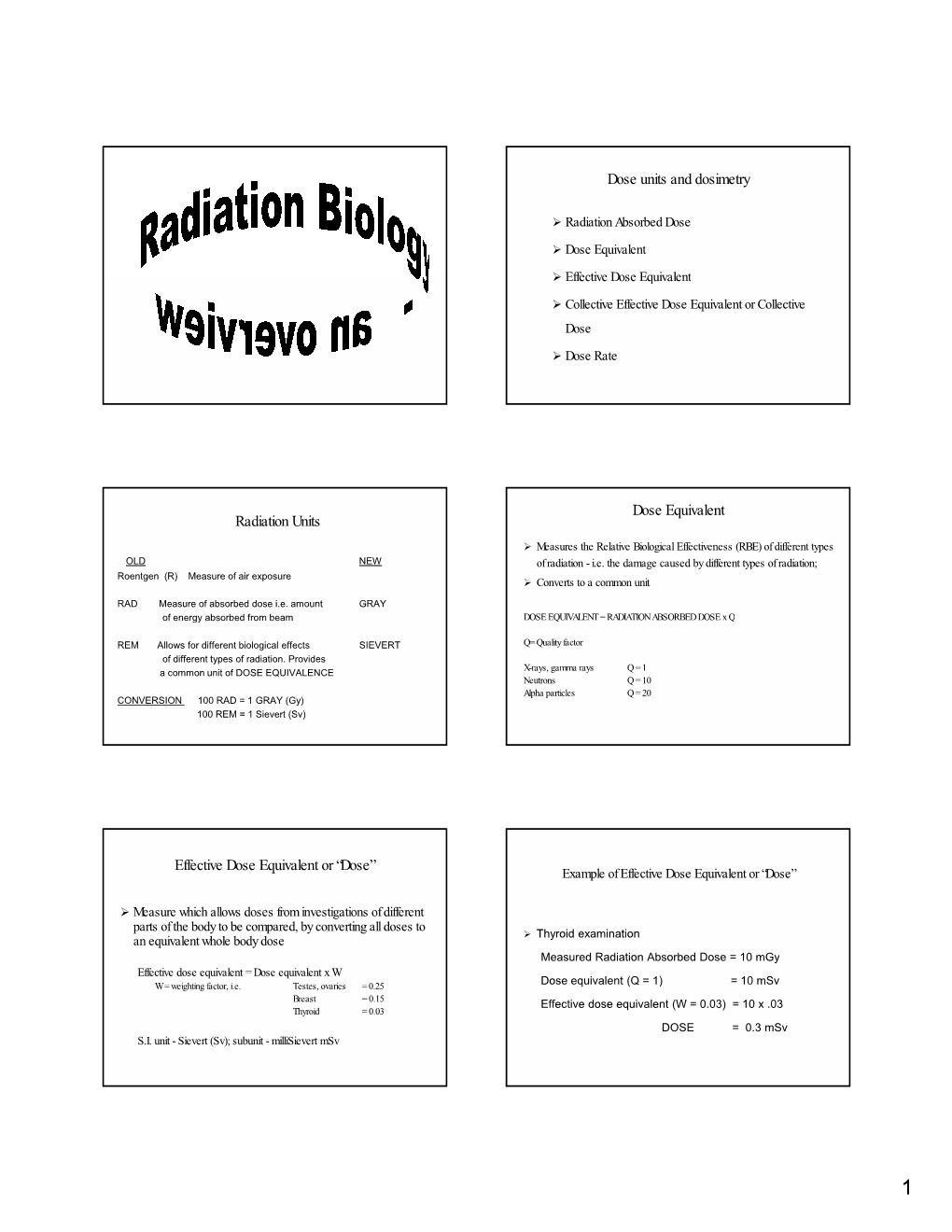
Dose Units and Dosimetry Radiation Units Dose Equivalent Effective Dose Equivalent Or “Dose”
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Absorbed Dose in Radioactive Media Outline Introduction Radiation Equilibrium Charged-Particle Equilibrium Limiting Cases
Outline • General dose calculation considerations, Absorbed Dose in Radioactive absorbed fraction Media • Radioactive disintegration processes and associated dose deposition – Alpha disintegration Chapter 5 – Beta disintegration – Electron-capture transitions F.A. Attix, Introduction to Radiological – Internal conversion Physics and Radiation Dosimetry • Summary Introduction Radiation equilibrium • We are interested in calculating the absorbed dose in a. The atomic composition radioactive media, applicable to cases of of the medium is – Dose within a radioactive organ homogeneous – Dose in one organ due to radioactive source in another b. The density of the organ medium is • If conditions of CPE or RE are satisfied, dose homogeneous c. The radioactive source calculation is straightforward is uniformly distributed • Intermediate situation is more difficult but can be d. No external electric or handled at least in approximations magnetic fields are present Charged-particle equilibrium Limiting cases • Emitted radiation typically includes both • Each charged particle of a given type and photons (longer range) and charged energy leaving the volume is replaced by an particles (shorter range) identical particle of the same energy entering • Assume the conditions for RE are satisfied the volume • Consider two • Existence of RE is sufficient condition for CPE limited cases based • Even if RE does not exist CPE may still exist on the size of the (for a very large or a very small volume) radioactive object 1 Limiting cases: small object Limiting -

Nuclear Radiation 1. an Atom Contains Electrons, Protons and Neutrons
Nuclear Radiation 1. An atom contains electrons, protons and neutrons. Which of these particles a) are outside the nucleus b) are uncharged c) have a negative charge d) are nucleons e) are much lighter than the others? 2. Complete the table below. Name Symbol Charge What is it? Alpha particle β -1 Gamma ray An electromagnetic wave 3. How is an ionised material different from a material that is not ionised? National 5 Physics: Waves & Radiation 1 Absorption of Radiation 1. The figure below shows a Geiger tube used to detect radiation from a radioactive source. thick lead plate 0 4 2 5 start counter stop ON OFF reset Geiger tube radioactive source The following measurements were made using the apparatus above. Counts in 300 seconds Readings Average 1 No source present 102 94 110 2 Source present at fixed distance from tube a) No lead plate present 3466 3420 3410 b) Thick lead plate present 105 109 89 c) Aluminium sheet in place of the 1834 1787 1818 thick lead sheet a) Complete the table by calculating the average readings. b) Why are the readings on each line not the same? c) What can you say from the table about the effect on the radiation of: i. The lead plate? ii. The aluminium plate? d) Why is it possible to say from the readings that: i. gamma radiation is emitted by the source? ii. alpha and beta radiation might be emitted by the source? e) What further tests could you make using this arrangement to find out whether or not the source emits alpha radiation? National 5 Physics: Waves & Radiation 2 2. -

