Head and Neck Contouring
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Parotid and Mandibular Salivary Glands Segmentation of the One Humped Dromedary Camel (Camelus Dromedarius)
Int. J. Adv. Res. Biol. Sci. (2017). 4(11): 32-41 International Journal of Advanced Research in Biological Sciences ISSN: 2348-8069 www.ijarbs.com DOI: 10.22192/ijarbs Coden: IJARQG(USA) Volume 4, Issue 11 - 2017 Research Article DOI: http://dx.doi.org/10.22192/ijarbs.2017.04.11.005 Parotid and Mandibular Salivary Glands Segmentation Of The One Humped Dromedary Camel (Camelus dromedarius) Hamdy M. Rezk and Nora A. Shaker* Department of Anatomy and Embryology, Faculty of Veterinary Medicine, Cairo University, Egypt *Corresponding author: [email protected] Abstract The present study provides detailed anatomical description of the parotid and mandibular salivary glands of the one humped camel with their segmentation based on arterial blood supply and salivary ducts; to facilitate partial removal of the pathologic gland. The shape, position, relations and blood supply of both salivary glands with their ducts were studied on six cadaveric heads. The mandibular and parotid ducts were injected with Urographin® as contrast medium; through inserting the catheter into their openings in the oral cavity; then applying lateral radiography immediately after the injection. The common carotid arteries were injected with red Latex Neoprene and dissected. The parotid gland was irregular rectangular and had five processes while the mandibular gland was irregular triangular with rounded proximal and pointed distal extremity. The parotid duct enters the oral cavity on the cheek opposite the upper 4th molar tooth. The mandibular duct opens in the oral cavity at the sublingual caruncles on the sublingual floor, just about 2cm cranial to frenulum linguae. Both The parotid and the mandibular salivary glands could be divided into four segments. -

Salivary Gland Infections and Salivary Stones (Sialadentis and Sialithiasis)
Salivary Gland Infections and Salivary Stones (Sialadentis and Sialithiasis) What is Sialadenitis and Sialithiasis? Sialdenitis is an infection of the salivary glands that causes painful swelling of the glands that produce saliva, or spit. Bacterial infections, diabetes, tumors or stones in the salivary glands, and tooth problems (poor oral hygiene) may cause a salivary gland infection. The symptoms include pain, swelling, pus in the mouth, neck skin infection. These infections and affect the submandibular gland (below the jaw) or the parotid glands (in front of the ears). The symptoms can be minor and just be a small swelling after meals (symptoms tend to be worse after times of high saliva flow). Rarely, the swelling in the mouth will progress and can cut off your airway and cause you to stop breathing. What Causes Sialadenitis and Sialithiasis When the flow of saliva is blocked by a small stone (salilithiasis) in a salivary gland or when a person is dehydrated, bacteria can build up and cause an infection. A viral infection, such as the mumps, also can cause a salivary gland to get infected and swell. These infections can also be caused by a spread from rotten or decaying teeth. Sometimes there can be a buildup of calcium in the saliva ducts that form into stones. These can easily stop the flow of saliva and cause problems How are these infections and stones treated? Treatment depends on what caused your salivary gland infection. If the infection is caused by bacteria, your doctor may prescribe antibiotics. Home treatment such as drinking fluids, applying warm compresses, and sucking on lemon wedges or sour candy to increase saliva may help to clear the infection quicker. -

Abscesses Apicectomy
BChD, Dip Odont. (Mondchir.) MBChB, MChD (Chir. Max.-Fac.-Med.) Univ. of Pretoria Co Reg: 2012/043819/21 Practice.no: 062 000 012 3323 ABSCESSES WHAT IS A TOOTH ABSCESS? A dental/tooth abscess is a localised acute infection at the base of a tooth, which requires immediate attention from your dentist. They are usually associated with acute pain, swelling and sometimes an unpleasant smell or taste in the mouth. More severe infections cause facial swelling as the bacteria spread to the nearby tissues of the face. This is a very serious condition. Once the swelling begins, it can spread rapidly. The pain is often made worse by drinking hot or cold fluids or biting on hard foods and may spread from the tooth to the ear or jaw on the same side. WHAT CAUSES AN ABSCESS? Damage to the tooth, an untreated cavity, or a gum disease can cause an abscessed tooth. If the cavity isn’t treated, the inside of the tooth can become infected. The bacteria can spread from the tooth to the tissue around and beneath it, creating an abscess. Gum disease causes the gums to pull away from the teeth, leaving pockets. If food builds up in one of these pockets, bacteria can grow, and an abscess may form. An abscess can cause the bone around the tooth to dissolve. WHY CAN'T ANTIBIOTIC TREATMENT ALONE BE USED? Antibiotics will usually help the pain and swelling associated with acute dental infections. However, they are not very good at reaching into abscesses and killing all the bacteria that are present. -

