocular hypertension comparing the test product to the reference listed drug (RLD), each applied as one drop in both eyes three times daily at approximately 8:00 a.m., 4:00 p.m., and 10:00 p.m. for 42 days (6 weeks). 2. Inclusion criteria (the sponsor may add additional criteria): a. Male or nonpregnant females aged at least 18 years with chronic open angle glaucoma or ocular hypertension in both eyes b. -

What Precautions Should We Use with Statins for Women of Childbearing
CLINICAL INQUIRIES What precautions should we use with statins for women of childbearing age? Chaitany Patel, MD, Lisa Edgerton, PharmD New Hanover Regional Medical Center, Wilmington, North Carolina Donna Flake, MSLS, MSAS Coastal Area Health Education Center, Wilmington, NC EVIDENCE- BASED ANSWER Statins are contraindicated for women who are on its low tissue-penetration properties. pregnant or breastfeeding. Data evaluating statin Cholesterol-lowering with simvastatin 40 mg/d did use for women of childbearing age is limited; how- not disrupt menstrual cycles or effect luteal phase ever, they may be used cautiously with adequate duration (strength of recommendation: C). contraception. Pravastatin may be preferred based CLINICAL COMMENTARY Use statins only as a last resort Before reading this review, I had not been for women of childbearing age ® Dowdenaware Health of the serious Media effects of statin medications I try to follow the USPSTF recommendations and on the developing fetus. In conversations with not screen women aged <45 years without coro- my colleagues, I found that the adverse effects nary artery disease riskCopyright factors for Fhyperlipidemia.or personalof usestatins onlyduring pregnancy are not readily When a woman of any age needs treatment, my known. Such information needs to be more first-line therapy is lifestyle modification. Given the widely disseminated. risks of statin drugs to the developing fetus, Ariel Smits, MD women with childbearing potential should give Department of Family Medicine, Oregon Health & Science fully informed consent and be offered reliable University, Portland contraception before stating statin therapy. I Evidence summary anal, cardiac, tracheal, esophageal, renal, Hydroxymethyl glutaryl coenzyme A and limb deficiency (VACTERL associa- (HMG CoA) reductase inhibitors, com- tion), intrauterine growth retardation monly called statins, have been on the (IUGR), and demise in fetuses exposed market since the late 1980s. -
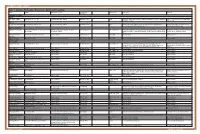
Table 1. Glaucoma Medications: Mechanisms, Dosing and Precautions Brand Generic Mechanism of Action Dosage/Avg
OPTOMETRIC STUDY CENTER Table 1. Glaucoma Medications: Mechanisms, Dosing and Precautions Brand Generic Mechanism of Action Dosage/Avg. % Product Sizes Side Effects Warnings Reduction CHOLINERGIC AGENTS Direct Pilocarpine (generic) Pilocarpine 1%, 2%, 4% Increases trabecular outflow BID-QID/15-25% 15ml Headache, blurred vision, myopia, retinal detachment, bronchiole constriction, Angle closure, shortness of breath, retinal narrowing of angle detachment Indirect Phospholine Iodide (Pfizer) Echothiophate iodide 0.125% Increases trabecular outflow QD-BID/15-25% 5ml Same as above plus cataractogenic iris cysts in children, pupillary block, Same as above, plus avoid prior to any increased paralysis with succinylcholine general anesthetic procedure ALPHA-2 AGONISTS Alphagan P (Allergan) Brimonidine tartrate 0.1%, 0.15% with Purite Decreases aqueous production, increases BID-TID/up to 26% 5ml, 10ml, 15ml Dry mouth, hypotension, bradycardia, follicular conjunctivitis, ocular irritation, Monitor for shortness of breath, dizziness, preservative uveoscleral outflow pruritus, dermatitis, conjunctival blanching, eyelid retraction, mydriasis, drug ocular redness and itching, fatigue allergy Brimonidine tartrate Brimonidine tartrate 0.15%, 0.2% Same as above Same as above 5ml, 10ml Same as above Same as above (generic) Iopidine (Novartis) Apraclonidine 0.5% Decreases aqueous production BID-TID/up to 25% 5ml, 10ml Same as above but higher drug allergy (40%) Same as above BETA-BLOCKERS Non-selective Betagan (Allergan) Levobunolol 0.25%, 0.5% Decreases -