Copyright by Arthur Bryan Crawford 2004
Copyright by Arthur Bryan Crawford 2004 The Dissertation Committee for Arthur Bryan Crawford Certifies that this is the approved version of the following dissertation: Evaluation of the Impact of Non -Uniform Neutron Radiation Fields on the Do se Received by Glove Box Radiation Workers Committee: Steven Biegalski, Supervisor Sheldon Landsberger John Howell Ofodike Ezekoye Sukesh Aghara Evaluation of the Impact of Non -Uniform Neutron Radiation Fields on the Dose Received by Glove Box Radiation Workers by Arthur Bryan Crawford, B.S., M.S. Dissertation Presented to the Faculty of the Graduate School of The University of Texas at Austin in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy The University of Texas at Austin December, 2004 Dedication I was born to goodly parents Harvey E. Crawford and Johnnie Lee Young Crawford Acknowledgements I would like to express my gratitude to Dr. Sheldon Landsberger for his vision in starting a distance learning program at the University of Texas at Austin and for his support and encouragement on this quest. I would like to thank my advisor, Dr. Steven Biegalski, for his support and encouragement even though the topic area was new to him. I would like to thank the members of my dissertation committee for finding the time to review this dissertation. To the staff of the Nuclear Engineering Teaching Laboratory I say thank you for your kindness and support during those brief times that I was on cam pus. A special thanks to my past and present group leaders, David Seidel, Eric McNamara, and Bill Eisele and my Division Leader, Lee McAtee, at Los Alamos National Laboratory, for their support in being allowed to use time and material resources at the Lab oratory and for financial support in the form of tuition reimbursement and travel expenses. -

Industrial Radiography
RADIATION PROTECTION OF WORKERS Industrial Radiography RADIATION AND RADIOGRAPHS RADIOACTIVE SOURCES PROCEDURES RADIOGRAPHERS DO follow the procedures. Ionizing radiation can pen- Materials of higher den Sealed sources are small þ Safe storage Precautions þ DO use the appropriate equipment, including collimators. in size and contain material etrate objects and create sity absorb more radiation. þ DO confi rm that there are no other people working in the images on photographic The metal components are which emits penetrating area of radiography. fi lm. The technique is revealed inside this tele radiation continuously. Radioactive sources should be kept in a secure, fi re þ DO use clear working signs and signals. called radiography and phone because they have Special containers made þ DO set up the controlled area and the necessary barriers. the processed fi lms are absorbed more radiation of dense metal shielding resistant and adequately shielded storage location