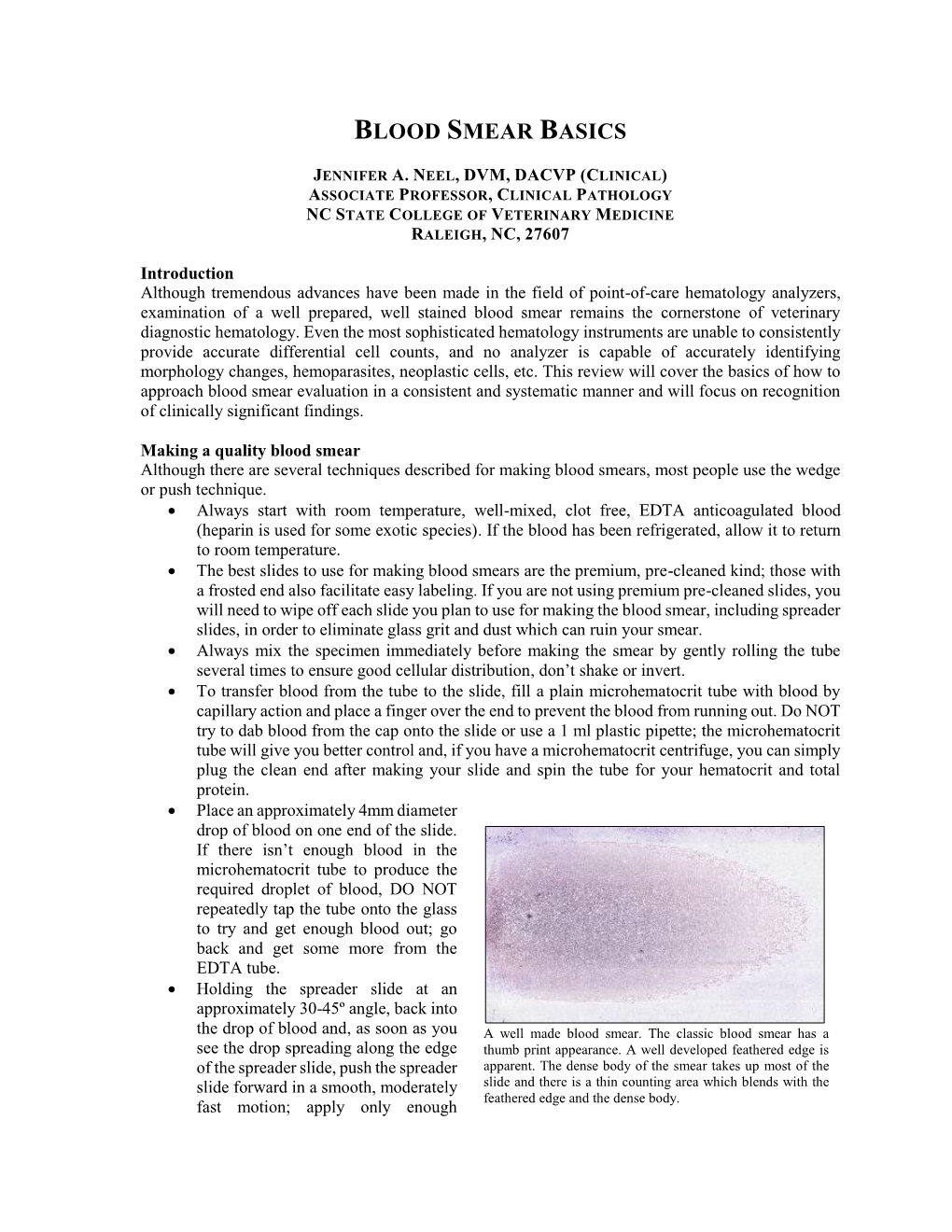
Blood Smear Basics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Markers of Carotid Atherosclerosis in Type 2 Diabetes Mellitus? Riya M Waghale, Rajashree Sanjay Khot, Prashant P Joshi Impact of Smoking and Nicotine Addiction
2020, Vol. 9, No. 2 ISSN 2450–7458 Platelet volume indices: markers of carotid atherosclerosis in type 2 diabetes mellitus? Riya M Waghale, Rajashree Sanjay Khot, Prashant P Joshi Impact of smoking and nicotine addiction on HbA1c levels and diabetic microvascular complication Hüseyin Akkuzulu, Cenk Aypak, Ayşe Özdemir, Süleyman Görpelioğlu Sugary beverages consumption and latent autoimmune diabetes in adults: systematic review and meta-analysis Ahmed Mahmoud El-Malky, Ramachandra G Naik, Azza A Elnouman The effect of low dose glargine U 300 on uncontrolled type 2 diabetes mellitus. An observational study in Indian patients Asis Mitra, Saswati Ray, Sushma Jayan Coffee in the diet and prevention of diabetes Regina Wierzejska Editor-in-Chief Scientific Board dr hab. n. med. Leszek Czupryniak, prof. nadzw. (Poland) prof. Antionio Ceriello (Spain) prof. dr hab. n. med. Edward Franek (Poland) Deputy Editor-in-Chief prof. dr hab. n. med. Władysław Grzeszczak (Poland) prof. dr hab. n. med. Wojciech Młynarski (Poland) prof. Martin Haluzík (Czech Republic) prof. dr hab. n. med. Krzysztof Strojek (Poland) prof. dr hab. n. med. Przemysława Jarosz-Chobot (Poland) prof. Nebojsa Lalic (Serbia and Montenegro) Editorial Board prof. Pierre Lefebvre (Belgium) prof. dr hab. n. med. Katarzyna Cypryk (Poland) prof. dr hab. n. med. Maciej Małecki (Poland) prof. Larisa Danilova (Belarus) prof. dr hab. n. med. Andrzej Milewicz (Poland) prof. dr hab. n. med. Janusz Gumprecht (Poland) prof. dr hab. n. med. Dariusz Moczulski (Poland) prof. dr hab. n. med. Krzysztof Narkiewicz (Poland) prof. dr hab. n. med. Irina Kowalska (Poland) dr Katherine Owen (United Kingdom) prof. dr hab. n. med. -
Mass Cytometric Functional Profiling of Acute Myeloid Leukemia Defines Cell-Cycle and Immunophenotypic Properties That Correlate with Known Responses to Therapy
Published OnlineFirst June 19, 2015; DOI: 10.1158/2159-8290.CD-15-0298 ReseaRch aRticle Mass Cytometric Functional Profiling of Acute Myeloid Leukemia Defines Cell-Cycle and Immunophenotypic Properties That Correlate with Known Responses to Therapy Gregory K. Behbehani1,2,3, Nikolay Samusik1, Zach B. Bjornson1, Wendy J. Fantl1,4, Bruno C. Medeiros2,3, and Garry P. Nolan1 Downloaded from cancerdiscovery.aacrjournals.org on September 25, 2021. © 2015 American Association for Cancer Research. Published OnlineFirst June 19, 2015; DOI: 10.1158/2159-8290.CD-15-0298 abstRact Acute myeloid leukemia (AML) is characterized by a high relapse rate that has been attributed to the quiescence of leukemia stem cells (LSC), which renders them resistant to chemotherapy. However, this hypothesis is largely supported by indirect evidence and fails to explain the large differences in relapse rates across AML subtypes. To address this, bone mar- row aspirates from 41 AML patients and five healthy donors were analyzed by high-dimensional mass cytometry. All patients displayed immunophenotypic and intracellular signaling abnormalities within CD34+CD38lo populations, and several karyotype- and genotype-specific surface marker patterns were identified. The immunophenotypic stem and early progenitor cell populations from patients with clinically favorable core-binding factor AML demonstrated a 5-fold higher fraction of cells in S-phase compared with other AML samples. Conversely, LSCs in less clinically favorable FLT3-ITD AML exhib- ited dramatic reductions in S-phase fraction. Mass cytometry also allowed direct observation of the in vivo effects of cytotoxic chemotherapy. SIGNIFICANCE: The mechanisms underlying differences in relapse rates across AML subtypes are poorly understood. -

