Abscesses Apicectomy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Lumps and Swellings
Clinical Oral medicine for the general practitioner: lumps and swellings Crispian Scully 1 his series of five papers summarises some of the most important oral medicine problems likely to be Tencountered by practitioners. Some are common, others rare. The practitioner cannot be expected to diagnose all, but has been trained to recognise oral health and disease, and should be competent to recognise normal variants, and common orofacial disorders. In any case of doubt, the practitioner is advised to seek a second opinion from a colleague. The series is not intended to be comprehensive in coverage either of the conditions encountered, or all aspects of Figure 1: Torus mandibularis. diagnosis or treatment: further details are available in standard texts, in the further reading section, or from the internet. The present article discusses aspects of lumps through fear, perhaps after hearing of someone with and swellings. ‘mouth cancer’. Thus some individuals discover and worry about normal anatomical features such as tori, the parotid Lumps and swellings papilla, foliate papillae on the tongue, or the pterygoid Lumps and swellings in the mouth are common, but of hamulus. The tongue often detects even a very small diverse aetiologies (Table 1), and some represent swelling, or the patient may first notice it because it is sore malignant neoplasms. Therefore, this article will discuss (Figure 1). In contrast, many oral cancers are diagnosed far lumps and swellings in general terms, but later focus on too late, often after being present several months, usually the particular problems of oral cancer and of orofacial because the patient ignores the swelling. -

Glossary for Narrative Writing
Periodontal Assessment and Treatment Planning Gingival description Color: o pink o erythematous o cyanotic o racial pigmentation o metallic pigmentation o uniformity Contour: o recession o clefts o enlarged papillae o cratered papillae o blunted papillae o highly rolled o bulbous o knife-edged o scalloped o stippled Consistency: o firm o edematous o hyperplastic o fibrotic Band of gingiva: o amount o quality o location o treatability Bleeding tendency: o sulcus base, lining o gingival margins Suppuration Sinus tract formation Pocket depths Pseudopockets Frena Pain Other pathology Dental Description Defective restorations: o overhangs o open contacts o poor contours Fractured cusps 1 ww.links2success.biz [email protected] 914-303-6464 Caries Deposits: o Type . plaque . calculus . stain . matera alba o Location . supragingival . subgingival o Severity . mild . moderate . severe Wear facets Percussion sensitivity Tooth vitality Attrition, erosion, abrasion Occlusal plane level Occlusion findings Furcations Mobility Fremitus Radiographic findings Film dates Crown:root ratio Amount of bone loss o horizontal; vertical o localized; generalized Root length and shape Overhangs Bulbous crowns Fenestrations Dehiscences Tooth resorption Retained root tips Impacted teeth Root proximities Tilted teeth Radiolucencies/opacities Etiologic factors Local: o plaque o calculus o overhangs 2 ww.links2success.biz [email protected] 914-303-6464 o orthodontic apparatus o open margins o open contacts o improper -

WHAT HAPPENED? CDR, a 24-Year-Old Chinese Male
CHILDHOOD DEVELOPMENTAL SCREENING 2020 https://doi.org/10.33591/sfp.46.5.up1 FINDING A MASS WITHIN THE ORAL CAVITY: WHAT ARE THE COMMON CAUSES AND 4-7 GAINING INSIGHT: WHAT ARE THE ISSUES? In Figure 2 below, a list of masses that could arise from each site Figure 3. Most common oral masses What are the common salivary gland pathologies Salivary gland tumours (Figure 7) commonly present as channel referrals to appropriate specialists who are better HOW SHOULD A GP MANAGE THEM? of the oral cavity is given and elaborated briey. Among the that a GP should be aware of? painless growing masses which are usually benign. ey can equipped in centres to accurately diagnose and treat these Mr Tan Tai Joum, Dr Marie Stella P Cruz CDR had a slow-growing mass in the oral cavity over one year more common oral masses are: torus palatinus, torus occur in both major and minor salivary glands but are most patients, which usually involves surgical excision. but sought treatment only when he experienced a sudden acute mandibularis, pyogenic granuloma, mucocele, broma, ere are three pairs of major salivary glands (parotid, commonly found occurring in the parotid glands. e most 3) Salivary gland pathology may be primary or secondary to submandibular and sublingual) as well as hundreds of minor ABSTRACT onset of severe pain and numbness. He was fortunate to have leukoplakia and squamous cell carcinoma – photographs of common type of salivary gland tumour is the pleomorphic systemic causes. ese dierent diseases may present with not sought treatment as it had not caused any pain. -