Head and Neck
DEFINITION OF ANATOMIC SITES WITHIN THE HEAD AND NECK adapted from the Summary Staging Guide 1977 published by the SEER Program, and the AJCC Cancer Staging Manual Fifth Edition published by the American Joint Committee on Cancer Staging. Note: Not all sites in the lip, oral cavity, pharynx and salivary glands are listed below. All sites to which a Summary Stage scheme applies are listed at the begining of the scheme. ORAL CAVITY AND ORAL PHARYNX (in ICD-O-3 sequence) The oral cavity extends from the skin-vermilion junction of the lips to the junction of the hard and soft palate above and to the line of circumvallate papillae below. The oral pharynx (oropharynx) is that portion of the continuity of the pharynx extending from the plane of the inferior surface of the soft palate to the plane of the superior surface of the hyoid bone (or floor of the vallecula) and includes the base of tongue, inferior surface of the soft palate and the uvula, the anterior and posterior tonsillar pillars, the glossotonsillar sulci, the pharyngeal tonsils, and the lateral and posterior walls. The oral cavity and oral pharynx are divided into the following specific areas: LIPS (C00._; vermilion surface, mucosal lip, labial mucosa) upper and lower, form the upper and lower anterior wall of the oral cavity. They consist of an exposed surface of modified epider- mis beginning at the junction of the vermilion border with the skin and including only the vermilion surface or that portion of the lip that comes into contact with the opposing lip. -

Basic Histology (23 Questions): Oral Histology (16 Questions
Board Question Breakdown (Anatomic Sciences section) The Anatomic Sciences portion of part I of the Dental Board exams consists of 100 test items. They are broken up into the following distribution: Gross Anatomy (50 questions): Head - 28 questions broken down in this fashion: - Oral cavity - 6 questions - Extraoral structures - 12 questions - Osteology - 6 questions - TMJ and muscles of mastication - 4 questions Neck - 5 questions Upper Limb - 3 questions Thoracic cavity - 5 questions Abdominopelvic cavity - 2 questions Neuroanatomy (CNS, ANS +) - 7 questions Basic Histology (23 questions): Ultrastructure (cell organelles) - 4 questions Basic tissues - 4 questions Bone, cartilage & joints - 3 questions Lymphatic & circulatory systems - 3 questions Endocrine system - 2 questions Respiratory system - 1 question Gastrointestinal system - 3 questions Genitouirinary systems - (reproductive & urinary) 2 questions Integument - 1 question Oral Histology (16 questions): Tooth & supporting structures - 9 questions Soft oral tissues (including dentin) - 5 questions Temporomandibular joint - 2 questions Developmental Biology (11 questions): Osteogenesis (bone formation) - 2 questions Tooth development, eruption & movement - 4 questions General embryology - 2 questions 2 National Board Part 1: Review questions for histology/oral histology (Answers follow at the end) 1. Normally most of the circulating white blood cells are a. basophilic leukocytes b. monocytes c. lymphocytes d. eosinophilic leukocytes e. neutrophilic leukocytes 2. Blood platelets are products of a. osteoclasts b. basophils c. red blood cells d. plasma cells e. megakaryocytes 3. Bacteria are frequently ingested by a. neutrophilic leukocytes b. basophilic leukocytes c. mast cells d. small lymphocytes e. fibrocytes 4. It is believed that worn out red cells are normally destroyed in the spleen by a. neutrophils b. -

Salivary Glands
GASTROINTESTINAL SYSTEM [Anatomy and functions of salivary gland] 1 INTRODUCTION Digestive system is made up of gastrointestinal tract (GI tract) or alimentary canal and accessory organs, which help in the process of digestion and absorption. GI tract is a tubular structure extending from the mouth up to anus, with a length of about 30 feet. GI tract is formed by two types of organs: • Primary digestive organs. • Accessory digestive organs 2 Primary Digestive Organs: Primary digestive organs are the organs where actual digestion takes place. Primary digestive organs are: Mouth Pharynx Esophagus Stomach 3 Anatomy and functions of mouth: FUNCTIONAL ANATOMY OF MOUTH: Mouth is otherwise known as oral cavity or buccal cavity. It is formed by cheeks, lips and palate. It encloses the teeth, tongue and salivary glands. Mouth opens anteriorly to the exterior through lips and posteriorly through fauces into the pharynx. Digestive juice present in the mouth is saliva, which is secreted by the salivary glands. 4 ANATOMY OF MOUTH 5 FUNCTIONS OF MOUTH: Primary function of mouth is eating and it has few other important functions also. Functions of mouth include: Ingestion of food materials. Chewing the food and mixing it with saliva. Appreciation of taste of the food. Transfer of food (bolus) to the esophagus by swallowing . Role in speech . Social functions such as smiling and other expressions. 6 SALIVARY GLANDS: The saliva is secreted by three pairs of major (larger) salivary glands and some minor (small) salivary glands. Major glands are: 1. Parotid glands 2. Submaxillary or submandibular glands 3. Sublingual glands. 7 Parotid Glands: Parotid glands are the largest of all salivary glands, situated at the side of the face just below and in front of the ear. -