Interpreting Your Child's Lab Results
www.ComplexChild.com Interpreting Your Child’s Lab Results When you get a list of labs back from your doctor or hospital, your eye is drawn immediately to the starred or highlighted results that came back abnormal. Knowing that any of your child’s results have come back abnormal can be disconcerting. Much of the time, however, there is no need to worry. But how do you know when abnormal results indicate a little problem, a big problem, or not a problem at all? Reference Ranges The first thing you need to do is look at the reference ranges that are given along with the results. Each lab has its own equipment that is calibrated uniquely, and results vary depending on the lab. While most tests have similar reference ranges from lab to lab, there are some, such as the test for Lipase, that use different testing systems with very different reference ranges. Results from one lab may not be equivalent to results at another lab. The Slightly High or Low Result In many cases, the abnormal result is ever so slightly high or low. Since reference ranges usually represent two standard deviations above or below the average mean value in healthy people, it is still normal for about five percent of the population to be ever so slightly higher or lower than the reference range. Keeping this in mind, a slightly low or high result is rarely concerning. Tests may also be slightly off due to illness, food or drink consumed, or many other factors. Many doctors will advise repeating the tests at a later time to see if the value has normalized, remains the same, or is trending upward or downward. -

Red Blood Cell Rheology in Sepsis K
M. Piagnerelli Red blood cell rheology in sepsis K. Zouaoui Boudjeltia M. Vanhaeverbeek J.-L. Vincent Abstract Changes in red blood cell membrane components such as sialic (RBC) function can contribute to acid, and an increase in others such alterations in microcirculatory blood as 2,3 diphosphoglycerate. Other flow and cellular dysoxia in sepsis. factors include interactions with Decreases in RBC and neutrophil white blood cells and their products deformability impair the passage of (reactive oxygen species), or the these cells through the microcircula- effects of temperature variations. tion. While the role of leukocytes Understanding the mechanisms of has been the focus of many studies altered RBC rheology in sepsis, and in sepsis, the role of erythrocyte the effects on blood flow and oxygen rheological alterations in this syn- transport, may lead to improved drome has only recently been inves- patient management and reductions tigated. RBC rheology can be influ- in morbidity and mortality. enced by many factors, including alterations in intracellular calcium Keywords Erythrocyte · and adenosine triphosphate (ATP) Deformability · Nitric oxide · concentrations, the effects of nitric Sialic acid · Multiple organ failure · oxide, a decrease in some RBC Oxygen transport Introduction ogy of microcirculatory alterations and, perhaps, the treatment of sepsis. Severe sepsis and septic shock are the commonest causes This review evaluates alterations occurring in RBC of death in intensive care units (ICUs), with associated rheology during sepsis and possible underlying mecha- mortality rates of 30–50% [1]. Sepsis is a complex nisms. The potential implications of blood transfusion pathophysiological process that involves both alterations and erythropoietin administration in sepsis will not be in the microcirculation and changes in the biochemical discussed. -