þ DO confi rm the location of the source, or that X rays are called radiographs. than the surrounding plastic. are necessary to store, not being generated, by use of a survey meter. when not in use, and should move and manipulate these þ DO secure and store the source or X ray machine when sources. Due to their small be kept separate from other not in use. materials. The storage loca- size and manoeuvrability, Portable and mobile radiographic þ DO wear your personal dosimeter. sealed sources can be containers. ~ tion for X ray machines that used in confined spaces. are not in use is not required to be shielded. OTHER WORKERS Iridium-192 is a common radioactive source used þ DO observe the access restrictions, however remote it may in gamma radiography. -
Development of Chemical Dosimeters Development Of
SUDANSUDAN ACADEMYAGADEMY OFOF SCIENCES(SAS)SGIENGES(SAS) ATOMICATOMIC ENERGYEhTERGYRESEARCHESRESEARCHES COORDINATIONCOORDII\rATI ON COUNCILCOUNCIL - Development of Chemical Dosimeters A dissertation Submitted in a partial Fulfillment of the Requirement forfbr Diploma Degree in Nuclear Science (Chemistry) By FareedFadl Alla MersaniMergani SupervisorDr K.S.Adam MurchMarch 2006 J - - - CONTENTS Subject Page -I - DedicationDedication........ ... ... ... ... ... ... ... ... ... ... ... ... ... ... ... ... ... ... ... I Acknowledgement ... '" ... ... ... ... ... ... '" ... ... ... ... '" ... '" ....... .. 11II Abstract ... ... ... '" ... ... ... '" ... ... ... ... -..... ... ... ... ... ... ..... III -I Ch-lch-1 DosimetryDosimefry - 1-1t-l IntroductionLntroduction . 1I - 1-2t-2 Principle of Dosimetry '" '" . 2 1-3l-3 DosimetryDosimefiySystems . 3J 1-3-1l-3-l primary standard dosimeters '" . 4 - 1-3-2l-3-Z Reference standard dosimeters ... .. " . 4 1-3-3L-3-3 Transfer standard dosimeters ... ... '" . 4 1-3-4t-3-4 Routine dosimeters . 5 1-4I-4 Measurement of absorbed dose . 6 1-5l-5 Calibration of DosimetryDosimetrvsystemsvstem '" . 6 1-6l-6 Transit dose effects . 8 Ch-2ch-2 Requirements of chemical dosimeters 2-12-l Introduction ... ... ... .............................................. 111l 2-2 Developing of chemical dosimeters ... ... .. ....... ... .. ..... 12t2 2-3 Classification of Dosimetry methods.methods .......................... 14l4 2-4 RequirementsRequiremsnts of ideal chemical dosimeters ,. ... 15 2-5 Types of chemical system . -

The International Commission on Radiological Protection: Historical Overview
Topical report The International Commission on Radiological Protection: Historical overview The ICRP is revising its basic recommendations by Dr H. Smith Within a few weeks of Roentgen's discovery of gamma rays; 1.5 roentgen per working week for radia- X-rays, the potential of the technique for diagnosing tion, affecting only superficial tissues; and 0.03 roentgen fractures became apparent, but acute adverse effects per working week for neutrons. (such as hair loss, erythema, and dermatitis) made hospital personnel aware of the need to avoid over- Recommendations in the 1950s exposure. Similar undesirable acute effects were By then, it was accepted that the roentgen was reported shortly after the