Prof. Dr. / Khaled Elhayes C
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Glossary for Narrative Writing
Periodontal Assessment and Treatment Planning Gingival description Color: o pink o erythematous o cyanotic o racial pigmentation o metallic pigmentation o uniformity Contour: o recession o clefts o enlarged papillae o cratered papillae o blunted papillae o highly rolled o bulbous o knife-edged o scalloped o stippled Consistency: o firm o edematous o hyperplastic o fibrotic Band of gingiva: o amount o quality o location o treatability Bleeding tendency: o sulcus base, lining o gingival margins Suppuration Sinus tract formation Pocket depths Pseudopockets Frena Pain Other pathology Dental Description Defective restorations: o overhangs o open contacts o poor contours Fractured cusps 1 ww.links2success.biz [email protected] 914-303-6464 Caries Deposits: o Type . plaque . calculus . stain . matera alba o Location . supragingival . subgingival o Severity . mild . moderate . severe Wear facets Percussion sensitivity Tooth vitality Attrition, erosion, abrasion Occlusal plane level Occlusion findings Furcations Mobility Fremitus Radiographic findings Film dates Crown:root ratio Amount of bone loss o horizontal; vertical o localized; generalized Root length and shape Overhangs Bulbous crowns Fenestrations Dehiscences Tooth resorption Retained root tips Impacted teeth Root proximities Tilted teeth Radiolucencies/opacities Etiologic factors Local: o plaque o calculus o overhangs 2 ww.links2success.biz [email protected] 914-303-6464 o orthodontic apparatus o open margins o open contacts o improper -

WHAT HAPPENED? CDR, a 24-Year-Old Chinese Male
CHILDHOOD DEVELOPMENTAL SCREENING 2020 https://doi.org/10.33591/sfp.46.5.up1 FINDING A MASS WITHIN THE ORAL CAVITY: WHAT ARE THE COMMON CAUSES AND 4-7 GAINING INSIGHT: WHAT ARE THE ISSUES? In Figure 2 below, a list of masses that could arise from each site Figure 3. Most common oral masses What are the common salivary gland pathologies Salivary gland tumours (Figure 7) commonly present as channel referrals to appropriate specialists who are better HOW SHOULD A GP MANAGE THEM? of the oral cavity is given and elaborated briey. Among the that a GP should be aware of? painless growing masses which are usually benign. ey can equipped in centres to accurately diagnose and treat these Mr Tan Tai Joum, Dr Marie Stella P Cruz CDR had a slow-growing mass in the oral cavity over one year more common oral masses are: torus palatinus, torus occur in both major and minor salivary glands but are most patients, which usually involves surgical excision. but sought treatment only when he experienced a sudden acute mandibularis, pyogenic granuloma, mucocele, broma, ere are three pairs of major salivary glands (parotid, commonly found occurring in the parotid glands. e most 3) Salivary gland pathology may be primary or secondary to submandibular and sublingual) as well as hundreds of minor ABSTRACT onset of severe pain and numbness. He was fortunate to have leukoplakia and squamous cell carcinoma – photographs of common type of salivary gland tumour is the pleomorphic systemic causes. ese dierent diseases may present with not sought treatment as it had not caused any pain. -
Mandibular Tori
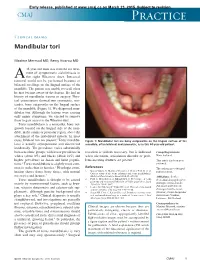
Early release, published at www.cmaj.ca on March 23, 2015. Subject to revision. CMAJ Practice Clinical images Mandibular tori Maxime Mermod MD, Remy Hoarau MD 44-year-old man was referred for treat- ment of symptomatic sialolithiasis in A the right Wharton duct. Intraoral removal could not be performed because of bilateral swellings on the lingual surface of the mandible. The patient was unable to recall when he first became aware of the lesions. He had no history of mandibular trauma or surgery. Phys- ical examination showed two symmetric, non- tender, bony outgrowths on the lingual surface of the mandible (Figure 1). We diagnosed man- dibular tori. Although the lesions were causing only minor symptoms, we elected to remove them to gain access to the Wharton duct. Torus mandibularis is a nontender, bony out- growth located on the lingual side of the man- dible, in the canine or premolar region, above the attachment of the mylohyoid muscle. In most 1 cases, bilateral tori are present. Torus mandibu- Figure 1: Mandibular tori are bony outgrowths on the lingual surface of the laris is usually asymptomatic and discovered mandible, often bilateral and symmetric, as in this 44-year-old patient. incidentally. The prevalence varies substantially between ethnic groups, with lower prevalence in resection is seldom necessary, but is indicated Competing interests: whites (about 8%) and blacks (about 16%) and when ulceration, articulation disorder or prob- None declared. higher prevalence in Asian and Inuit popula- lems inserting dentures are present.3 This article has been peer tions.2 Torus mandibularis is slightly more com- reviewed. -