Contraception and Misconceptions
CONTRACEPTION AND MISCONCEPTIONS CONTRACEPTION IN WOMEN WITH MENTAL ILLNESS OVERVIEW Hormones and mood How mental illness impacts on contraceptive choice Ideal contraception Pro and cons of contraceptive methods in women with mental illness Hormonal contraception and mood ESTROGENS anti-inflammatory neuroprotective effects of estradiol modulation of the limbic processing memory of emotionally-relevant information. estradiol “beneficially” modulates pathways implicated in the pathophysiology of depression, including serotonin and norepinephrine pathways PROGESTROGENS Previously thought to be anxiogenic, depressogenic Breakdown products Depression – alpha hydroxy progestrogen breakdown products pro – inflammatory, anxiogenic HORMONES AND MOODS – COMPLEX INTERPLAY MENTAL ILLNESS AND CONTRACEPTIVE CHOICE Effect of mental illness on contraceptive choice Effect of contraceptive choice on mental illness Drug interactions EFFECT MENTAL ILLNESS ON CONTRACEPTIVE CHOICE Impulsive Poor planning Cognitive and problem judgement Poor adherence IMPULSIVITY COGNITION POOR JUDGEMENT LETS NOT FORGET SUBSTANCES…… TYPES OF CONTRACEPTION No method Non hormonal Condom/Femidom Diaphragm Non hormone containing IUCD (Copper T) Hormonal COC POP Mirena Evra Patch Nuva Ring Implant ORAL CONTRACEPTIVES POP – avoid Same time every day COC Pros Effective Reduction PMS – monophasic estrogen dominant pill eg Femodene, Yaz, Nordette Cons Drug interactions Pill burden Daily dose EVRA PATCH Weekly patch Transdermal system: 150 mcg/day -

209627Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 209627Orig1s000 MULTI-DISCIPLINE REVIEW Summary Review Office Director Cross Discipline Team Leader Review Clinical Review Non-Clinical Review Statistical Review Clinical Pharmacology Review Reviewers of Multi-Disciplinary Review and Evaluation SECTIONS OFFICE/ AUTHORED/ ACKNOWLEDGED/ DISCIPLINE REVIEWER DIVISION APPROVED Mark Seggel, Ph.D. OPQ/ONDP/DNDP2 Authored: Section 4.2 Digitally signed by Mark R. Seggel -S CMC Lead DN: c=US, o=U.S. Government, ou=HHS, ou=FDA, ou=People, cn=Mark R. Signature: Mark R. Seggel -S Seggel -S, 0.9.2342.19200300.100.1.1=1300071539 Date: 2018.08.08 16:29:15 -04'00' Frederic Moulin, DVM, PhD OND/ODE3/DBRUP Authored: Section 5 Pharmacology/ Digitally signed by Frederic Moulin -S Toxicology DN: c=US, o=U.S. Government, ou=HHS, ou=FDA, ou=People, Reviewer Signature: Frederic Moulin -S 0.9.2342.19200300.100.1.1=2001708658, cn=Frederic Moulin -S Date: 2018.08.08 15:26:57 -04'00' Kimberly Hatfield, PhD OND/ODE3/DBRUP Approved: Section 5 Pharmacology/ Toxicology Digitally signed by Kimberly P. Hatfield -S DN: c=US, o=U.S. Government, ou=HHS, ou=FDA, ou=People, Team Leader Signature: Kimberly P. Hatfield -S 0.9.2342.19200300.100.1.1=1300387215, cn=Kimberly P. Hatfield -S Date: 2018.08.08 14:56:10 -04'00' Li Li, Ph.D. OCP/DCP3 Authored: Sections 6 and 17.3 Clinical Pharmacology Dig ta ly signed by Li Li S DN c=US o=U S Government ou=HHS ou=FDA ou=People Reviewer cn=Li Li S Signature: Li Li -S 0 9 2342 19200300 100 1 1=20005 08577 Date 2018 08 08 15 39 23 04'00' Doanh Tran, Ph.D. -

