Salivary Glands
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Parotid and Mandibular Salivary Glands Segmentation of the One Humped Dromedary Camel (Camelus Dromedarius)
Int. J. Adv. Res. Biol. Sci. (2017). 4(11): 32-41 International Journal of Advanced Research in Biological Sciences ISSN: 2348-8069 www.ijarbs.com DOI: 10.22192/ijarbs Coden: IJARQG(USA) Volume 4, Issue 11 - 2017 Research Article DOI: http://dx.doi.org/10.22192/ijarbs.2017.04.11.005 Parotid and Mandibular Salivary Glands Segmentation Of The One Humped Dromedary Camel (Camelus dromedarius) Hamdy M. Rezk and Nora A. Shaker* Department of Anatomy and Embryology, Faculty of Veterinary Medicine, Cairo University, Egypt *Corresponding author: [email protected] Abstract The present study provides detailed anatomical description of the parotid and mandibular salivary glands of the one humped camel with their segmentation based on arterial blood supply and salivary ducts; to facilitate partial removal of the pathologic gland. The shape, position, relations and blood supply of both salivary glands with their ducts were studied on six cadaveric heads. The mandibular and parotid ducts were injected with Urographin® as contrast medium; through inserting the catheter into their openings in the oral cavity; then applying lateral radiography immediately after the injection. The common carotid arteries were injected with red Latex Neoprene and dissected. The parotid gland was irregular rectangular and had five processes while the mandibular gland was irregular triangular with rounded proximal and pointed distal extremity. The parotid duct enters the oral cavity on the cheek opposite the upper 4th molar tooth. The mandibular duct opens in the oral cavity at the sublingual caruncles on the sublingual floor, just about 2cm cranial to frenulum linguae. Both The parotid and the mandibular salivary glands could be divided into four segments. -

Salivary Gland Infections and Salivary Stones (Sialadentis and Sialithiasis)
Salivary Gland Infections and Salivary Stones (Sialadentis and Sialithiasis) What is Sialadenitis and Sialithiasis? Sialdenitis is an infection of the salivary glands that causes painful swelling of the glands that produce saliva, or spit. Bacterial infections, diabetes, tumors or stones in the salivary glands, and tooth problems (poor oral hygiene) may cause a salivary gland infection. The symptoms include pain, swelling, pus in the mouth, neck skin infection. These infections and affect the submandibular gland (below the jaw) or the parotid glands (in front of the ears). The symptoms can be minor and just be a small swelling after meals (symptoms tend to be worse after times of high saliva flow). Rarely, the swelling in the mouth will progress and can cut off your airway and cause you to stop breathing. What Causes Sialadenitis and Sialithiasis When the flow of saliva is blocked by a small stone (salilithiasis) in a salivary gland or when a person is dehydrated, bacteria can build up and cause an infection. A viral infection, such as the mumps, also can cause a salivary gland to get infected and swell. These infections can also be caused by a spread from rotten or decaying teeth. Sometimes there can be a buildup of calcium in the saliva ducts that form into stones. These can easily stop the flow of saliva and cause problems How are these infections and stones treated? Treatment depends on what caused your salivary gland infection. If the infection is caused by bacteria, your doctor may prescribe antibiotics. Home treatment such as drinking fluids, applying warm compresses, and sucking on lemon wedges or sour candy to increase saliva may help to clear the infection quicker. -

