Oral Medicine:11. Lumps and Swellings: Mouth
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Lumps and Swellings
Clinical Oral medicine for the general practitioner: lumps and swellings Crispian Scully 1 his series of five papers summarises some of the most important oral medicine problems likely to be Tencountered by practitioners. Some are common, others rare. The practitioner cannot be expected to diagnose all, but has been trained to recognise oral health and disease, and should be competent to recognise normal variants, and common orofacial disorders. In any case of doubt, the practitioner is advised to seek a second opinion from a colleague. The series is not intended to be comprehensive in coverage either of the conditions encountered, or all aspects of Figure 1: Torus mandibularis. diagnosis or treatment: further details are available in standard texts, in the further reading section, or from the internet. The present article discusses aspects of lumps through fear, perhaps after hearing of someone with and swellings. ‘mouth cancer’. Thus some individuals discover and worry about normal anatomical features such as tori, the parotid Lumps and swellings papilla, foliate papillae on the tongue, or the pterygoid Lumps and swellings in the mouth are common, but of hamulus. The tongue often detects even a very small diverse aetiologies (Table 1), and some represent swelling, or the patient may first notice it because it is sore malignant neoplasms. Therefore, this article will discuss (Figure 1). In contrast, many oral cancers are diagnosed far lumps and swellings in general terms, but later focus on too late, often after being present several months, usually the particular problems of oral cancer and of orofacial because the patient ignores the swelling. -

Glossary for Narrative Writing
Periodontal Assessment and Treatment Planning Gingival description Color: o pink o erythematous o cyanotic o racial pigmentation o metallic pigmentation o uniformity Contour: o recession o clefts o enlarged papillae o cratered papillae o blunted papillae o highly rolled o bulbous o knife-edged o scalloped o stippled Consistency: o firm o edematous o hyperplastic o fibrotic Band of gingiva: o amount o quality o location o treatability Bleeding tendency: o sulcus base, lining o gingival margins Suppuration Sinus tract formation Pocket depths Pseudopockets Frena Pain Other pathology Dental Description Defective restorations: o overhangs o open contacts o poor contours Fractured cusps 1 ww.links2success.biz [email protected] 914-303-6464 Caries Deposits: o Type . plaque . calculus . stain . matera alba o Location . supragingival . subgingival o Severity . mild . moderate . severe Wear facets Percussion sensitivity Tooth vitality Attrition, erosion, abrasion Occlusal plane level Occlusion findings Furcations Mobility Fremitus Radiographic findings Film dates Crown:root ratio Amount of bone loss o horizontal; vertical o localized; generalized Root length and shape Overhangs Bulbous crowns Fenestrations Dehiscences Tooth resorption Retained root tips Impacted teeth Root proximities Tilted teeth Radiolucencies/opacities Etiologic factors Local: o plaque o calculus o overhangs 2 ww.links2success.biz [email protected] 914-303-6464 o orthodontic apparatus o open margins o open contacts o improper -