Abscesses Apicectomy
BChD, Dip Odont. (Mondchir.) MBChB, MChD (Chir. Max.-Fac.-Med.) Univ. of Pretoria Co Reg: 2012/043819/21 Practice.no: 062 000 012 3323 ABSCESSES WHAT IS A TOOTH ABSCESS? A dental/tooth abscess is a localised acute infection at the base of a tooth, which requires immediate attention from your dentist. They are usually associated with acute pain, swelling and sometimes an unpleasant smell or taste in the mouth. More severe infections cause facial swelling as the bacteria spread to the nearby tissues of the face. This is a very serious condition. Once the swelling begins, it can spread rapidly. The pain is often made worse by drinking hot or cold fluids or biting on hard foods and may spread from the tooth to the ear or jaw on the same side. WHAT CAUSES AN ABSCESS? Damage to the tooth, an untreated cavity, or a gum disease can cause an abscessed tooth. If the cavity isn’t treated, the inside of the tooth can become infected. The bacteria can spread from the tooth to the tissue around and beneath it, creating an abscess. Gum disease causes the gums to pull away from the teeth, leaving pockets. If food builds up in one of these pockets, bacteria can grow, and an abscess may form. An abscess can cause the bone around the tooth to dissolve. WHY CAN'T ANTIBIOTIC TREATMENT ALONE BE USED? Antibiotics will usually help the pain and swelling associated with acute dental infections. However, they are not very good at reaching into abscesses and killing all the bacteria that are present. -

Oral Pathology Final Exam Review Table Tuanh Le & Enoch Ng, DDS
Oral Pathology Final Exam Review Table TuAnh Le & Enoch Ng, DDS 2014 Bump under tongue: cementoblastoma (50% 1st molar) Ranula (remove lesion and feeding gland) dermoid cyst (neoplasm from 3 germ layers) (surgical removal) cystic teratoma, cyst of blandin nuhn (surgical removal down to muscle, recurrence likely) Multilocular radiolucency: mucoepidermoid carcinoma cherubism ameloblastoma Bump anterior of palate: KOT minor salivary gland tumor odontogenic myxoma nasopalatine duct cyst (surgical removal, rare recurrence) torus palatinus Mixed radiolucencies: 4 P’s (excise for biopsy; curette vigorously!) calcifying odontogenic (Gorlin) cyst o Pyogenic granuloma (vascular; granulation tissue) periapical cemento-osseous dysplasia (nothing) o Peripheral giant cell granuloma (purple-blue lesions) florid cemento-osseous dysplasia (nothing) o Peripheral ossifying fibroma (bone, cartilage/ ossifying material) focal cemento-osseous dysplasia (biopsy then do nothing) o Peripheral fibroma (fibrous ct) Kertocystic Odontogenic Tumor (KOT): unique histology of cyst lining! (see histo notes below); 3 important things: (1) high Multiple bumps on skin: recurrence rate (2) highly aggressive (3) related to Gorlin syndrome Nevoid basal cell carcinoma (Gorlin syndrome) Hyperparathyroidism: excess PTH found via lab test Neurofibromatosis (see notes below) (refer to derm MD, tell family members) mucoepidermoid carcinoma (mixture of mucus-producing and squamous epidermoid cells; most common minor salivary Nevus gland tumor) (get it out!) -