Pediatric Oral Pathology. Soft Tissue and Periodontal Conditions
PEDIATRIC ORAL HEALTH 0031-3955100 $15.00 + .OO PEDIATRIC ORAL PATHOLOGY Soft Tissue and Periodontal Conditions Jayne E. Delaney, DDS, MSD, and Martha Ann Keels, DDS, PhD Parents often are concerned with “lumps and bumps” that appear in the mouths of children. Pediatricians should be able to distinguish the normal clinical appearance of the intraoral tissues in children from gingivitis, periodontal abnormalities, and oral lesions. Recognizing early primary tooth mobility or early primary tooth loss is critical because these dental findings may be indicative of a severe underlying medical illness. Diagnostic criteria and .treatment recommendations are reviewed for many commonly encountered oral conditions. INTRAORAL SOFT-TISSUE ABNORMALITIES Congenital Lesions Ankyloglossia Ankyloglossia, or “tongue-tied,” is a common congenital condition characterized by an abnormally short lingual frenum and the inability to extend the tongue. The frenum may lengthen with growth to produce normal function. If the extent of the ankyloglossia is severe, speech may be affected, mandating speech therapy or surgical correction. If a child is able to extend his or her tongue sufficiently far to moisten the lower lip, then a frenectomy usually is not indicated (Fig. 1). From Private Practice, Waldorf, Maryland (JED); and Department of Pediatrics, Division of Pediatric Dentistry, Duke Children’s Hospital, Duke University Medical Center, Durham, North Carolina (MAK) ~~ ~ ~ ~ ~ ~ ~ PEDIATRIC CLINICS OF NORTH AMERICA VOLUME 47 * NUMBER 5 OCTOBER 2000 1125 1126 DELANEY & KEELS Figure 1. A, Short lingual frenum in a 4-year-old child. B, Child demonstrating the ability to lick his lower lip. Developmental Lesions Geographic Tongue Benign migratory glossitis, or geographic tongue, is a common finding during routine clinical examination of children. -

Anatomy-Nerve Tracking
INJECTABLES ANATOMY www.aestheticmed.co.uk Nerve tracking Dr Sotirios Foutsizoglou on the anatomy of the facial nerve he anatomy of the human face has received enormous attention during the last few years, as a plethora of anti- ageing procedures, both surgical and non-surgical, are being performed with increasing frequency. The success of each of those procedures is greatly dependent on Tthe sound knowledge of the underlying facial anatomy and the understanding of the age-related changes occurring in the facial skeleton, ligaments, muscles, facial fat compartments, and skin. The facial nerve is the most important motor nerve of the face as it is the sole motor supply to all the muscles of facial expression and other muscles derived from the mesenchyme in the embryonic second pharyngeal arch.1 The danger zone for facial nerve injury has been well described. Confidence when approaching the nerve and its branches comes from an understanding of its three dimensional course relative to the layered facial soft tissue and being aware of surface anatomy landmarks and measurements as will be discussed in this article. Aesthetic medicine is not static, it is ever evolving and new exciting knowledge emerges every day unmasking the relationship of the ageing process and the macroscopic and microscopic (intrinsic) age-related changes. Sound anatomical knowledge, taking into consideration the natural balance between the different facial structures and facial layers, is fundamental to understanding these changes which will subsequently help us develop more effective, natural, long-standing and most importantly, safer rejuvenating treatments and procedures. The soft tissue of the face is arranged in five layers: 1) Skin; 2) Subcutaneous fat layer; 3) Superficial musculoaponeurotic system (SMAS); 4) Areolar tissue or loose connective tissue (most clearly seen in the scalp and forehead); 5) Deep fascia formed by the periosteum of facial bones and the fascial covering of the muscles of mastication (lateral face). -

Head and Neck
DEFINITION OF ANATOMIC SITES WITHIN THE HEAD AND NECK adapted from the Summary Staging Guide 1977 published by the SEER Program, and the AJCC Cancer Staging Manual Fifth Edition published by the American Joint Committee on Cancer Staging. Note: Not all sites in the lip, oral cavity, pharynx and salivary glands are listed below. All sites to which a Summary Stage scheme applies are listed at the begining of the scheme. ORAL CAVITY AND ORAL PHARYNX (in ICD-O-3 sequence) The oral cavity extends from the skin-vermilion junction of the lips to the junction of the hard and soft palate above and to the line of circumvallate papillae below. The oral pharynx (oropharynx) is that portion of the continuity of the pharynx extending from the plane of the inferior surface of the soft palate to the plane of the superior surface of the hyoid bone (or floor of the vallecula) and includes the base of tongue, inferior surface of the soft palate and the uvula, the anterior and posterior tonsillar pillars, the glossotonsillar sulci, the pharyngeal tonsils, and the lateral and posterior walls. The oral cavity and oral pharynx are divided into the following specific areas: LIPS (C00._; vermilion surface, mucosal lip, labial mucosa) upper and lower, form the upper and lower anterior wall of the oral cavity. They consist of an exposed surface of modified epider- mis beginning at the junction of the vermilion border with the skin and including only the vermilion surface or that portion of the lip that comes into contact with the opposing lip. -