Music from a Darkened Room
DELTA GREEN-MUSIC FROM A DARKENED ROOM DENNIS DETWILLER Music from a Darkened Room A DELTA GREEN INVESTIGATION FOR 1 TO 4 AGENTS Wherein the Agents learn some threats are more tangible than others... BY DENNIS DETWILLER laces, like people, sometimes P go wrong. They turn off the The House on Spooner path and head into the shadows; Avenue becoming something other than Spooner Avenue is a quiet street normal. Black places filled with that can be set in any suburban BREAKDOWN OF INTEL blank rooms, closed doors and location in the United States. empty hallways lined with dust. 1206 Spooner Avenue is a small 1 THE HOUSE ON SPOONER AVENUE ! In these places your voice house, originally built in 1907, 2 THE AGENTS ARRIVE catches in your throat, the air and amended with additional 3 WHAT’S GOING ON AT 1206 SPOONER seems to hum and things hap- construction in the 1940’s. It’s not 4 TRAILS pen. People get hurt, objects van- pretty or ugly; it’s just plain. Few 4 1206 SPOONER — THE EXTERIOR ish. Bad feelings flow like the notice anything past the vibrant 4 INSIDE 1206 SPOONER loose tap in the bathroom and growth of ivy that scales the 4 THE COUNTY SEAT hate hangs in the air like old north side of the building. It is 8 SHUT DOORS, CLOSED SHADES paint. It smells of time and cir- wholly unremarkable in appear- 8 THE LUCKY FEW cumstance and something just a ance. But the neighbors are not 10 BREAK OUT THE BADGES little beyond the world. -

Educational Commentary – Blood Cell Id: Peripheral Blood Findings in a Case of Pelger Huët Anomaly
EDUCATIONAL COMMENTARY – BLOOD CELL ID: PERIPHERAL BLOOD FINDINGS IN A CASE OF PELGER HUËT ANOMALY Educational commentary is provided through our affiliation with the American Society for Clinical Pathology (ASCP). To obtain FREE CME/CMLE credits, click on Earn CE Credits under Continuing Education on the left side of the screen. To view the blood cell images in more detail, click on the sample identification numbers underlined in the paragraphs below. This will open a virtual image of the selected cell and the surrounding fields. If the image opens in the same window as the commentary, saving the commentary PDF and opening it outside your browser will allow you to switch between the commentary and the images more easily. Click on this link for the API ImageViewerTM Instructions. Learning Outcomes On completion of this exercise, the participant should be able to • discuss the morphologic features of normal peripheral blood leukocytes; • describe characteristic morphologic findings in Pelger-Huët cells; and • differentiate Pelger-Huët cells from other neutrophils in a peripheral blood smear. Case History: A 30 year old female had a routine CBC performed as part of a physical examination. Her CBC results are as follows: WBC=5.9 x 109/L, RBC=4.53 x 1012/L, Hgb=13.6 g/dL, Hct=40%, MCV=88.3 fL, MCH=29.7 pg, MCHC=32.9 g/dL, Platelet=184 x 109/L. Introduction The images presented in this testing event represent normal white blood cells as well as several types of neutrophils that may be seen in the peripheral blood when a patient has the Pelger-Huët anomaly. -