discovery of radium and its inappropriate as a measure of exposure. In 1953, the medical applications. Notwithstanding these observa- ICRU recommended that limits of exposure should be tions, protection of staff exposed to X-rays and gamma based on consideration of the energy absorbed in tissues rays from radium was poorly co-ordinated. and introduced the rad (radiation absorbed dose) as a The British X-ray and Radium Protection Committee unit of absorbed dose (that is, energy imparted by radia- and the American Roentgen Ray Society proposed tion to a unit mass of tissue). In 1954, the ICRP general radiation protection recommendations in the introduced the rem (roentgen equivalent man) as a unit early 1920s. In 1925, at the First International Congress of absorbed dose weighted for the way different types of of Radiology, the need for quantifying exposure was radiation distribute energy in tissue (called the dose recognized. As a result, in 1928 the roentgen was equivalent in 1966). -

MIRD Pamphlet No. 22 - Radiobiology and Dosimetry of Alpha- Particle Emitters for Targeted Radionuclide Therapy
Alpha-Particle Emitter Dosimetry MIRD Pamphlet No. 22 - Radiobiology and Dosimetry of Alpha- Particle Emitters for Targeted Radionuclide Therapy George Sgouros1, John C. Roeske2, Michael R. McDevitt3, Stig Palm4, Barry J. Allen5, Darrell R. Fisher6, A. Bertrand Brill7, Hong Song1, Roger W. Howell8, Gamal Akabani9 1Radiology and Radiological Science, Johns Hopkins University, Baltimore MD 2Radiation Oncology, Loyola University Medical Center, Maywood IL 3Medicine and Radiology, Memorial Sloan-Kettering Cancer Center, New York NY 4International Atomic Energy Agency, Vienna, Austria 5Centre for Experimental Radiation Oncology, St. George Cancer Centre, Kagarah, Australia 6Radioisotopes Program, Pacific Northwest National Laboratory, Richland WA 7Department of Radiology, Vanderbilt University, Nashville TN 8Division of Radiation Research, Department of Radiology, New Jersey Medical School, University of Medicine and Dentistry of New Jersey, Newark NJ 9Food and Drug Administration, Rockville MD In collaboration with the SNM MIRD Committee: Wesley E. Bolch, A Bertrand Brill, Darrell R. Fisher, Roger W. Howell, Ruby F. Meredith, George Sgouros (Chairman), Barry W. Wessels, Pat B. Zanzonico Correspondence and reprint requests to: George Sgouros, Ph.D. Department of Radiology and Radiological Science CRB II 4M61 / 1550 Orleans St Johns Hopkins University, School of Medicine Baltimore MD 21231 410 614 0116 (voice); 413 487-3753 (FAX) [email protected] (e-mail) - 1 - Alpha-Particle Emitter Dosimetry INDEX A B S T R A C T......................................................................................................................... -
Chapter 2 Radiation Safety Manual Revision 1 Principles of Radiation Safety 6/1/2018