WHAT HAPPENED? CDR, a 24-Year-Old Chinese Male
CHILDHOOD DEVELOPMENTAL SCREENING 2020 https://doi.org/10.33591/sfp.46.5.up1 FINDING A MASS WITHIN THE ORAL CAVITY: WHAT ARE THE COMMON CAUSES AND 4-7 GAINING INSIGHT: WHAT ARE THE ISSUES? In Figure 2 below, a list of masses that could arise from each site Figure 3. Most common oral masses What are the common salivary gland pathologies Salivary gland tumours (Figure 7) commonly present as channel referrals to appropriate specialists who are better HOW SHOULD A GP MANAGE THEM? of the oral cavity is given and elaborated briey. Among the that a GP should be aware of? painless growing masses which are usually benign. ey can equipped in centres to accurately diagnose and treat these Mr Tan Tai Joum, Dr Marie Stella P Cruz CDR had a slow-growing mass in the oral cavity over one year more common oral masses are: torus palatinus, torus occur in both major and minor salivary glands but are most patients, which usually involves surgical excision. but sought treatment only when he experienced a sudden acute mandibularis, pyogenic granuloma, mucocele, broma, ere are three pairs of major salivary glands (parotid, commonly found occurring in the parotid glands. e most 3) Salivary gland pathology may be primary or secondary to submandibular and sublingual) as well as hundreds of minor ABSTRACT onset of severe pain and numbness. He was fortunate to have leukoplakia and squamous cell carcinoma – photographs of common type of salivary gland tumour is the pleomorphic systemic causes. ese dierent diseases may present with not sought treatment as it had not caused any pain. -
Mandibular Tori
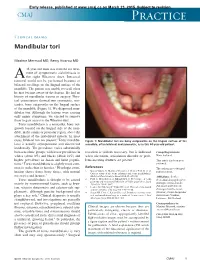
Early release, published at www.cmaj.ca on March 23, 2015. Subject to revision. CMAJ Practice Clinical images Mandibular tori Maxime Mermod MD, Remy Hoarau MD 44-year-old man was referred for treat- ment of symptomatic sialolithiasis in A the right Wharton duct. Intraoral removal could not be performed because of bilateral swellings on the lingual surface of the mandible. The patient was unable to recall when he first became aware of the lesions. He had no history of mandibular trauma or surgery. Phys- ical examination showed two symmetric, non- tender, bony outgrowths on the lingual surface of the mandible (Figure 1). We diagnosed man- dibular tori. Although the lesions were causing only minor symptoms, we elected to remove them to gain access to the Wharton duct. Torus mandibularis is a nontender, bony out- growth located on the lingual side of the man- dible, in the canine or premolar region, above the attachment of the mylohyoid muscle. In most 1 cases, bilateral tori are present. Torus mandibu- Figure 1: Mandibular tori are bony outgrowths on the lingual surface of the laris is usually asymptomatic and discovered mandible, often bilateral and symmetric, as in this 44-year-old patient. incidentally. The prevalence varies substantially between ethnic groups, with lower prevalence in resection is seldom necessary, but is indicated Competing interests: whites (about 8%) and blacks (about 16%) and when ulceration, articulation disorder or prob- None declared. higher prevalence in Asian and Inuit popula- lems inserting dentures are present.3 This article has been peer tions.2 Torus mandibularis is slightly more com- reviewed. -

Abscesses Apicectomy
BChD, Dip Odont. (Mondchir.) MBChB, MChD (Chir. Max.-Fac.-Med.) Univ. of Pretoria Co Reg: 2012/043819/21 Practice.no: 062 000 012 3323 ABSCESSES WHAT IS A TOOTH ABSCESS? A dental/tooth abscess is a localised acute infection at the base of a tooth, which requires immediate attention from your dentist. They are usually associated with acute pain, swelling and sometimes an unpleasant smell or taste in the mouth. More severe infections cause facial swelling as the bacteria spread to the nearby tissues of the face. This is a very serious condition. Once the swelling begins, it can spread rapidly. The pain is often made worse by drinking hot or cold fluids or biting on hard foods and may spread from the tooth to the ear or jaw on the same side. WHAT CAUSES AN ABSCESS? Damage to the tooth, an untreated cavity, or a gum disease can cause an abscessed tooth. If the cavity isn’t treated, the inside of the tooth can become infected. The bacteria can spread from the tooth to the tissue around and beneath it, creating an abscess. Gum disease causes the gums to pull away from the teeth, leaving pockets. If food builds up in one of these pockets, bacteria can grow, and an abscess may form. An abscess can cause the bone around the tooth to dissolve. WHY CAN'T ANTIBIOTIC TREATMENT ALONE BE USED? Antibiotics will usually help the pain and swelling associated with acute dental infections. However, they are not very good at reaching into abscesses and killing all the bacteria that are present. -

