Understanding Your Blood Test Lab Results
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Markers of Carotid Atherosclerosis in Type 2 Diabetes Mellitus? Riya M Waghale, Rajashree Sanjay Khot, Prashant P Joshi Impact of Smoking and Nicotine Addiction
2020, Vol. 9, No. 2 ISSN 2450–7458 Platelet volume indices: markers of carotid atherosclerosis in type 2 diabetes mellitus? Riya M Waghale, Rajashree Sanjay Khot, Prashant P Joshi Impact of smoking and nicotine addiction on HbA1c levels and diabetic microvascular complication Hüseyin Akkuzulu, Cenk Aypak, Ayşe Özdemir, Süleyman Görpelioğlu Sugary beverages consumption and latent autoimmune diabetes in adults: systematic review and meta-analysis Ahmed Mahmoud El-Malky, Ramachandra G Naik, Azza A Elnouman The effect of low dose glargine U 300 on uncontrolled type 2 diabetes mellitus. An observational study in Indian patients Asis Mitra, Saswati Ray, Sushma Jayan Coffee in the diet and prevention of diabetes Regina Wierzejska Editor-in-Chief Scientific Board dr hab. n. med. Leszek Czupryniak, prof. nadzw. (Poland) prof. Antionio Ceriello (Spain) prof. dr hab. n. med. Edward Franek (Poland) Deputy Editor-in-Chief prof. dr hab. n. med. Władysław Grzeszczak (Poland) prof. dr hab. n. med. Wojciech Młynarski (Poland) prof. Martin Haluzík (Czech Republic) prof. dr hab. n. med. Krzysztof Strojek (Poland) prof. dr hab. n. med. Przemysława Jarosz-Chobot (Poland) prof. Nebojsa Lalic (Serbia and Montenegro) Editorial Board prof. Pierre Lefebvre (Belgium) prof. dr hab. n. med. Katarzyna Cypryk (Poland) prof. dr hab. n. med. Maciej Małecki (Poland) prof. Larisa Danilova (Belarus) prof. dr hab. n. med. Andrzej Milewicz (Poland) prof. dr hab. n. med. Janusz Gumprecht (Poland) prof. dr hab. n. med. Dariusz Moczulski (Poland) prof. dr hab. n. med. Krzysztof Narkiewicz (Poland) prof. dr hab. n. med. Irina Kowalska (Poland) dr Katherine Owen (United Kingdom) prof. dr hab. n. med. -

Interpreting Your Child's Lab Results
www.ComplexChild.com Interpreting Your Child’s Lab Results When you get a list of labs back from your doctor or hospital, your eye is drawn immediately to the starred or highlighted results that came back abnormal. Knowing that any of your child’s results have come back abnormal can be disconcerting. Much of the time, however, there is no need to worry. But how do you know when abnormal results indicate a little problem, a big problem, or not a problem at all? Reference Ranges The first thing you need to do is look at the reference ranges that are given along with the results. Each lab has its own equipment that is calibrated uniquely, and results vary depending on the lab. While most tests have similar reference ranges from lab to lab, there are some, such as the test for Lipase, that use different testing systems with very different reference ranges. Results from one lab may not be equivalent to results at another lab. The Slightly High or Low Result In many cases, the abnormal result is ever so slightly high or low. Since reference ranges usually represent two standard deviations above or below the average mean value in healthy people, it is still normal for about five percent of the population to be ever so slightly higher or lower than the reference range. Keeping this in mind, a slightly low or high result is rarely concerning. Tests may also be slightly off due to illness, food or drink consumed, or many other factors. Many doctors will advise repeating the tests at a later time to see if the value has normalized, remains the same, or is trending upward or downward. -
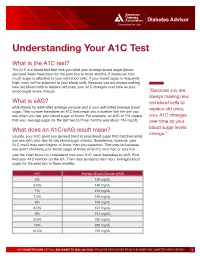
Understanding Your A1C Test