The University of Georgia Chapter 2 Radiation Safety Manual Revision 1 Principles of Radiation Safety 6/1/2018 CHAPTER 2 PRINCIPLES OF RADIATION SAFETY 1.0 UNITS OF RADIATION DOSE 1.1 Historical Units In 1896, x-rays were discovered by Wilhelm Roentgen. The Roentgen is unit of measurement for the exposure of x-rays and gamma rays. It is defined as the electric charge freed by such radiation in a specified volume of air divided by the mass of that air. Radioactivity was discovered by Henri Becquerel. Radioactivity refers to the amount of radiation released when an element spontaneously emits energy as a result of the decay of its unstable atoms. The Becquerel is a unit used to measure radioactivity, and stands for 1 disintegration per second. The Curie is a unit of radioactivity equal to 3.7 X 1010 disintegrations per second and was first used, but being such a large unit was replaced by the Becquerel. The Curie is named for Pierre Curie, Marie Curie’s husband and co- discoverer of radium. After his accidental death, she continued their work. For some time, no one realized that radiation could cause harmful effects. It was recognized very soon that x-rays could be used in medical diagnosis, and early radiologists received large doses of radiation. Many of these radiologists later suffered severe injuries due to overexposure (radiation effects may appear years after exposure). The first unit of dose was the erythema dose. This was the amount of x-radiation which would barely cause reddening of the skin. It was not a very satisfactory unit of dose, but indicates the early recognition by some scientists that radiation exposure can be harmful and should be limited. -

Sievert Roofing Products Catalog
Heating tools for professionals Distributed by: BEST MATERIALS LLC Ph: 1-800-474-7570, 1-602-272-8128 Fax: 1-602-272-8014 Email: [email protected] www.bestmaterials.com Roofing Catalog Sievert Industries, Inc. Edition 9 Sievert Industries, Inc. In 1882, the Swedish inventor, Carl Richard Nyberg The Leader in Torch worked in his kitchen to design a revolutionary product, Technolog since1882 a vaporization torch for petrol. During the same year, he obtained a patent for his product which he called a “blow lamp”. This “blow lamp,” or torch, was distributed throughout the world with the help of the famous industrialist, Max Sievert. Carrying on Max Sievert’s work ethic, Sievert Industries, Inc. continually strives to be the leader in the North and South American roofing market since our entrance in 1996. Our goal is to provide our valued customers with quality service, competitive pricing, and the highest level of dependable roofing equipment available. Table of Contents Featured Products.. 7 Sievert Safety.. 8 - 9 Sievert Turboroofer Torch Kits. 10 Sievert Turboroofer Multi-Piece Torch Kits.. 11 Sievert Turboroofer Torch Kit Accessories. 12 Sievert Promatic Torches and Kits.. 13 Sievert Promatic Repair Kits. .. 14 Sievert Promatic Torch Kit Accessories . .15 Sievert Granule Embedders, Sievert Industrial Steel Roller and Sievert Quality Hand Irons . .16 Sievert ES Soldering Iron Kits. 17 Sievert SIK Premium Soldering Iron Kits.. 18 Sievert LSK Premium Basic Soldering Iron Kits.. .19 Sievert ES, SIK and LSK Soldering Iron Kit Accessories.. .20 Sievert Heavy Duty Electronic Hot Air Guns and Accessories. .21 Sievert TW 5000 Hot-Air Automatic Welding Machine and Accessories. -

What Are Health Risks from Ionising Radiation?