Orofacial Granulomatosis
Al-Hamad, A; Porter, S; Fedele, S; (2015) Orofacial Granulomatosis. Dermatol Clin , 33 (3) pp. 433- 446. 10.1016/j.det.2015.03.008. Downloaded from UCL Discovery: http://discovery.ucl.ac.uk/1470143 ARTICLE Oro-facial Granulomatosis Arwa Al-Hamad1, 2, Stephen Porter1, Stefano Fedele1, 3 1 University College London, UCL Eastman Dental Institute, Oral Medicine Unit, 256 Gray’s Inn Road, WC1X 8LD, London UK. 2 Dental Services, King Abdulaziz Medical City-Riyadh, Ministry of National Guard, Riyadh, Saudi Arabia. 3 NIHR University College London Hospitals Biomedical Research Centre, London, UK. Acknowledgments: Part of this work was undertaken at University College London/University College London Hospital, which received a proportion of funding from the Department of Health’s National Institute for Health Research Biomedical Research Centre funding scheme. Conflicts of Interest: The authors declare that they have no affiliation with any organization with a financial interest, direct or indirect, in the subject matter or materials discussed in the manuscript that may affect the conduct or reporting of the work submitted. Authorship: all authors named above meet the following criteria of the International Committee of Medical Journal Editors: 1) Substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data; 2) Drafting the article or revising it critically for important intellectual content; 3) Final approval of the version to be published. Corresponding author: Dr. Stefano Fedele DDS, PhD -

Recognition and Management of Oral Health Problems in Older Adults by Physicians: a Pilot Study
J Am Board Fam Pract: first published as 10.3122/jabfm.11.6.474 on 1 November 1998. Downloaded from BRIEF REPORTS Recognition and Management of Oral Health Problems in Older Adults by Physicians: A Pilot Study Thomas V. Jones, MD, MPH, Mitchel J Siegel, DDS, andJohn R. Schneider, A1A Oral health problems are among the most com of the nation's current and future health care mon chronic health conditions experienced by needs, the steady increase in the older adult popu older adults. Healthy People 2000, an initiative to lation, and the generally high access elderly per improve the health of America, has selected oral sons have to medical care provided by family health as a priority area. l About 11 of 100,000 physicians and internists.s,7,8 Currently there is persons have oral cancer diagnosed every year.2 very little information about the ability of family The average age at which oral cancer is diagnosed physicians or internists, such as geriatricians, to is approximately 65 years, with the incidence in assess the oral health of older patients. We con creasing from middle adulthood through the sev ducted this preliminary study to determine how enth decade of life. l-3 Even though the mortality family physicians and geriatricians compare with rate associated with oral cancer (7700 deaths an each other and with general practice dentists in nually)4 ranks among the lowest compared with their ability to recognize, diagnose, and perform other cancers, many deaths from oral cancer initial management of a wide spectrum of oral might be prevented by improved case finding and health problems seen in older adults. -

Orofacial Granulomatosis Presenting As Gingival Enlargement – Report of Three Cases
Open Access Journal of Dentistry & Oral Disorders Case Report Orofacial Granulomatosis Presenting as Gingival Enlargement – Report of Three Cases Savithri V*, Janardhanan M, Suresh R and Aravind T Abstract Department of Oral Pathology & Microbiology, Amrita Orofacial Granulomatosis (OFG) is an uncommon disease characterized School of Dentistry, Amrita VishwaVidyapeetham, Amrita by non-caseating granulomatous inflammation in the oral and maxillofacial University, India region. They present clinically as labial enlargement, perioral and/or mucosal *Corresponding author: Vindhya Savithri, swelling, angular cheilitis, mucosal tags, vertical fissures of lips, lingua plicata, Department of Oral Pathology & Microbiology, Amrita oral ulcerations and gingival enlargement. The term OFG was introduced by School of Dentistry, Amrita VishwaVidyapeetham, Amrita Wiesenfeld in 1985. The diagnosis of OFG is done by the clinical presentation University, India and histological picture and this may be further complicated by the fact that OFG may be the oral manifestation of a systemic condition, such as Crohn’s Received: October 16, 2017; Accepted: November 27, disease, sarcoidosis, or, more rarely, Wegener’s granulomatosis. In addition, 2017; Published: December 04, 2017 several conditions, including tuberculosis, leprosy, systemic fungal infections, and foreign body reactions may show granulomatous inflammation on histologic examination. They have to be excluded out by appropriate investigations. They have to be excluded out by appropriate investigations. -