The Catchiest Disease “Hesitation Marks” Embodies a Ruined Man Many a Personal Downfall in This Album by Max Robison Contributing Writer Especially
Tuesday, Features Sept. 10, 2013 11 “Get to Know a Retriever” Meet Arash Fallah, a student driven to succeed at UMBC have been mentoring me club wrestling team but I would really like to see I really look up to their the team be elevated to a andhumility, I’ve learned grace, aclass lot from. and formal collegiate level. Beverage choice that’s wisdom.is extremely Farrah intelligent,Daham is indicative of your onetrustworthy, of my role models.nuanced She personality? characteristics I admire in anda person. beautiful. Those are Pepsi,Keep Calmit’s sweet and and_________? dark. What is your favorite COURTESY ARASH FALLAH part about UMBC? RelaxHow has UMBC helped Arash Fallah rides a carousel at Whatever you want to you achieve success? Pentagon mall. With little exception, there importance of failure BY DAVID POZNANSKY doare atfew UMBC, obstacles you keepingcan do. It’s taught me the Contributing Writer you from pursuing your understanding that few passions. andadvantages success. comeAs well from as Name, Major, Year? taking a position of conceit. Sports team you’d be most excited to see play a measured impact by Arash Fallah, History and live? I’veapplying learned the lessonshow to of make tact. PoliticalFrom? Science, 2015 Potomac, Maryland challenge myself by taking LosWhat Angeles sport Lakers or activity It’s also encouraged me to Do you have any should UMBC compete in than merely coasting role models? What on a collegiate level? difficultthrough college.courses rather characteristics of theirs do you admire? have such an outstanding [email protected] I think it’s great that we There are two people who The catchiest disease “Hesitation Marks” embodies a ruined man many a personal downfall in this album BY MAX ROBISON Contributing Writer especially. -

Hemolytic Disease of the Newborn
Intensive Care Nursery House Staff Manual Hemolytic Disease of the Newborn INTRODUCTION and DEFINITION: Hemolytic Disease of the Newborn (HDN), also known as erythroblastosis fetalis, isoimmunization, or blood group incompatibility, occurs when fetal red blood cells (RBCs), which possess an antigen that the mother lacks, cross the placenta into the maternal circulation, where they stimulate antibody production. The antibodies return to the fetal circulation and result in RBC destruction. DIFFERENTIAL DIAGNOSIS of hemolytic anemia in a newborn infant: -Isoimmunization -RBC enzyme disorders (e.g., G6PD, pyruvate kinase deficiency) -Hemoglobin synthesis disorders (e.g., alpha-thalassemias) -RBC membrane abnormalities (e.g., hereditary spherocytosis, elliptocytosis) -Hemangiomas (Kasabach Merritt syndrome) -Acquired conditions, such as sepsis, infections with TORCH or Parvovirus B19 (anemia due to RBC aplasia) and hemolysis secondary to drugs. ISOIMMUNIZATION A. Rh disease (Rh = Rhesus factor) (1) Genetics: Rh positive (+) denotes presence of D antigen. The number of antigenic sites on RBCs varies with genotype. Prevalence of genotype varies with the population. Rh negative (d/d) individuals comprise 15% of Caucasians, 5.5% of African Americans, and <1% of Asians. A sensitized Rh negative mother produces anti-Rh IgG antibodies that cross the placenta. Risk factors for antibody production include 2nd (or later) pregnancies*, maternal toxemia, paternal zygosity (D/D rather than D/d), feto-maternal compatibility in ABO system and antigen load. (2) Clinical presentation of HDN varies from mild jaundice and anemia to hydrops fetalis (with ascites, pleural and pericardial effusions). Because the placenta clears bilirubin, the chief risk to the fetus is anemia. Extramedullary hematopoiesis (due to anemia) results in hepatosplenomegaly. -