What are health risks from Ionising Radiation? It has been known for many years that large doses of ionising radiation, very every 100 persons exposed to a short-term dose of 1000 mSv (ie. if the much larger than background levels, can cause a measurable increase in normal incidence of fatal cancer were 25%, this dose would increase it to cancers and leukemias (‘cancer of the blood’) after some years delay. It must 30%).If doses greater than 1000 mSv occur over a long period they are also be assumed, because of experiments on plants and animals, that ionising less likely to have early health effects but they create a definite risk that radiation can also cause genetic mutations that affect future generations, cancer will develop many years later. although there has been no evidence of radiation-induced mutation in Higher accumulated doses of radiation might produce a cancer which humans. At very high levels, radiation can cause sickness and death within would only be observed several – up to twenty – years after the radiation weeks of exposure. exposure. This delay makes it impossible to say with any certainty which The degree of damage caused by radiation depends on many factors – of many possible agents were the cause of a particular cancer. In western dose, dose rate, type of radiation, the part of the body exposed, age and countries, about a quarter of people die from cancers, with smoking, health, for example. Embryos including the human fetus are particularly dietary factors, genetic factors and strong sunlight being among the sensitive to radiation damage. -

Radiation Glossary
Radiation Glossary Activity The rate of disintegration (transformation) or decay of radioactive material. The units of activity are Curie (Ci) and the Becquerel (Bq). Agreement State Any state with which the U.S. Nuclear Regulatory Commission has entered into an effective agreement under subsection 274b. of the Atomic Energy Act of 1954, as amended. Under the agreement, the state regulates the use of by-product, source, and small quantities of special nuclear material within said state. Airborne Radioactive Material Radioactive material dispersed in the air in the form of dusts, fumes, particulates, mists, vapors, or gases. ALARA Acronym for "As Low As Reasonably Achievable". Making every reasonable effort to maintain exposures to ionizing radiation as far below the dose limits as practical, consistent with the purpose for which the licensed activity is undertaken. It takes into account the state of technology, the economics of improvements in relation to state of technology, the economics of improvements in relation to benefits to the public health and safety, societal and socioeconomic considerations, and in relation to utilization of radioactive materials and licensed materials in the public interest. Alpha Particle A positively charged particle ejected spontaneously from the nuclei of some radioactive elements. It is identical to a helium nucleus, with a mass number of 4 and a charge of +2. Annual Limit on Intake (ALI) Annual intake of a given radionuclide by "Reference Man" which would result in either a committed effective dose equivalent of 5 rems or a committed dose equivalent of 50 rems to an organ or tissue. Attenuation The process by which radiation is reduced in intensity when passing through some material. -
External and Internal Dosimetry
Chapter 7 External and Internal Dosimetry H-117 – Introductory Health Physics Slide 1 Objectives ¾ Discuss factors influencing external and internal doses ¾ Define terms used in external dosimetry ¾ Discuss external dosimeters such as TLDs, film badges, OSL dosimeters, pocket chambers, and electronic dosimetry H-117 – Introductory Health Physics Slide 2 Objectives ¾ Define terms used in internal dosimetry ¾ Discuss dose units and limits ¾ Define the ALI, DAC and DAC-hr ¾ Discuss radiation signs and postings H-117 – Introductory Health Physics Slide 3 Objectives ¾ Discuss types of bioassays ¾ Describe internal dose measuring equipment and facilities ¾ Discuss principles of internal dose calculation and work sample problems H-117 – Introductory Health Physics Slide 4 External Dosimetry H-117 – Introductory Health Physics Slide 5 External Dosimetry Gamma, beta or neutron radiation emitted by radioactive material outside the body irradiates the skin, lens of the eye, extremities & the whole body (i.e. internal organs) H-117 – Introductory Health Physics Slide 6 External Dosimetry (cont.) ¾ Alpha particles cannot penetrate the dead layer of skin (0.007 cm) ¾ Beta particles are primarily a skin hazard. However, energetic betas can penetrate the lens of an eye (0.3 cm) and deeper tissue (1 cm) ¾ Beta sources can produce more penetrating radiation through bremsstrahlung ¾ Primary sources of external exposure are photons and neutrons ¾ External dose must be measured by means of appropriate dosimeters H-117 – Introductory Health Physics Slide 7