Oral Health and Disease
Downloaded from bmj.com on 19 August 2005 ABC of oral health: Oral health and disease Ruth Holt, Graham Roberts and Crispian Scully BMJ 2000;320;1652-1655 doi:10.1136/bmj.320.7250.1652 Updated information and services can be found at: http://bmj.com/cgi/content/full/320/7250/1652 These include: Rapid responses One rapid response has been posted to this article, which you can access for free at: http://bmj.com/cgi/content/full/320/7250/1652#responses You can respond to this article at: http://bmj.com/cgi/eletter-submit/320/7250/1652 Email alerting Receive free email alerts when new articles cite this article - sign up in the box at service the top right corner of the article Topic collections Articles on similar topics can be found in the following collections Dentistry and Oral Medicine (79 articles) Notes To order reprints of this article go to: http://www.bmjjournals.com/cgi/reprintform To subscribe to BMJ go to: http://bmj.bmjjournals.com/subscriptions/subscribe.shtml Clinical review Downloaded from bmj.com on 19 August 2005 ABC of oral health Oral health and disease Ruth Holt, Graham Roberts, Crispian Scully A healthy dentition and mouth is important to both quality of life and nutrition, and oral disease may affect systemic health, as Enamel covering crown Gingival crevice discussed in later articles in this series. (gingival sulcus) Dentine Development of the dentition Gingiva Pulp chamber Teeth form mainly from neuroectoderm and comprise a crown of insensitive enamel surrounding sensitive dentine and a root Periodontal ligament that has no enamel covering. -

QUICK ORAL HEALTH FACTS ABOUT the YOUNG Dr Ng Jing Jing, Dr Wong Mun Loke
ORAL health IN PRIMARY CARE UNIT NO. 2 QUICK ORAL HEALTH FACTS ABOUT THE YOUNG Dr Ng Jing Jing, Dr Wong Mun Loke ABSTRACT Table 1. Eruption sequence of Primary Dentition This article sheds light on the sequence of teeth eruption Primary Upper Teeth Primary Lower Teeth in the young and teething problems; highlights the importance and functions of the primary dentition and Central Incisors: 8-13 months Central Incisors: 6-10 months provides a quick overview of common developmental Lateral Incisors: 8-13 months Lateral Incisors: 10-16 months dental anomalies and other dental conditions in Canines: 16-23 months Canines: 16-23 months children. First Molars: 16-23 months First Molars: 13-19 months Second Molars: 25-33 months Second Molars: 23-31 months SFP2011; 37(1) Supplement : 10-13 Table 2. Eruption sequence of Adult Dentition Adult Upper Teeth Adult Lower Teeth INTRODUCTION Central Incisors: 7-8 years Central Incisors: 6-7 years The early years are always full of exciting moments as we observe Lateral Incisors: 8-9 years Lateral Incisors: 7-8 years our children grow and develop. One of the most noticeable Canines: 11-12 years Canines: 9-10 years aspects of their growth and development is the eruption of First Premolars: 10-11 years First Premolars: 10-11 years teeth. The first sign of a tooth in the mouth never fails to Second Premolars: 11-12 years Second Premolars: 11-12 years attract the attention of the parent and child. For the parent, it First Molars: 6-7 years First Molars: 6-7 years marks an important developmental milestone of the child but Second Molars: 12-13 years Second Molars: 11-13 years for the child, it can be a source of irritation brought on by the Third Molars: 18-25 years Third Molars: 18-25 years whole process of teething. -