SUBMANDIBULAR GLAND REMOVAL Post Operative Instructions
SUBMANDIBULAR GLAND REMOVAL Post Operative Instructions Nurse Line (8:30am to 5pm) 937-496-0261 Emergency After Hours Line 937-496-2600 The Surgery Itself Surgery to remove the submandibular gland involves general anesthesia, typically for about two hours. Patients may be quite sedated for several hours after surgery and may remain sleepy for much of the day. Nausea and vomiting are occasionally seen, and usually resolve by the evening of surgery - even without additional medications. Some patients stay overnight in the hospital; other patients can go home the evening of surgery. Some patients will have a drain in place after surgery; this is removed the following day before you go home from the hospital or in the office 1-2 days after surgery. Your Incision Your incision is closed with absorbable sutures and is covered with a small strip of tape or skin glue. You can shower and wash your hair as usual starting 24 hours after your drain is removed. If you did not have a drain in place after surgery, you may shower 24 hours after surgery. You may wash in a bathtub prior to that time if you are careful not to get your neck wet. Use a dab of Bacitracin ointment on your drain site (on one side of your incision, not covered by the tape or glue) before and after showering. Do not soak or scrub the incision. You might notice bruising around your incision or jaw line and slight swelling above the scar when you are upright. In addition, the scar may become pink and hard. -

Salivary Glands; the Parotid Submandibular and Sublingual Functions of Saliva
Lecture series Gastrointestinal tract Professor Shraddha Singh, Department of Physiology, KGMU, Lucknow Various secretions from GIT First secretion from GIT that encounter the food is SALIVARY SECRETIONS What is saliva • Saliva is the mixed glandular secretion which constantly bathes the teeth and the oral mucosa • First secretion encounter the food • It is vital for oral health • It is constituted by the secretions of the three paired major salivary glands; The Parotid Submandibular and Sublingual Functions of saliva 1. Defense: a. Antibacterial b. Antifungal c.Immunological 2. Digestive function: a. Digestive enzymes – ptyalin, lipase b. Formation of bolus c. Taste 3. Protective function: a. Protective coating for hard tissues-teeth b. Protective coating for soft tissues 4. Lubricative function: a.Keeps the oral cavity moist b.Facilitates speech c.Helps in mastication and swallowing 5. Buffering function Salivary glands Structure of Salivary Gland Parotid gland • Parotid is large accounts for 50% secretion of saliva • Situated in front of ear behind the ramus of mandible • Gland drain in to oral cavity opposite to second molar tooth • Secretions are basically serous Submandibular and Sub lingual gland • The submandibular gland is about half the size of the parotid gland • It lies above the mylohyoid in the floor of the mouth. It opens into the floor of the mouth underneath the anterior part of the tongue • The sublingual is the smallest of the paired major salivary glands, being about one fifth the size of the submandibular. • It -