Correlation of Blood Culture and Band Cell Ratio in Neonatal Septicaemia
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 13, Issue 3 Ver. VI. (Mar. 2014), PP 55-58 www.iosrjournals.org Correlation of blood culture and band cell ratio in neonatal septicaemia. Nautiyal S1., *Kataria V. K1., Pahuja V. K1., Jauhari S1., Roy R. C.,1 Aggarwal B.2 1Department of Microbiology, SGRRIM&HS and SMIH, Dehradun, Uttarakhand, India. 2Department of Paediatrics, SGRRIM&HS and SMIH, Dehradun, Uttarakhand, India. Abstract: Background: Neonatal sepsis is a clinical syndrome characterized by signs and symptoms of infection with or without accompanying bacteraemia in the first month of life. Incidence differs among hospitals depending on variety of factors. Blood culture is considered gold standard for the diagnosis, but does not give a rapid result. Hence, there is a need to look for a surrogate marker for diagnosing neonatal septicaemia. Material & Methods: 335 neonates were studied for clinically suspected septicaemia over a period of one year. Blood was cultured and organism identified biochemically. Parameters of subjects like EOS, LOS and Band cell counts were recorded. Results analysed statistically. Results: Male preponderance was observed. Majority of the cases had a normal vaginal delivery. 47.46% cases had early onset septicaemia. Meconium stained liquor was the predominant risk factor .Culture positivity was found to be 32.24% and 87.96% of them also had band cells percentage ranging from 0 to >25. Conclusion: Band cell count can be used as a surrogate marker for neonatal septicaemia. An upsurge of Candida species as a causative agent in Neonatal septicaemia has been observed. -

Section 8: Hematology CHAPTER 47: ANEMIA
Section 8: Hematology CHAPTER 47: ANEMIA Q.1. A 56-year-old man presents with symptoms of severe dyspnea on exertion and fatigue. His laboratory values are as follows: Hemoglobin 6.0 g/dL (normal: 12–15 g/dL) Hematocrit 18% (normal: 36%–46%) RBC count 2 million/L (normal: 4–5.2 million/L) Reticulocyte count 3% (normal: 0.5%–1.5%) Which of the following caused this man’s anemia? A. Decreased red cell production B. Increased red cell destruction C. Acute blood loss (hemorrhage) D. There is insufficient information to make a determination Answer: A. This man presents with anemia and an elevated reticulocyte count which seems to suggest a hemolytic process. His reticulocyte count, however, has not been corrected for the degree of anemia he displays. This can be done by calculating his corrected reticulocyte count ([3% × (18%/45%)] = 1.2%), which is less than 2 and thus suggestive of a hypoproliferative process (decreased red cell production). Q.2. A 25-year-old man with pancytopenia undergoes bone marrow aspiration and biopsy, which reveals profound hypocellularity and virtual absence of hematopoietic cells. Cytogenetic analysis of the bone marrow does not reveal any abnormalities. Despite red blood cell and platelet transfusions, his pancytopenia worsens. Histocompatibility testing of his only sister fails to reveal a match. What would be the most appropriate course of therapy? A. Antithymocyte globulin, cyclosporine, and prednisone B. Prednisone alone C. Supportive therapy with chronic blood and platelet transfusions only D. Methotrexate and prednisone E. Bone marrow transplant Answer: A. Although supportive care with transfusions is necessary for treating this patient with aplastic anemia, most cases are not self-limited. -