Estrogen and Progestin Hormone Doses in Combined Birth Control Pills
Estrogen and Progestin Hormone Doses in Combined Birth Control Pills Estrogen level Pill Brand Name Progestin Dose (mg) ethinyl estradiol (micrograms) 20 mcgm Alesse® levonorgestrel 0.10 Levlite® levonorgestrel 0.10 Loestrin 1/20® Fe norethindrone 1.00 acetate Mircette® desogestrel 0.15 Ortho Evra® norelgestromin 0.15 (patch) (norgestimate metabolite) phasic Estrostep® Fe norethindrone 1.0/1.0/1.0 20/30/35 mcgm acetate 30 mcgm Levlen® levonorgestrel 0.15 Levora® levonorgestrel 0.15 Nordette® levonorgestrel 0.15 Lo/Ovral® norgestrel 0.30 Desogen® desogestrel 0.15 Ortho-Cept® desogestrel 0.15 Loestrin® 1.5/30 norethindrone 1.50 acetate Yasmin® drospirenone 3.0 phasic Triphasil® levonorgestrel 0.05/0.075/0.125 30/40/30 mcgm Tri-Levlen® levonorgestrel 0.05/0.075/0.125 Trivora® levonorgestrel 0.05/0.075/0.125 35 mcgm Ortho-Cyclen® norgestimate 0.25 Ovcon-35® norethindrone 0.40 Brevicon® norethindrone 0.50 Modicon® norethindrone 0.50 Necon® norethindrone 1.00 Norethin® norethindrone 1.00 Norinyl® 1/35 norethindrone 1.00 Ortho-Novum® 1/35 norethindrone 1.00 Demulen® 1/35 ethynodiol diacetate 1.00 Zovia® 1/35E ethynodiol diacetate 1.00 phasic Ortho-Novum® norethindrone 0.50/1.00 35/35 mcgm 10/11 Jenest® norethindrone 0.50/1.00 phasic Ortho-Tri-Cyclen® norgestimate 0.15/0.215/0.25 35/35/35 mcgm Ortho-Novum® norethindrone 0.50/0.75/1.00 7/7/7 Tri-Norinyl® norethindrone 0.50/1.00/0.50 50 mcgm Necon® 1/50 norethindrone 1.00 Norinyl® 1/50 norethindrone 1.00 Ortho-Novum® 1/50 norethindrone 1.00 Ovcon-50® norethindrone 1.00 Ovral® norgestrel 0.50 Demulen® 1/50 ethynodiol diacetate 1.00 Zovia® 1/50E ethynodiol diacetate 1.00 Which pills have higher progestin side efects or cause more acne and hair growth? Each progestin has a diferent potency, milligram per milligram, in terms of progesterone efect to stop menstrual bleeding or androgen efect to stimulate acne and hair growth. -

NEW ZEALAND DATA SHEET 1. PRODUCT NAME IOPIDINE® (Apraclonidine Hydrochloride) Eye Drops 0.5%
NEW ZEALAND DATA SHEET 1. PRODUCT NAME IOPIDINE® (apraclonidine hydrochloride) Eye Drops 0.5%. 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each mL of Iopidine Eye Drops 0.5% contains apraclonidine hydrochloride 5.75 mg, equivalent to apraclonidine base 5 mg. Excipient with known effect Benzalkonium chloride 0.1 mg per 1 mL as a preservative. For the full list of excipients, see section 6.1. 2. PHARMACEUTICAL FORM Eye drops, solution, sterile, isotonic. 4. CLINICAL PARTICULARS 4.1. Therapeutic indications Iopidine Eye Drops 0.5% are indicated for short-term adjunctive therapy in patients on maximally tolerated medical therapy who require additional IOP reduction. Patients on maximally tolerated medical therapy who are treated with Iopidine Eye Drops 0.5% to delay surgery should have frequent follow up examinations and treatment should be discontinued if the intraocular pressure rises significantly. The addition of Iopidine Eye Drops 0.5% to patients already using two aqueous suppressing drugs (i.e. beta-blocker plus carbonic anhydrase inhibitor) as part of their maximally tolerated medical therapy may not provide additional benefit. This is because apraclonidine is an aqueous-suppressing drug and the addition of a third aqueous suppressant may not significantly reduce IOP. The IOP-lowering efficacy of Iopidine Eye Drops 0.5% diminishes over time in some patients. This loss of effect, or tachyphylaxis, appears to be an individual occurrence with a variable time of onset and should be closely monitored. The benefit for most patients is less than one month. 4.2. Dose and method of administration Dose One drop of Iopidine Eye Drops 0.5% should be instilled into the affected eye(s) three times per day. -