Orofacial Granulomatosis: a Review
DOI Number: 10.5958/0974-1283.2019.00181.6 Orofacial Granulomatosis: A Review Saloni Banga1, M K Sunil2, Hina Padaliya1 1Intern, 2Professor and Head of Department, Department of Oral Medicine & Radiology, Teerthanker Mahaveer Dental College & Research Center Moradabad Abstract Orofacial Granulomatosis (OFG) is an uncommon clinicopathological entity characterized clinically by the presence of persistent enlargement of the soft tissues of the oral and maxillofacial region and histologically by non-caseating and non-necrotizing granulomatous inflammation. The term ‘orofacial granulomatosis’ has been introduced to denote the group of various disorders, including Melkersson-Rosenthal syndrome and granulomatous cheilitis and has been noted to be associated with Crohn’s disease, Sarcoidosis and infectious diseases such as Tuberculosis. Although, various etiological agents such as dental materials, food additives and microbial agents have been recommended in the disease process. Treatment of orofacial granulomatosis is by corticosteroids but it’s not so efficient. It is more important to identify the pathogen first to specify the appropriate treatment line. Keywords— orofacial granulomatosis, Melkersson Rosenthal syndrome, crohn,s disease. Introduction Definition and its associated to other granulomatous disorders Orofacial granulomatosis term was introduced by Wiesenfeld in 19851. Granulomatosis is any condition Orofacial granulomatosis is an uncommon disorder1 characterized by the formation of multiple nodules or but is increasingly recognized. Orofacial granulomatosis granulomas in soft tissues. It encompasses Melkersson (as defined by Wiesenfeld in 1985) is the specific Rosenthal syndrome and Cheilitis granulomatosa1. histological finding of granulomas in mucosal or skin The true prevalence of this disease is unknown but is biopsies taken from the mouth or face in the absence suggested to be 0.8% (Mahler and Kiesewetter, 1996)3. -

Cinnamon Products As a Possible Etiologic Factor in Orofacial Granulomatosis
Med Oral Patol Oral Cir Bucal. 2007 Oct 1;12(6):E440-4. Orofacial granulomatosis caused by cinnamon flavoring Med Oral Patol Oral Cir Bucal 2007;12:E440-4. Orofacial granulomatosis caused by cinnamon flavoring Cinnamon products as a possible etiologic factor in orofacial granulomatosis Hiroyasu Endo 1, Terry D. Rees 2 (1) Assistant Professor, Department of Periodontology, Nihon University, School of Dentistry at Matsudo, Japan (2) Professor and Former Chairman, Director of Stomatology, Department of Periodontics, Baylor College of Dentistry, Texas A&M University Health Science Center, Dallas, TX, USA Correspondence: Dr. Hiroyasu Endo Dept. of Periodontology Nihon University School of Dentistry at Matsudo 2-870-1 Sakaecho Nishi, Matsudo Chiba, Japan. 271-8587 E-mail: [email protected] Endo H, Rees TD. Cinnamon products as a possible etiologic factor Received: 17-09-2006 Accepted: 25-03-2007 in orofacial granulomatosis. Med Oral Patol Oral Cir Bucal. 2007 Oct 1;12(6):E440-4. © Medicina Oral S. L. C.I.F. B 96689336 - ISSN 1698-6946 Indexed in: -Index Medicus / MEDLINE / PubMed -EMBASE, Excerpta Medica -SCOPUS -Indice Médico Español -IBECS ABStract Objectives: It has been reported that clinical changes due to hypersensitivity reactions to various foods, preservatives, and oral hygiene products may be consistent with the characteristic signs of orofacial granulomatosis (OFG). The ob- jective of this study was to examine 37 well-documented cases of cinnamon-induced contact stomatitis for clinical and histological features consistent with a diagnosis of OFG. Study design: We reviewed the records of the 37 cases to screen them for the clinical and histopathologic features of OFG. -