Evaluation of Anemia Survey (NHANES III) Data- 9 10-28% of Patients Over 65 Years Are Anemic Mark Wurster, M.D., F.A.C.P
Anemia - Definition • National Health and Nutrition Examination Evaluation of Anemia Survey (NHANES III) data- 9 10-28% of patients over 65 years are anemic Mark Wurster, M.D., F.A.C.P. 9 One third of these are due to iron, folate, B12 The Ohio State University deficiency alone or in combination 9 One third are due to renal disease, or other chronic inflammatory response 9 One third are due to various primary marrow disorders, malignancies or other disorders Anemia Anemia - Definition Classification Schemes • A simplified approach to anemia, • Most common hematologic disorder emphasizing information already included • Decrease from normal levels of Hgb, Hct, RBC: in the CBC: 9 FlFemales – MHb14/dlMean Hgb = 14 g/dl; -2SD = 12 g /dl • Mean Cellular Volume (MCV) 9 Males – Mean Hgb = 15.5 g/dl; -2SD = 13.5 g/dl • Red Cell Distribution Width (RDW) • Caveat – Anemia is a syndrome, not a disease. • Retic count An abnormal Hgb or Hct should ALWAYS be investigated if confirmed on repeat testing. 1 Anemia Anemia Classification Schemes Classification Schemes • Mean Cellular Volume (MCV) • Red blood cell Distribution Width (RDW) • Decreased MCV (microcytic); < 80 fL 9 A numerical expression of • Normal MCV (normocytic); 80 – 99 fL anisocytosis, or variation in RBC size • Increased MCV (macrocytic); > 100 fL Anemia Anemia Classification Schemes Classification Schemes • Red blood cell Distribution Width (RDW) 9 Normal RDW - representing a uniform population • Red blood cell Distribution Width (RDW) of RBCs with respect to size (actually the standard deviation of red blood cell volume divided by the mean volume) 9 Normal; < or = to app. -

Canine Immune-Mediated Hemolytic Anemia – Brief Review
TRADITION AND MODERNITY IN VETERINARY MEDICINE, 2018, vol. 3, No 1(4): 59–64 CANINE IMMUNE-MEDIATED HEMOLYTIC ANEMIA – BRIEF REVIEW Iliyan Manev1, Victoria Marincheva2 1University of Forestry, Faculty of Veterinary Medicine, Sofia, Bulgaria 2Animal Rescue, Sofia, Bulgaria E-mail: [email protected] ABSTRACT Immune-mediated hemolytic anemia (IMHA) is a common autoimmune disorder in dogs. It affects both sexes but occurs more often in female, middle-aged animals. IMHA can be idiopathic (primary) or secondary to infectious, neoplastic and autoimmune disorders. There is an acute regenerative anemia with accompanying hypoxia. Destruction of erythrocytes can be intravascular (as a result of complement system activation) or extravascular (removal of antibody-coated red blood cells by the macrophages in the liver and spleen). Diag- nosis is based on the presence of anemia, in vitro autoagglutination, positive direct antiglobulin test (Coomb`s test), detection of spherocytes. It is crucial to exclude possible secondary causes. The treatment protocol aims to cease cell destruction by high doses of corticosteroids, aggressive supportive care and long-term application of immunosuppressive drug combinations. Still lethality is high because of complications (pulmonary throm- boembolism, DIC), medication resistance, relapses. Key words: immune-mediated, anemia, canine, hemolysis, immunosuppressive drugs. Immune-mediated hemolytic anemia is one of the commonly diagnosed canine autoimmune diseases and a model of acute and clinically relevant anemia. Impaired