Concurrence of Torus Palatinus, Torus Mandibularis and Buccal Exostosis Sarfaraz Khan1, Syed Asif Haider Shah2, Farman Ali3 and Dil Rasheed4
CASE REPORT Concurrence of Torus Palatinus, Torus Mandibularis and Buccal Exostosis Sarfaraz Khan1, Syed Asif Haider Shah2, Farman Ali3 and Dil Rasheed4 ABSTRACT Torus palatinus (TP), torus mandibularis (TM), and buccal exostosis are localised, benign, osseous projections, occurring in maxilla and mandible. Etiology is multifactorial and not well established. Tori and exostoses have been associated with parafunctional occlusal habits, temporomandibular joint (TMJ) disorders, migraine and consumption of fish. Concurrence of TP, TM, and exostosis in the same individual is very rare. Concurrence of TP and TM has not been reported from Pakistan. We report a case of a 22-year female patient manifesting concurrence of TP, bilateral TM, and maxillary buccal exostoses; with possible association of abnormal occlusal stresses and use of calcium and vitamin D supplements. Key Words: Torus palatinus. Torus mandibularis. Exostoses. INTRODUCTION upper teeth, for the last one year. She noticed a gradual Torus palatinus (TP) is a localised, benign, osseous increase in the severity of her symptoms. The patient projection in midline of the hard palate. Torus denied any associated pain or ulceration. She had mandibularis (TM) is a benign, bony protuberance, on remained under orthodontic treatment for 2 years for the lingual aspect of the mandible, usually bilaterally, at correction of her crooked teeth. After completion of the the canine-premolar area, above the mylohyoid line. treatment, she was advised to wear removable retainer appliance; but owing to her admittedly non-compliant Exostoses are multiple small bony nodules occurring attitude towards treatment, malalignment of her teeth along the buccal or palatal aspects of maxilla and buccal recurred within the next 2 years. -

Adverse Effects of Medicinal and Non-Medicinal Substances
Benign? Not So Fast: Challenging Oral Diseases presented with DDX June 21st 2018 Dolphine Oda [email protected] Tel (206) 616-4748 COURSE OUTLINE: Five Topics: 1. Oral squamous cell carcinoma (SCC)-Variability in Etiology 2. Oral Ulcers: Spectrum of Diseases 3. Oral Swellings: Single & Multiple 4. Radiolucent Jaw Lesions: From Benign to Metastatic 5. Radiopaque Jaw Lesions: Benign & Other Oral SCC: Tobacco-Associated White lesions 1. Frictional white patches a. Tongue chewing b. Others 2. Contact white patches 3. Smoker’s white patches a. Smokeless tobacco b. Cigarette smoking 4. Idiopathic white patches Red, Speckled lesions 5. Erythroplakia 6. Georgraphic tongue 7. Median rhomboid glossitis Deep Single ulcers 8. Traumatic ulcer -TUGSE 9. Infectious Disease 10. Necrotizing sialometaplasia Oral Squamous Cell Carcinoma: Tobacco-associated If you suspect that a lesion is malignant, refer to an oral surgeon for a biopsy. It is the most common type of oral SCC, which accounts for over 75% of all malignant neoplasms of the oral cavity. Clinically, it is more common in men over 55 years of age, heavy smokers and heavy drinkers, more in males especially black males. However, it has been described in young white males, under the age of fifty non-smokers and non-drinkers. The latter group constitutes less than 5% of the patients and their SCCs tend to be in the posterior mouth (oropharynx and tosillar area) associated with HPV infection especially HPV type 16. The most common sites for the tobacco-associated are the lateral and ventral tongue, followed by the floor of mouth and soft palate area. -