Submandibular Gland Transfer for Prevention of Xerostomia After Radiation Therapy Swallowing Outcomes
ORIGINAL ARTICLE Submandibular Gland Transfer for Prevention of Xerostomia After Radiation Therapy Swallowing Outcomes Jana Rieger, PhD; Hadi Seikaly, MD; Naresh Jha, MBBS; Jeffrey Harris, MD; David Williams, MD; Richard Liu, MD; Tim McGaw, DDS; John Wolfaardt, PhD Objective: To assess swallowing outcomes in patients had preservation of 1 submandibular gland (SJP group) with oropharyngeal carcinoma in relation to the Seikaly- and 11 who did not (control group). Jha procedure for submandibular gland transfer (SJP). The SJP has recently been described as beneficial in the Main Outcome Measures: Quantitative and qualita- prevention of xerostomia induced by radiation therapy tive aspects of swallowing were obtained to determine in patients with head and neck cancer. whether patients in the SJP group performed more op- timally than those in the control group. Design: Inception cohort. Results: Baseline and stimulated salivary flow rates were Setting: University-affiliated primary care center. significantly different between groups. Patients in the SJP group were able to move the bolus through the oral cavity Patients: A phase 2 clinical trial was conducted from and into the pharynx faster than those in the control group. February 1, 1999, through February 28, 2002, to evalu- In addition, patients in the SJP group swallowed less often ate SJP in patients with head and neck cancer. During per bolus than patients in the control group. The com- that period, a consecutive sample of 51 patients who un- plete swallowing sequence was twice as long in controls. derwent surgical resection and reconstruction with a ra- dial forearm free flap for oropharyngeal carcinoma were Conclusions: The SJP for submandibular gland trans- referred for functional assessment of swallowing after fer appears to be beneficial in promoting more time- completion of adjuvant radiation therapy. -
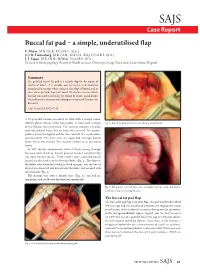
Buccal Fat Pad – a Simple, Underutilised Flap E
SAJS Case Report Buccal fat pad – a simple, underutilised flap E. Meyer, M.B. Ch.B., F.C.O.R.L. (S.A.) S. J. R. Liebenberg, M.B. Ch.B., M.R.C.S. (Ed.), F.C.O.R.L. (S.A.) J. J. Fagan, M.B. Ch.B., M.Med., F.C.O.R.L. (S.A.) Division of Otolaryngology, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital Summary The pedicled buccal fat pad is a reliable flap for the repair of small oral defects. It is durable, easy to harvest, and should be considered in settings where access to free flaps is limited and in cases where previous flaps have failed. We discuss a case in which this flap was used successfully for closure of an oro-antral fistula. The indications, anatomy and techniques of successful harvest are discussed. S Afr J Surg 2012;50(2):47-49. A 57-year-old woman presented in 1998 with a benign minor salivary gland tumour of the hard palate. A wide local excision Fig. 2. Buccal fat pad sutured to cover the oro-antral fistula. of the tumour was performed. The excision margins extended onto the palatal bone, but no bone was excised. The greater palatine artery was ligated and the bone was left to re-epithelialise spontaneously. Two years later, she again had a benign palatal lesion which was excised. The surgery resulted in an oro-antral fistula. In 2007 she was symptomatic, with all fluids coming through her nose when drinking. A local gingival mucosal rotational flap was done without success. -

Distribution and Roles of Substance P in Human Parotid Duct
IJAE Vol. 121, n. 3: 219-225, 2016 ITALIAN JOURNAL OF ANATOMY AND EMBRYOLOGY Research article - Histology and cell biology Distribution and roles of substance P in human parotid duct Kaori Amano1,*, Osamu Amano2, George Matsumura3, Kazuyuki Shimada4 1,3Department of Anatomy, Kyorin University School of Medicine; 2Department of Anatomy, Meikai University School of Dentistry; 4Kagoshima University Abstract Sialadenitis occurs with greatest frequency in the parotid glands because infection and inflam- mation arise easily from the oral cavity. Since patients often experience severe swelling and pain during inflammation, the distribution of sensory nerves in these ducts may have clini- cal significance. We used antibodies to the known neuropeptide substance P and to tyrosine hydroxylase - a marker of adrenergic fibres - to observe their distribution and gain insight on their functional role in adult human parotid duct. After excising the parotid duct along with the gland, specimens were divided into three regions: the tract adjacent to the parotid gland, the route along the anterior surface of the masseter, and the area where the duct penetrates the buc- cinator muscle and opens into the oral cavity. Specimens were prepared and examined under a fluorescence microscope following immunostaining. Substance P positivity was observed in all three regions of the duct, whereas tyrosine hydroxylase was distributed mainly in the vas- cular walls and surrounding areas. The distribution of substance P candidates this molecule to assist in tissue defense in conjunction with the blood and lymph vessels of this area. Tyrosine hydroxylase in the blood vessel wall likely contributes to regulation of blood flow in concert with substance P positive nerves surrounding the blood vessels. -

Oral & Maxillofacial Surgery Removal of Parotid Salivary Gland
Oxford University Hospitals NHS Trust Oral & Maxillofacial Surgery Removal of parotid salivary gland Information for patients This leaflet will help you understand your treatment and should answer many of the questions patients commonly ask before surgery for the removal of a parotid gland. A member of staff will be available if you would like further explanation and to answer any other questions that the leaflet does not cover. What is the parotid gland? The parotid gland lies in front of and below the earlobe. It produces saliva. Saliva drains from the parotid gland through a tube that opens on the inside of the cheek, opposite the upper back teeth. Why do I need my gland removed? The most common reason for removing a parotid gland (or part of the gland) is because a lump has been found inside it. There are also other reasons which your surgeon will discuss with you. What happens before the operation? Pre-assessment clinic – You will be asked to attend an appointment at this clinic. Nursing and/or medical staff will go through some important checks and make certain all relevant investigations have been completed well in advance of the operation date. Admission – You will normally be asked to come to Theatre Direct Admissions or Litchfield Day Surgery Unit on the morning of your operation. The anaesthetist will see you to explain the anaesthetic and answer any questions you may have. They will also be able to advise you about pain relief available after the operation. The surgeon will explain the details of the operation and discuss the possible risks, before asking you to sign a consent form (this may be done at the pre-assessment appointment).