Diabetes Advisor Understanding Your A1C Test What is the A1C test? The A1C is a blood test that tells you what your average blood sugar (blood glucose) levels have been for the past two to three months. It measures how much sugar is attached to your red blood cells. If your blood sugar is frequently high, more will be attached to your blood cells. Because you are always making new red blood cells to replace old ones, your A1C changes over time as your blood sugar levels change. “Because you are always making new What is eAG? red blood cells to eAG stands for estimated average glucose and is your estimated average blood replace old ones, sugar. This number translates an A1C test result into a number like the one you see when you test your blood sugar at home. For example, an A1C of 7% means your A1C changes that your average sugar for the last two to three months was about 154 mg/dL. over time as your What does an A1C/eAG result mean? blood sugar levels change.” Usually, your A1C gives you general trend in your blood sugar that matches what you see with your day-to-day blood sugar checks. Sometimes, however, your A1C result may seem higher or lower than you expected. That may be because you aren’t checking your blood sugar at times when it’s very high or very low. Use the chart below to understand how your A1C result translates to eAG. First find your A1C number on the left. -

Quantitation of Relative Mobilities of Serum Transferrin in Quarter Horses and Thoroughbreds Using Crossed Immunoelectrophoresis
QUANTITATION OF RELATIVE MOBILITIES OF SERUM TRANSFERRIN IN QUARTER HORSES AND THOROUGHBREDS USING CROSSED IMMUNOELECTROPHORESIS BY RUTH GREER KAGEN II Bachelor of Science in Biology East Central Oklahoma State University Ada. Oklahoma 1982 Submitted to the Faculty of the Graduate College of the Oklahoma State University in partial fulfillment of requirements for the degree of MASTERS OF SCIENCE December. 1985 4 ' ;_ '" SERUM TRANSFERRIN IN QUARTER HORSES AND THOROUGHBREDS USING CROSSED IMMUNOELECTROPHORESIS Thesis Approved ii 1236431 ~ ACKNOWLEDGEMENTS The author wishes to express sincere gratitude to Dr. T. E. Staley for serving as the principle advisor and for providing the facilities and financial support necessary to carry out this work. I am most in debted to Dr. Staley for his continued faith in my work. his constant support and patient advice. and for his attentive and meticulous instruc tion as well as superb organization--all without which this study would not have been possible. I also wish to thank the members of the committee: Dr. C. L. Ownby and Dr. L. G. Stratton. I wish to extend my sincere thanks to Dr. C. L. Ownby for her continued interest in my career and her invaluable advice. both which greatly assisted me in the endeavors to carry out this work. I am very grateful for all the time which Dr. Ownby has afforded me and for her objective and sincere counsel. I am most appreciative of Dr. L. G. Stratton's interest in this project. Through his generous support and concern. we were provided with Pxcellent facilities in which to carry out this work and we were also provided with access to the animals needed for this project. -

Wilson Disease
Wilson Disease What is Wilson disease? Wilson disease is a hereditary disease in which excessive amounts of copper accumulate in the body, mainly in the liver. The disease affects approximately one in every 30,000 Canadians. Small amounts of copper are essential to good health. One of the liver’s jobs is to maintain the balance of copper in the body. The liver is also the main organ to store copper. In Wilson disease, when its storage capacity is full, copper is released into the blood stream. It then accumulates in various organs such as the brain and the cornea of the eye. This copper overload damages these organs. Left untreated, Wilson disease can be fatal. What causes the disease? Wilson disease is inherited. In order to have the disease, a person must get two defective genes, one from each parent. The liver begins to retain copper at birth and it may take years before symptoms manifest themselves. Having only one defective gene does not lead to Wilson disease. What are the symptoms of Wilson disease? Wilson disease is sometimes difficult to diagnose. Affected individuals may have no symptoms for years. When symptoms develop, they can be subtle. Sometimes symptoms of Wilson disease resemble hepatitis. Alternatively, some individuals have an enlarged liver and spleen and liver test abnormalities. Copper accumulation in the brain can present itself in two ways: (1) as physical symptoms such as slurred speech, failing voice, drooling, tremors or difficulty in swallowing or (2) as psychiatric disorders such as depression, manic behaviour or suicidal impulses. Very rarely, Wilson disease may cause the liver to fail. -