Cheilitis Glandularis: Two Case Reports of Asian-Japanese Men and Literature Review of Japanese Cases
International Scholarly Research Network ISRN Dentistry Volume 2011, Article ID 457567, 6 pages doi:10.5402/2011/457567 Case Report Cheilitis Glandularis: Two Case Reports of Asian-Japanese Men and Literature Review of Japanese Cases Toru Yanagawa,1 Akira Yamaguchi,2 Hiroyuki Harada,3 Kenji Yamagata,1 Naomi Ishibashi,1 Masayuki Noguchi,4 Kojiro Onizawa,1 and Hiroki Bukawa1 1 Department of Oral and Maxillofacial Surgery, Clinical Sciences, Graduate School of Comprehensive Human Sciences, University of Tsukuba, 1-1-1 Tennodai, Tsukuba, Ibaraki, 305-8575, Japan 2 Section of Oral Pathology, Division of Oral Health Sciences, Department of Oral Restitution, Graduate School Medical and Dental Sciences, Tokyo Medical and Dental University, Tokyo 113-8549, Japan 3 Section of Oral and Maxillofacial Surgery, Division of Oral Health Sciences, Department of Oral Restitution, Graduate School Medical and Dental Sciences, Tokyo Medical and Dental University, Tokyo 113-8549, Japan 4 Department of Pathology, Life System Medical Sciences, Graduate School of Comprehensive Human Sciences, University of Tsukuba, 1-1-1 Tennodai, Tsukuba, Ibaraki 305-8575, Japan Correspondence should be addressed to Toru Yanagawa, [email protected] Received 25 October 2010; Accepted 5 December 2010 Academic Editor: G. L. Lodi Copyright © 2011 Toru Yanagawa et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Cheilitis glandularis (CG) is a rare disorder characterized by swelling of the lip with hyperplasia of the labial salivary glands. CG is most frequently encountered in the lower lip, in middle-aged to older Caucasian men; however Asian cases were rarely reported. -

Glands: a Correlation in Postmortem Subjects
J. clin. Path., 1970, 23, 690-694 Lymphocytic sialadenitis in the major and minor glands: a correlation in postmortem subjects D. M. CHISHOLM, J. P. WATERHOUSE, AND D. K. MASON From the Department of Oral Medicine and Pathology, University of Glasgow Dental Hospital and School, Glasgow, Scotland, and the Department of Oral Pathology, University ofIllinois, Chicago, USA SYNOPSIS In the present investigation, the prevalence offocal lymphocytic adenitis in the submandibular salivary gland was observed in a series of 116 postmortem subjects after suitable exclusions had been made. Focal lymphocytic adenitis could not be demonstrated in the labial salivary glands. The degree of lymphocytic infiltration in the labial salivary glands is positively correlated with the level of focal lymphocytic adenitis in the submandibular glands in the same subject. Lymphocytic foci and lymphocytic infiltrations found under these circumstances are probably related. This finding provides conceptual support for the examina- tion, by biopsy, of the labial glands in patients suspected of Sjogren's syndrome. The aim of the present study was to investigate muscle layer of the lower lip were excised at the prevalence and degree of lymphocytic sial- necropsy. Tissue was obtained from necropsies adenitis in the submandibular and minor labial at the Bernhard Baron Institute of Pathology, glands in a series of postmortem subjects. London Hospital, and the University Depart- Waterhouse (1963) has shown that the changes ment of Pathology, Royal Infirmary, Glasgow, observed in the submandibular gland in the between March and June 1967. They were taken postmortem subject reflect the degree of focal from all necropsies on fixed days of the week adenitis present in the parotid and lacrimal excepting a few not obtainable for administrative glands. -