Salivary Gland Infections and Salivary Stones (Sialadentis and Sialithiasis)
Salivary Gland Infections and Salivary Stones (Sialadentis and Sialithiasis) What is Sialadenitis and Sialithiasis? Sialdenitis is an infection of the salivary glands that causes painful swelling of the glands that produce saliva, or spit. Bacterial infections, diabetes, tumors or stones in the salivary glands, and tooth problems (poor oral hygiene) may cause a salivary gland infection. The symptoms include pain, swelling, pus in the mouth, neck skin infection. These infections and affect the submandibular gland (below the jaw) or the parotid glands (in front of the ears). The symptoms can be minor and just be a small swelling after meals (symptoms tend to be worse after times of high saliva flow). Rarely, the swelling in the mouth will progress and can cut off your airway and cause you to stop breathing. What Causes Sialadenitis and Sialithiasis When the flow of saliva is blocked by a small stone (salilithiasis) in a salivary gland or when a person is dehydrated, bacteria can build up and cause an infection. A viral infection, such as the mumps, also can cause a salivary gland to get infected and swell. These infections can also be caused by a spread from rotten or decaying teeth. Sometimes there can be a buildup of calcium in the saliva ducts that form into stones. These can easily stop the flow of saliva and cause problems How are these infections and stones treated? Treatment depends on what caused your salivary gland infection. If the infection is caused by bacteria, your doctor may prescribe antibiotics. Home treatment such as drinking fluids, applying warm compresses, and sucking on lemon wedges or sour candy to increase saliva may help to clear the infection quicker. -
Mandibular Tori
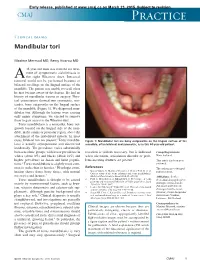
Early release, published at www.cmaj.ca on March 23, 2015. Subject to revision. CMAJ Practice Clinical images Mandibular tori Maxime Mermod MD, Remy Hoarau MD 44-year-old man was referred for treat- ment of symptomatic sialolithiasis in A the right Wharton duct. Intraoral removal could not be performed because of bilateral swellings on the lingual surface of the mandible. The patient was unable to recall when he first became aware of the lesions. He had no history of mandibular trauma or surgery. Phys- ical examination showed two symmetric, non- tender, bony outgrowths on the lingual surface of the mandible (Figure 1). We diagnosed man- dibular tori. Although the lesions were causing only minor symptoms, we elected to remove them to gain access to the Wharton duct. Torus mandibularis is a nontender, bony out- growth located on the lingual side of the man- dible, in the canine or premolar region, above the attachment of the mylohyoid muscle. In most 1 cases, bilateral tori are present. Torus mandibu- Figure 1: Mandibular tori are bony outgrowths on the lingual surface of the laris is usually asymptomatic and discovered mandible, often bilateral and symmetric, as in this 44-year-old patient. incidentally. The prevalence varies substantially between ethnic groups, with lower prevalence in resection is seldom necessary, but is indicated Competing interests: whites (about 8%) and blacks (about 16%) and when ulceration, articulation disorder or prob- None declared. higher prevalence in Asian and Inuit popula- lems inserting dentures are present.3 This article has been peer tions.2 Torus mandibularis is slightly more com- reviewed. -

Head and Neck
DEFINITION OF ANATOMIC SITES WITHIN THE HEAD AND NECK adapted from the Summary Staging Guide 1977 published by the SEER Program, and the AJCC Cancer Staging Manual Fifth Edition published by the American Joint Committee on Cancer Staging. Note: Not all sites in the lip, oral cavity, pharynx and salivary glands are listed below. All sites to which a Summary Stage scheme applies are listed at the begining of the scheme. ORAL CAVITY AND ORAL PHARYNX (in ICD-O-3 sequence) The oral cavity extends from the skin-vermilion junction of the lips to the junction of the hard and soft palate above and to the line of circumvallate papillae below. The oral pharynx (oropharynx) is that portion of the continuity of the pharynx extending from the plane of the inferior surface of the soft palate to the plane of the superior surface of the hyoid bone (or floor of the vallecula) and includes the base of tongue, inferior surface of the soft palate and the uvula, the anterior and posterior tonsillar pillars, the glossotonsillar sulci, the pharyngeal tonsils, and the lateral and posterior walls. The oral cavity and oral pharynx are divided into the following specific areas: LIPS (C00._; vermilion surface, mucosal lip, labial mucosa) upper and lower, form the upper and lower anterior wall of the oral cavity. They consist of an exposed surface of modified epider- mis beginning at the junction of the vermilion border with the skin and including only the vermilion surface or that portion of the lip that comes into contact with the opposing lip. -