Serological (Antibody) Testing for Covid-19
SEROLOGICAL (ANTIBODY) TESTING FOR COVID-19 Serological tests detect antibodies in the blood People in the early stages of COVID-19 might generated as part of the immune response test antibody negative despite being highly to a specific infection, such as infection with infectious. Additionally, some tests might give a SARS-CoV-2, the virus that causes COVID-19. false positive result because of past or present Antibody tests are different from tests such as infection with other types of coronaviruses. polymerase chain reaction (PCR) and antigen False positive results are also more likely tests which detect the SARS-CoV-2 virus. when the percentage of the population with Many new serological tests for COVID-19 have the disease is low. The Idaho Division of Public been developed and have an emergency use Health discourages persons who have a positive authorization (EUA) from the U.S. Food and serology test from relaxing the precautions such Drug Administration (FDA). Only antibody tests as social distancing that are recommended for that have an FDA EUA should be used. The all Idahoans to prevent spread of coronavirus, Idaho Division of Public Health discourages and strongly discourages employers form the use of unauthorized serology-based assays relaxing the employee protections for an for diagnosis of COVID-19 or determining if employee solely based upon a positive serology someone is currently infected or had a prior test. infection. The immune response to SARS-CoV-2 (the Serological tests are not recommended for virus that causes COVID-19) infection is not COVID-19 diagnosis in most situations because well understood. -
Effect of Thyroid Hormones on Kidney Function in Patients After
www.nature.com/scientificreports OPEN Efect of Thyroid Hormones on Kidney Function in Patients after Kidney Transplantation Benjamin Schairer1, Viktoria Jungreithmayr2, Mario Schuster2, Thomas Reiter 1, Harald Herkner3, Alois Gessl4, Gürkan Sengölge1* & Wolfgang Winnicki 1 Elevated levels of thyroid-stimulating-hormone (TSH) are associated with reduced glomerular fltration rate (GFR) and increased risk of developing chronic kidney disease even in euthyroid patients. Thyroid hormone replacement therapy has been shown to delay progression to end-stage renal disease in sub-clinically hypothyroid patients with renal insufciency. However, such associations after kidney transplantation were never investigated. In this study the association of thyroid hormones and estimated GFR (eGFR) in euthyroid patients after kidney transplantation was analyzed. In total 398 kidney transplant recipients were assessed retrospectively and association between thyroid and kidney function parameters at and between defned time points, 12 and 24 months after transplantation, was studied. A signifcant inverse association was shown for TSH changes and eGFR over time between months 12 and 24 post transplantation. For each increase of TSH by 1 µIU/mL, eGFR decreased by 1.34 mL/min [95% CI, −2.51 to −0.16; p = 0.03], corresponding to 2.2% eGFR decline, within 12 months. At selected time points 12 and 24 months post transplantation, however, TSH was not associated with eGFR. In conclusion, an increase in TSH between 12 and 24 months after kidney transplantation leads to a signifcant decrease in eGFR, which strengthens the concept of a kidney- thyroid-axis. Interactions between thyroid hormones and kidney function have been suggested in previous studies. -
Jaundice Protocol