Description Concept ID Synonyms Definition
Description Concept ID Synonyms Definition Category ABNORMALITIES OF TEETH 426390 Subcategory Cementum Defect 399115 Cementum aplasia 346218 Absence or paucity of cellular cementum (seen in hypophosphatasia) Cementum hypoplasia 180000 Hypocementosis Disturbance in structure of cementum, often seen in Juvenile periodontitis Florid cemento-osseous dysplasia 958771 Familial multiple cementoma; Florid osseous dysplasia Diffuse, multifocal cementosseous dysplasia Hypercementosis (Cementation 901056 Cementation hyperplasia; Cementosis; Cementum An idiopathic, non-neoplastic condition characterized by the excessive hyperplasia) hyperplasia buildup of normal cementum (calcified tissue) on the roots of one or more teeth Hypophosphatasia 976620 Hypophosphatasia mild; Phosphoethanol-aminuria Cementum defect; Autosomal recessive hereditary disease characterized by deficiency of alkaline phosphatase Odontohypophosphatasia 976622 Hypophosphatasia in which dental findings are the predominant manifestations of the disease Pulp sclerosis 179199 Dentin sclerosis Dentinal reaction to aging OR mild irritation Subcategory Dentin Defect 515523 Dentinogenesis imperfecta (Shell Teeth) 856459 Dentin, Hereditary Opalescent; Shell Teeth Dentin Defect; Autosomal dominant genetic disorder of tooth development Dentinogenesis Imperfecta - Shield I 977473 Dentin, Hereditary Opalescent; Shell Teeth Dentin Defect; Autosomal dominant genetic disorder of tooth development Dentinogenesis Imperfecta - Shield II 976722 Dentin, Hereditary Opalescent; Shell Teeth Dentin Defect; -

Partnering General Practitioners to Advance Community Oral Health
E D I T O R I A L PartNERING GENERAL PRACTITIONERS to ADVANCE CoMMUNITY ORAL Health SFP2011; 37(1) Supplement : 4 In Unit 3 – “Recognising Common Adult Oral Conditions” – Dr Rahul Nair, Dr Adeline Wong, Dr Joanna Ngo and Dr Wong Mun Loke highlight the common oral problems in the Oral health has long been overlooked in the medical adult population which are dental caries, and periodontal community. We are not well versed in anything more disease. The prevention of oral diseases has now taken on than the rudimentary aspects of oral health. The medical the strategy of targeting a small set of risk factors that are school curriculum is also lacking in coverage of this area of important for a large number of diseases. This Common Risk medicine. This is despite the fact that oral health and hygiene Factor Approach aims to reduce risk factors in diet, stress, is often one of the first indicators of the general health of hygiene, smoking, alcohol, lack of exercise and injuries to the individual, and of disease. prevent the onset of a range of diseases including dental caries and periodontal disease. Many of us in Family Practice see the very young in our daily work. Neonates, infants and toddlers make up, for some of In Unit 4 – “Ageing and its Influence on the Oral us, a large part of our clinical responsibilities. We are often Environment” – Dr Hilary Thean and Dr Wong Mun Loke faced with questions from anxious parents such as teething cover issues which are specific to the ageing process and issues, new tooth eruption, tongue tie and the list goes on. -

Orthognathic (Jaw) Surgery
UnitedHealthcare® Commercial Coverage Determination Guideline Orthognathic (Jaw) Surgery Guideline Number: CDG.013.14 Effective Date: July 1, 2021 Instructions for Use Table of Contents Page Related Commercial Policies Coverage Rationale ....................................................................... 1 • Obstructive Sleep Apnea Treatment Documentation Requirements ...................................................... 2 • Temporomandibular Joint Disorders Definitions ...................................................................................... 2 Applicable Codes .......................................................................... 3 Community Plan Policy References ..................................................................................... 6 • Orthognathic (Jaw) Surgery Guideline History/Revision Information ....................................... 6 Instructions for Use ....................................................................... 6 Coverage Rationale Orthognathic (jaw) surgery is a standard exclusion from coverage in most fully-insured plans. The following represents exceptions to the orthognathic (jaw) surgery exclusion and may be eligible for coverage as reconstructive and medically necessary: Acute traumatic injury Cancerous or non-cancerous tumors and cysts Obstructive sleep apnea Congenital anomalies Criteria Orthognathic (jaw) surgery may be eligible for coverage as reconstructive and medically necessary for the conditions cited above when the following criteria below are met: The presence