Recognition and Management of Oral Health Problems in Older Adults by Physicians: a Pilot Study
J Am Board Fam Pract: first published as 10.3122/jabfm.11.6.474 on 1 November 1998. Downloaded from BRIEF REPORTS Recognition and Management of Oral Health Problems in Older Adults by Physicians: A Pilot Study Thomas V. Jones, MD, MPH, Mitchel J Siegel, DDS, andJohn R. Schneider, A1A Oral health problems are among the most com of the nation's current and future health care mon chronic health conditions experienced by needs, the steady increase in the older adult popu older adults. Healthy People 2000, an initiative to lation, and the generally high access elderly per improve the health of America, has selected oral sons have to medical care provided by family health as a priority area. l About 11 of 100,000 physicians and internists.s,7,8 Currently there is persons have oral cancer diagnosed every year.2 very little information about the ability of family The average age at which oral cancer is diagnosed physicians or internists, such as geriatricians, to is approximately 65 years, with the incidence in assess the oral health of older patients. We con creasing from middle adulthood through the sev ducted this preliminary study to determine how enth decade of life. l-3 Even though the mortality family physicians and geriatricians compare with rate associated with oral cancer (7700 deaths an each other and with general practice dentists in nually)4 ranks among the lowest compared with their ability to recognize, diagnose, and perform other cancers, many deaths from oral cancer initial management of a wide spectrum of oral might be prevented by improved case finding and health problems seen in older adults. -

Basic Histology (23 Questions): Oral Histology (16 Questions
Board Question Breakdown (Anatomic Sciences section) The Anatomic Sciences portion of part I of the Dental Board exams consists of 100 test items. They are broken up into the following distribution: Gross Anatomy (50 questions): Head - 28 questions broken down in this fashion: - Oral cavity - 6 questions - Extraoral structures - 12 questions - Osteology - 6 questions - TMJ and muscles of mastication - 4 questions Neck - 5 questions Upper Limb - 3 questions Thoracic cavity - 5 questions Abdominopelvic cavity - 2 questions Neuroanatomy (CNS, ANS +) - 7 questions Basic Histology (23 questions): Ultrastructure (cell organelles) - 4 questions Basic tissues - 4 questions Bone, cartilage & joints - 3 questions Lymphatic & circulatory systems - 3 questions Endocrine system - 2 questions Respiratory system - 1 question Gastrointestinal system - 3 questions Genitouirinary systems - (reproductive & urinary) 2 questions Integument - 1 question Oral Histology (16 questions): Tooth & supporting structures - 9 questions Soft oral tissues (including dentin) - 5 questions Temporomandibular joint - 2 questions Developmental Biology (11 questions): Osteogenesis (bone formation) - 2 questions Tooth development, eruption & movement - 4 questions General embryology - 2 questions 2 National Board Part 1: Review questions for histology/oral histology (Answers follow at the end) 1. Normally most of the circulating white blood cells are a. basophilic leukocytes b. monocytes c. lymphocytes d. eosinophilic leukocytes e. neutrophilic leukocytes 2. Blood platelets are products of a. osteoclasts b. basophils c. red blood cells d. plasma cells e. megakaryocytes 3. Bacteria are frequently ingested by a. neutrophilic leukocytes b. basophilic leukocytes c. mast cells d. small lymphocytes e. fibrocytes 4. It is believed that worn out red cells are normally destroyed in the spleen by a. neutrophils b. -

SUBMANDIBULAR GLAND REMOVAL Post Operative Instructions
SUBMANDIBULAR GLAND REMOVAL Post Operative Instructions Nurse Line (8:30am to 5pm) 937-496-0261 Emergency After Hours Line 937-496-2600 The Surgery Itself Surgery to remove the submandibular gland involves general anesthesia, typically for about two hours. Patients may be quite sedated for several hours after surgery and may remain sleepy for much of the day. Nausea and vomiting are occasionally seen, and usually resolve by the evening of surgery - even without additional medications. Some patients stay overnight in the hospital; other patients can go home the evening of surgery. Some patients will have a drain in place after surgery; this is removed the following day before you go home from the hospital or in the office 1-2 days after surgery. Your Incision Your incision is closed with absorbable sutures and is covered with a small strip of tape or skin glue. You can shower and wash your hair as usual starting 24 hours after your drain is removed. If you did not have a drain in place after surgery, you may shower 24 hours after surgery. You may wash in a bathtub prior to that time if you are careful not to get your neck wet. Use a dab of Bacitracin ointment on your drain site (on one side of your incision, not covered by the tape or glue) before and after showering. Do not soak or scrub the incision. You might notice bruising around your incision or jaw line and slight swelling above the scar when you are upright. In addition, the scar may become pink and hard. -