fighting childhood liver disease Jaundice Protocol Early identification and referral of liver disease in infants fighting childhood liver disease 36 Great Charles Street Birmingham B3 3JY Telephone: 0121 212 3839 yellowalert.org childliverdisease.org [email protected] Registered charity number 1067331 (England & Wales); SC044387 (Scotland) The following organisations endorse the Yellow Alert Campaign and are listed in alphabetical order. 23957 CLDF Jaundice Protocol.indd 1 03/08/2015 18:25:24 23957 3 August 2015 6:25 PM Proof 1 1 INTRODUCTION This protocol forms part of Children’s Liver Disease Foundation’s (CLDF) Yellow Alert Campaign and is written to provide general guidelines on the early identification of liver disease in infants and their referral, where appropriate. Materials available in CLDF’s Yellow Alert Campaign CLDF provides the following materials as part of this campaign: • Yellow Alert Jaundice Protocol for community healthcare professionals • Yellow Alert stool colour book mark for quick and easy reference • Parents’ leaflet entitled “Jaundice in the new born baby”. CLDF can provide multiple copies to accompany an antenatal programme or for display in clinics • Yellow Alert poster highlighting the Yellow Alert message and also showing the stool chart 2 GENERAL AWARENESS AND TRAINING The National Institute of Health and Clinical Excellence (NICE) has published a clinical guideline on neonatal jaundice which provides guidance on the recognition, assessment and treatment of neonatal jaundice in babies from birth to 28 days. Neonatal Jaundice Clinical Guideline guidance.nice.org.uk cg98 For more information go to nice.org.uk/cg98 • Jaundice Community healthcare professionals should be aware that there are many causes for jaundice in infants and know how to tell them apart: • Physiological jaundice • Breast milk jaundice • Jaundice caused by liver disease • Jaundice from other causes, e.g. -

K392-100 Total Iron-Binding Capacity (TIBC) and Serum Iron Assay Kit (Colorimetric)
FOR RESEARCH USE ONLY! Total Iron-Binding Capacity (TIBC) and Serum Iron Assay Kit (Colorimetric) rev 08/19 (Catalog # K392-100; 100 assays; Store at -20°C) I. Introduction: BioVision’s TIBC and Serum Iron Assay Kit measures both Total iron-binding capacity (TIBC) and Serum iron. Those values indicate the requisite iron for transferrin saturation and Serum Iron respectively. In humans, Transferrin is a blood protein that binds and transports iron throughout the body. Iron bound to transferrin and not bound are reflected in the following: 1) Total Iron Binding Capacity, 2) Unbound Iron, 3) Transferrin Saturation Bound Iron, and 4) Free Iron. Those measurements can be used for to detect and monito transferrin saturation and also iron-deficiency anemia and chronic inflammatory diseases. Part A: TIBC Part B: Serum Iron 1 1 2 2 3 3 4 II. Application: Determination of TIBC, Unbound Iron, Transferrin Saturation, Serum Iron III. Sample Type: Serum or plasma. Serum-off-the clot is preferable to normal serum. IV. Kit Contents: Components K392-100 Cap Code Part Number TIBC Assay Buffer 25 ml WM K392-100-1 Iron Solution 100 µl Blue K392-100-2 TIBC Detector 2 x 1.5 ml Brown K392-100-3 TIBC Developer 5 ml NM K392-100-4 Iron Standard (100 mM) 100 µl Yellow K392-100-5 V. User Supplied Reagents and Equipment: • 96-well plate clear plate with flat bottom • Microplate reader capable of absorbance reading VI. Storage Conditions and Reagent Preparation: Store kit at -20°C, protected from light. Briefly centrifuge small vials prior to opening. -

Lactose Tolerance Blood Test
Lactose tolerance blood test Lactose tolerance tests measure the ability of your intestines to break down lactose, a type of sugar found in milk and other dairy products. How the test is performed The lactose tolerance blood test looks for glucose in your blood. Your body creates glucose when lactose breaks down. For this test, several blood samples will be taken before and after you drink the lactose solution described above. For information on how a blood sample is obtained, see venipuncture. How to prepare for the test You should not eat for 8 hours before the test. Avoid strenuous exercise for 8 hours before the test. How the test will feel There should not be any pain or discomfort when giving a breath sample. When the needle is inserted to draw