Characteristics of the Saliva Flow Rates of Minor Salivary Glands in Healthy
a r c h i v e s o f o r a l b i o l o g y 6 0 ( 2 0 1 5 ) 3 8 5 – 3 9 2 Available online at www.sciencedirect.com ScienceDirect journal homepage: http://www.elsevier.com/locate/aob Characteristics of the saliva flow rates of minor salivary glands in healthy people a b a c a, Zhen Wang , Ming-Ming Shen , Xiao-Jing Liu , Yan Si , Guang-Yan Yu * a Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology, 100081, Beijing, PR China b Department of Oral and Maxillofacial Surgery, School of Stomatology, the Second Hospital of Hebei Medical University, 050000, Shijiazhuang, PR China c Department of Preventive Dentistry, Peking University School and Hospital of Stomatology, 100081, Beijing, PR China a r t i c l e i n f o a b s t r a c t Article history: Objectives: To investigate the normal range and characteristics of saliva secretion in the Accepted 23 November 2014 minor salivary glands (MSGs). Design: The flow rates of MSGs were measured in 4 anatomical locations of oral mucosa, and Keywords: the relationship between MSG flow rates and whole saliva flow rates were assessed in 300 healthy subjects stratified by age and sex. An additional 30 young females were further Minor salivary gland Saliva evaluated for flow symmetry, effects of stimulation, circadian effects in MSGs, and the relationship with the flow rates of major salivary glands. Saliva secretion Results: (1) The mean saliva flow rates were 2.10 Æ 0.66 (lower labial glands), 2.14 Æ 0.62 Saliva flow rate 2 (upper labial glands), 2.88 Æ 0.72 (buccal glands) and 2.15 Æ 0.51 (palatal glands) ml/min/cm , Salivary gland respectively. -

Salivary Glands Massage
Patient Education Sheet How to Massage Salivary Glands The Foundation thanks Ava J. Wu, DDS for authoring this Patient Education Sheet. Dr. Wu is a Clinical Professor and Co-Director of the Salivary Gland Dysfunction Clinic, School of Dentistry, University of California, San Fr anci sc o. If a sharp and stabbing pain occurs in one of your salivary glands right before or while eating or drinking, the cause might be an obstruction (a stone or mucous plug). In rare cases, associated gland swelling can accompany the discomfort. Here are some tips for massaging or “milking” the gland that might help: Figure 1A: The parotid glands are 2A located bilaterally in the cheek area in front of your ear and have a “tail” area that can extend over the lower jaw. 1A Figure 2A: The submandibular and sublingual glands are located bilaterally under your jaw and 2B tongue with the sublingual gland closer to the chin. Figures 1B and 2B: Place two fingers on the body or 1B tail area of the parotid, Or under the jaw for the submandibular/sublingual glands. 2C Figures 1C and 2C: Sweep fingers forward with gentle pressure as indicated by the black arrows. This will 1C encourage movement of saliva past a possible obstruction or constriction and into the oral cavity. Additional Tips: • Stay well hydrated to encourage the flow of saliva through the gland. • Temporarily avoid foods and beverages that cause the pain and possible swelling. • Apply warm compresses to the area to increase comfort. • Ibuprofen may be taken temporarily to decrease pain and inflammation. -
Buccal Fat Pad – a Simple, Underutilised Flap E
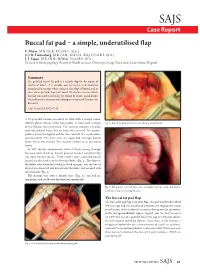
SAJS Case Report Buccal fat pad – a simple, underutilised flap E. Meyer, M.B. Ch.B., F.C.O.R.L. (S.A.) S. J. R. Liebenberg, M.B. Ch.B., M.R.C.S. (Ed.), F.C.O.R.L. (S.A.) J. J. Fagan, M.B. Ch.B., M.Med., F.C.O.R.L. (S.A.) Division of Otolaryngology, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital Summary The pedicled buccal fat pad is a reliable flap for the repair of small oral defects. It is durable, easy to harvest, and should be considered in settings where access to free flaps is limited and in cases where previous flaps have failed. We discuss a case in which this flap was used successfully for closure of an oro-antral fistula. The indications, anatomy and techniques of successful harvest are discussed. S Afr J Surg 2012;50(2):47-49. A 57-year-old woman presented in 1998 with a benign minor salivary gland tumour of the hard palate. A wide local excision Fig. 2. Buccal fat pad sutured to cover the oro-antral fistula. of the tumour was performed. The excision margins extended onto the palatal bone, but no bone was excised. The greater palatine artery was ligated and the bone was left to re-epithelialise spontaneously. Two years later, she again had a benign palatal lesion which was excised. The surgery resulted in an oro-antral fistula. In 2007 she was symptomatic, with all fluids coming through her nose when drinking. A local gingival mucosal rotational flap was done without success. -