Submandibular Gland Transfer for Prevention of Xerostomia After Radiation Therapy Swallowing Outcomes
ORIGINAL ARTICLE Submandibular Gland Transfer for Prevention of Xerostomia After Radiation Therapy Swallowing Outcomes Jana Rieger, PhD; Hadi Seikaly, MD; Naresh Jha, MBBS; Jeffrey Harris, MD; David Williams, MD; Richard Liu, MD; Tim McGaw, DDS; John Wolfaardt, PhD Objective: To assess swallowing outcomes in patients had preservation of 1 submandibular gland (SJP group) with oropharyngeal carcinoma in relation to the Seikaly- and 11 who did not (control group). Jha procedure for submandibular gland transfer (SJP). The SJP has recently been described as beneficial in the Main Outcome Measures: Quantitative and qualita- prevention of xerostomia induced by radiation therapy tive aspects of swallowing were obtained to determine in patients with head and neck cancer. whether patients in the SJP group performed more op- timally than those in the control group. Design: Inception cohort. Results: Baseline and stimulated salivary flow rates were Setting: University-affiliated primary care center. significantly different between groups. Patients in the SJP group were able to move the bolus through the oral cavity Patients: A phase 2 clinical trial was conducted from and into the pharynx faster than those in the control group. February 1, 1999, through February 28, 2002, to evalu- In addition, patients in the SJP group swallowed less often ate SJP in patients with head and neck cancer. During per bolus than patients in the control group. The com- that period, a consecutive sample of 51 patients who un- plete swallowing sequence was twice as long in controls. derwent surgical resection and reconstruction with a ra- dial forearm free flap for oropharyngeal carcinoma were Conclusions: The SJP for submandibular gland trans- referred for functional assessment of swallowing after fer appears to be beneficial in promoting more time- completion of adjuvant radiation therapy. -

A Guide to Salivary Gland Disorders the Salivary Glands May Be Affected by a Wide Range of Neoplastic and Inflammatory
MedicineToday PEER REVIEWED ARTICLE CPD 1 POINT A guide to salivary gland disorders The salivary glands may be affected by a wide range of neoplastic and inflammatory disorders. This article reviews the common salivary gland disorders encountered in general practice. RON BOVA The salivary glands include the parotid glands, examination are often adequate to recognise and MB BS, MS, FRACS submandibular glands and sublingual glands differentiate many of these conditions. A wide (Figure 1). There are also hundreds of minor sali- array of benign and malignant neoplasms may also Dr Bova is an ENT, Head and vary glands located in the mucosa of the hard and affect the salivary glands and a neoplasia should Neck Surgeon, St Vincent’s soft palate, oral cavity, lips, tongue and oro - always be considered when assessing a salivary Hospital, Sydney, NSW. pharynx. The parotid gland lies in the preauricular gland mass. region and extends inferiorly over the angle of the mandible. The parotid duct courses anteriorly Inflammatory disorders from the parotid gland and enters the mouth Acute sialadenitis through the buccal mucosa adjacent to the second Acute inflammation of the salivary glands is usu- upper molar tooth. The submandibular gland lies ally of viral or bacterial origin. Mumps is the most in the submandibular triangle and its duct passes common causative viral illness, typically affecting anteriorly along the floor of the mouth to enter the parotid glands bilaterally. Children are most adjacent to the frenulum of the tongue. The sub- often affected, with peak incidence occurring at lingual glands are small glands that lie just beneath approximately 4 to 6 years of age. -

Oral Pathology Final Exam Review Table Tuanh Le & Enoch Ng, DDS
Oral Pathology Final Exam Review Table TuAnh Le & Enoch Ng, DDS 2014 Bump under tongue: cementoblastoma (50% 1st molar) Ranula (remove lesion and feeding gland) dermoid cyst (neoplasm from 3 germ layers) (surgical removal) cystic teratoma, cyst of blandin nuhn (surgical removal down to muscle, recurrence likely) Multilocular radiolucency: mucoepidermoid carcinoma cherubism ameloblastoma Bump anterior of palate: KOT minor salivary gland tumor odontogenic myxoma nasopalatine duct cyst (surgical removal, rare recurrence) torus palatinus Mixed radiolucencies: 4 P’s (excise for biopsy; curette vigorously!) calcifying odontogenic (Gorlin) cyst o Pyogenic granuloma (vascular; granulation tissue) periapical cemento-osseous dysplasia (nothing) o Peripheral giant cell granuloma (purple-blue lesions) florid cemento-osseous dysplasia (nothing) o Peripheral ossifying fibroma (bone, cartilage/ ossifying material) focal cemento-osseous dysplasia (biopsy then do nothing) o Peripheral fibroma (fibrous ct) Kertocystic Odontogenic Tumor (KOT): unique histology of cyst lining! (see histo notes below); 3 important things: (1) high Multiple bumps on skin: recurrence rate (2) highly aggressive (3) related to Gorlin syndrome Nevoid basal cell carcinoma (Gorlin syndrome) Hyperparathyroidism: excess PTH found via lab test Neurofibromatosis (see notes below) (refer to derm MD, tell family members) mucoepidermoid carcinoma (mixture of mucus-producing and squamous epidermoid cells; most common minor salivary Nevus gland tumor) (get it out!)