blood, some people feel moderate pain, while others feel only a prick or stinging sensation. Afterward, there may be some throbbing. Why the test is performed Your doctor may order these tests if you have signs of lactose intolerance. Normal Values The breath test is considered normal if the increase in hydrogen is less than 12 parts per million over your fasting (pre-test) level. The blood test is considered normal if your glucose level rises more than 30 mg/dL within 2 hours of drinking the lactose solution. A rise of 20-30 mg/dL is inconclusive. Note: Normal value ranges may vary slightly among different laboratories. Talk to your doctor about the meaning of your specific test results. The examples above show the common measurements for results for these tests. -

Rotational Thromboelastometry Predicts Care Level in Covid-19
medRxiv preprint doi: https://doi.org/10.1101/2020.06.11.20128710; this version posted June 12, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-NC-ND 4.0 International license . Rotational Thromboelastometry predicts care level in Covid-19 1 2 3 4 Lou M. Almskog, MD ; Agneta Wikman, MD, PhD ; Jonas Svensson, MD ; 1 5 6 2 Michael Wanecek, MD, PhD ; Matteo Bottai, PhD ; Jan van der Linden, MD, PhD 7 8 9 ; Anna Ågren, MD, PhD . 1 Department of Anaesthesiology and Intensive Care, Capio St Göran’s Hospital, Stockholm, Sweden 2 Department of Molecular Medicine and Surgery, Karolinska Institutet, Stockholm, Sweden 3 Department of Clinical Immunology and Transfusion Medicine, Karolinska University Hospital and Department of CLINTEC, Karolinska Institutet, Stockholm, Sweden 4 Department of Clinical Neuroscience, Karolinska Institutet, Stockholm, Sweden 5 Department of Physiology and Pharmacology, Karolinska Institutet, Stockholm, Sweden 6 Unit of Biostatistics, Institute of Environmental Medicine, Karolinska Institutet, Stockholm, Sweden 7 Perioperative Medicine and Intensive Care, Karolinska University Hospital, Stockholm, Sweden 8 Coagulation Unit, Division of Hematology, Karolinska University Hospital, Stockholm, Sweden 9 Department of Clinical Sciences, Danderyd Hospital, Stockholm, Sweden NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice. medRxiv preprint doi: https://doi.org/10.1101/2020.06.11.20128710; this version posted June 12, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. -

Wellness Labs Explanation of Results
WELLNESS LABS EXPLANATION OF RESULTS BASIC METABOLIC PANEL BUN – Blood Urea Nitrogen (BUN) is a waste product of protein breakdown and is produced when excess protein in your body is broken down and used for energy. BUN levels greater than 50 mg/dL generally means that the kidneys are not functioning normally. Abnormally low BUN levels can be seen with malnutrition and liver failure. Creatinine – a waste product of normal muscle activity. High creatinine levels are most commonly seen in kidney failure and can also been seen with hyperthyroidism, conditions of overgrowth of the body, rhabdomyolysis, and early muscular dystrophy. Low creatinine levels can indicate low muscle mass associated with malnutrition and late-stage muscular dystrophy. Glucose – a simple sugar that serves as the main source of energy in the body. High glucose levels (hyperglycemia) is usually associated with prediabetes and can also occur with severe stress on the body such as surgery or events like stroke or trauma. High levels can also be seen with overactive thyroid, pancreatitis, or pancreatic cancer. Low glucose levels can occur with underactive thyroid and rare insulin- secreting tumors. Electrolytes – Sodium, Calcium, Potassium, Chloride, and Carbon Dioxide are all included in this category. Sodium – high levels of sodium can be seen with dehydration, excessive thirst, and urination due to abnormally low levels of antidiuretic hormone (diabetes insipidus) as well as with excessive levels of cortisol in the body (Cushing syndrome). Low levels of sodium can be seen with congestive heart failure, cirrhosis of the liver, kidney failure, and the syndrome of inappropriate antidiuretic hormone (SIADH).