Pharmacogenomics of Endocrine Therapy in Breast Cancer
Journal of Human Genetics (2013) 58, 306–312 & 2013 The Japan Society of Human Genetics All rights reserved 1434-5161/13 OPEN www.nature.com/jhg REVIEW Pharmacogenomics of endocrine therapy in breast cancer James N Ingle The most important modality of treatment in the two-thirds of patients with an estrogen receptor (ER)-positive early breast cancer is endocrine therapy. In postmenopausal women, options include the selective ER modulators (SERMs), tamoxifen and raloxifene, and the ‘third-generation’ aromatase inhibitors (AIs), anastrozole, exemestane and letrozole. Under the auspices of the National Institutes of Health Global Alliance for Pharmacogenomics, Japan, the Mayo Clinic Pharmacogenomics Research Network Center and the RIKEN Center for Genomic Medicine have worked collaboratively to perform genome-wide association studies (GWAS) in women treated with both SERMs and AIs. On the basis of the results of the GWAS, scientists at the Mayo Clinic have proceeded with functional genomic laboratory studies. As will be seen in this review, this has led to new knowledge relating to endocrine biology that has provided a clear focus for further research to move toward truly personalized medicine for women with breast cancer. Journal of Human Genetics (2013) 58, 306–312; doi:10.1038/jhg.2013.35; published online 2 May 2013 Keywords: aromatase inhibitors; breast cancer; pharmacogenomics; tamoxifen INTRODUCTION trials were the double-blind, placebo-controlled NSABP P-1 trial of Breast cancer is the most common form of cancer in women both in tamoxifen8, and the double-blind NSABP P-2 trial that compared the United States1 and Japan.2 Endocrine therapy is the most raloxifene with tamoxifen.9,10 Combined, these two studies involved important modality in the two-thirds of patients with an estrogen over 33 000 women, which constituted about 59% of the world’s receptor (ER)-positive early breast cancer. -

Aromatase Inhibitors
FACTS FOR LIFE Aromatase Inhibitors What are aromatase inhibitors? Aromatase Inhibitors vs. Tamoxifen Aromatase inhibitors (AIs) are a type of hormone therapy used to treat some breast cancers. They AIs and tamoxifen are both hormone therapies, are taken in pill form and can be started after but they act in different ways: surgery or radiation therapy. They are only given • AIs lower the amount of estrogen in the body to postmenopausal women who have a hormone by stopping certain hormones from turning receptor-positive tumor, a tumor that needs estrogen into estrogen. If estrogen levels are low to grow. enough, the tumor cannot grow. AIs are used to stop certain hormones from turning • Tamoxifen blocks estrogen receptors on breast into estrogen. In doing so, these drugs lower the cancer cells. Estrogen is still present in normal amount of estrogen in the body. levels, but the breast cancer cells cannot get enough of it to grow. Generic/Brand names of AI’s As part of their treatment plan, some post- Generic name Brand name menopausal women will use AIs alone. Others anastrozole Arimidex will use tamoxifen for 1-5 years and then begin exemestane Aromasin using AIs. letrozole Femara Who can use aromatase inhibitors? Postmenopausal women with early stage and metastatic breast cancer are often treated with AIs. After menopause, the ovaries produce only a small amount of estrogen. AIs stop the body from making estrogen, and as a result hormone receptor-positive tumors do not get fed by estrogen and die. AIs are not given to premenopausal women because their ovaries still produce estrogen. -

Tetracaine and Oxymetazoline
PATIENT & CAREGIVER EDUCATION Tetracaine and Oxymetazoline This information from Lexicomp® explains what you need to know about this medication, including what it’s used for, how to take it, its side effects, and when to call your healthcare provider. What is this drug used for? It is used before dental care to numb the area. What do I need to tell the doctor BEFORE my child takes this drug? If your child is allergic to this drug; any part of this drug; or any other drugs, foods, or substances. Tell the doctor about the allergy and what signs your child had. If your child has thyroid disease, talk with the doctor. If your child has high blood pressure. If your child has methemoglobinemia. If your child is taking certain drugs used for depression like isocarboxazid, phenelzine, or tranylcypromine, or drugs used for certain other health problems like selegiline or rasagiline. If your child is taking or has recently taken any drugs for mental or mood problems like depression. There are many drugs that Tetracaine and Oxymetazoline 1/7 must not be taken with this drug. Talk with your child’s doctor if you are not sure. If your child is taking any of these drugs: Nadolol, penbutolol, pindolol, propranolol, sotalol, or timolol. If your child has used another drug in the last 24 hours that has the same drug in it. If your child is using another drug in the nose. If your child weighs less than 88 pounds (40 kilograms). This drug is not for use in children who weigh less than 88 pounds (40 kilograms).