Distribution and Roles of Substance P in Human Parotid Duct
IJAE Vol. 121, n. 3: 219-225, 2016 ITALIAN JOURNAL OF ANATOMY AND EMBRYOLOGY Research article - Histology and cell biology Distribution and roles of substance P in human parotid duct Kaori Amano1,*, Osamu Amano2, George Matsumura3, Kazuyuki Shimada4 1,3Department of Anatomy, Kyorin University School of Medicine; 2Department of Anatomy, Meikai University School of Dentistry; 4Kagoshima University Abstract Sialadenitis occurs with greatest frequency in the parotid glands because infection and inflam- mation arise easily from the oral cavity. Since patients often experience severe swelling and pain during inflammation, the distribution of sensory nerves in these ducts may have clini- cal significance. We used antibodies to the known neuropeptide substance P and to tyrosine hydroxylase - a marker of adrenergic fibres - to observe their distribution and gain insight on their functional role in adult human parotid duct. After excising the parotid duct along with the gland, specimens were divided into three regions: the tract adjacent to the parotid gland, the route along the anterior surface of the masseter, and the area where the duct penetrates the buc- cinator muscle and opens into the oral cavity. Specimens were prepared and examined under a fluorescence microscope following immunostaining. Substance P positivity was observed in all three regions of the duct, whereas tyrosine hydroxylase was distributed mainly in the vas- cular walls and surrounding areas. The distribution of substance P candidates this molecule to assist in tissue defense in conjunction with the blood and lymph vessels of this area. Tyrosine hydroxylase in the blood vessel wall likely contributes to regulation of blood flow in concert with substance P positive nerves surrounding the blood vessels. -

Oral & Maxillofacial Surgery Removal of Parotid Salivary Gland
Oxford University Hospitals NHS Trust Oral & Maxillofacial Surgery Removal of parotid salivary gland Information for patients This leaflet will help you understand your treatment and should answer many of the questions patients commonly ask before surgery for the removal of a parotid gland. A member of staff will be available if you would like further explanation and to answer any other questions that the leaflet does not cover. What is the parotid gland? The parotid gland lies in front of and below the earlobe. It produces saliva. Saliva drains from the parotid gland through a tube that opens on the inside of the cheek, opposite the upper back teeth. Why do I need my gland removed? The most common reason for removing a parotid gland (or part of the gland) is because a lump has been found inside it. There are also other reasons which your surgeon will discuss with you. What happens before the operation? Pre-assessment clinic – You will be asked to attend an appointment at this clinic. Nursing and/or medical staff will go through some important checks and make certain all relevant investigations have been completed well in advance of the operation date. Admission – You will normally be asked to come to Theatre Direct Admissions or Litchfield Day Surgery Unit on the morning of your operation. The anaesthetist will see you to explain the anaesthetic and answer any questions you may have. They will also be able to advise you about pain relief available after the operation. The surgeon will explain the details of the operation and discuss the possible risks, before asking you to sign a consent form (this may be done at the pre-assessment appointment).