Oral and Maxillo-Facial Manifestations of Systemic Diseases: an Overview
medicina Review Oral and Maxillo-Facial Manifestations of Systemic Diseases: An Overview Saverio Capodiferro *,† , Luisa Limongelli *,† and Gianfranco Favia Department of Interdisciplinary Medicine, University of Bari Aldo Moro, Piazza G. Cesare, 11, 70124 Bari, Italy; [email protected] * Correspondence: [email protected] (S.C.); [email protected] (L.L.) † These authors contributed equally to the paper. Abstract: Many systemic (infective, genetic, autoimmune, neoplastic) diseases may involve the oral cavity and, more generally, the soft and hard tissues of the head and neck as primary or secondary localization. Primary onset in the oral cavity of both pediatric and adult diseases usually represents a true challenge for clinicians; their precocious detection is often difficult and requires a wide knowledge but surely results in the early diagnosis and therapy onset with an overall better prognosis and clinical outcomes. In the current paper, as for the topic of the current Special Issue, the authors present an overview on the most frequent clinical manifestations at the oral and maxillo-facial district of systemic disease. Keywords: oral cavity; head and neck; systemic disease; oral signs of systemic diseases; early diagnosis; differential diagnosis Citation: Capodiferro, S.; Limongelli, 1. Introduction L.; Favia, G. Oral and Maxillo-Facial Oral and maxillo-facial manifestations of systemic diseases represent an extensive and Manifestations of Systemic Diseases: fascinating study, which is mainly based on the knowledge that many signs and symptoms An Overview. Medicina 2021, 57, 271. as numerous systemic disorders may first present as or may be identified by head and https://doi.org/10.3390/ neck tissue changes. -

Orofacial Granulomatosis
Division of Oral Medicine and Dentistry Orofacial Granulomatosis What is orofacial granulomatosis? How do we know it is OFG? Orofacial granulomatosis (OFG) is an uncommon condition of A dental specialist can usually diagnose OFG based on a good the mouth that causes lip swelling, and sometimes swelling of history, a thorough clinical examination, and a biopsy to the face, inner cheeks, and the gums. Tis swelling may come confrm the diagnosis. You may be sent to a specialist who can and go at frst, but over time, becomes persistent if not treated. perform a patch test of your skin to see if you are sensitive to Patients will typically describe their symptoms as swelling and foods, food preservatives or other substances. Te results of the tightness and sometimes, soreness. In addition, there may be patch test may help your doctor to suggest the best treatment some folding of the inside of the mouth giving it a “cobblestone” option for your disease. Patients may be referred to appearance. OFG may be part of Melkersson-Rosenthal a gastrointestinal specialist if a diagnosis of Crohn disease syndrome, a rare condition that consists of OFG, fssured is suspected. tongue (tongue with deep grooves) and paralysis of the face. How do we treat OFG? What causes OFG? A food diary can be helpful if food sensitivity is suspected or It is likely that patients with OFG are reacting to something confrmed by patch testing, and completely avoiding such foods although this is not always easy to identify. Some common may substantially reduce swelling. Te doctor who patch tested triggers are foods and food preservatives such as chocolate, you will provide you with a list of substances to avoid if you cinnamon favorings, and preservatives such as benzoates and patch tested positive to them.