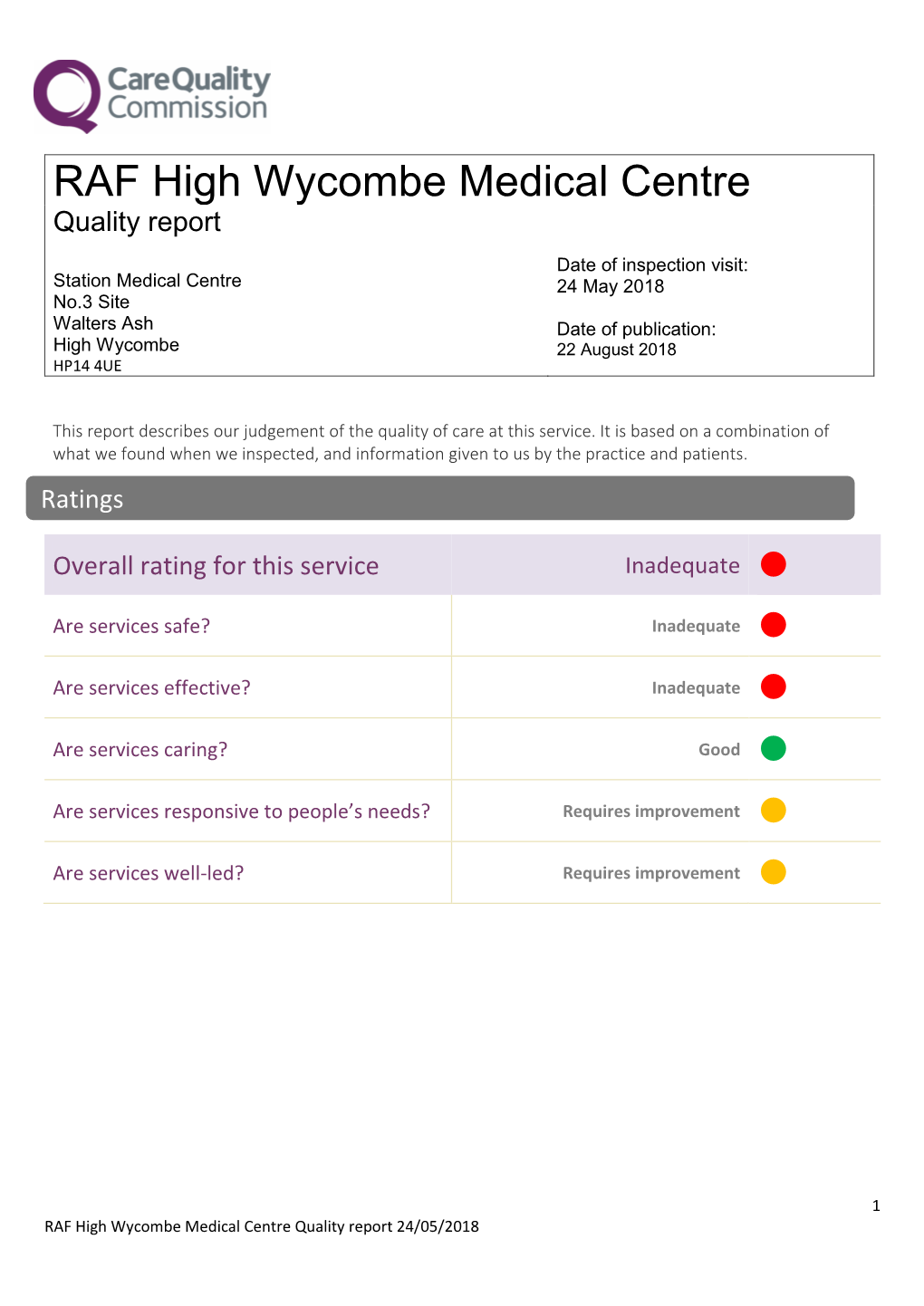
RAF High Wycombe Medical Centre
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Technical Details of the Elliott 152 and 153
Appendix 1 Technical Details of the Elliott 152 and 153 Introduction The Elliott 152 computer was part of the Admiralty’s MRS5 (medium range system 5) naval gunnery project, described in Chap. 2. The Elliott 153 computer, also known as the D/F (direction-finding) computer, was built for GCHQ and the Admiralty as described in Chap. 3. The information in this appendix is intended to supplement the overall descriptions of the machines as given in Chaps. 2 and 3. A1.1 The Elliott 152 Work on the MRS5 contract at Borehamwood began in October 1946 and was essen- tially finished in 1950. Novel target-tracking radar was at the heart of the project, the radar being synchronized to the computer’s clock. In his enthusiasm for perfecting the radar technology, John Coales seems to have spent little time on what we would now call an overall systems design. When Harry Carpenter joined the staff of the Computing Division at Borehamwood on 1 January 1949, he recalls that nobody had yet defined the way in which the control program, running on the 152 computer, would interface with guns and radar. Furthermore, nobody yet appeared to be working on the computational algorithms necessary for three-dimensional trajectory predic- tion. As for the guns that the MRS5 system was intended to control, not even the basic ballistics parameters seemed to be known with any accuracy at Borehamwood [1, 2]. A1.1.1 Communication and Data-Rate The physical separation, between radar in the Borehamwood car park and digital computer in the laboratory, necessitated an interconnecting cable of about 150 m in length. -
Voices from an Old Warrior Why KC-135 Safety Matters
Voices from an Old Warrior Why KC-135 Safety Matters Foreword by General Paul Selva GALLEON’S LAP PUBLISHING ND 2 EDITION, FIRST PRINTING i Hoctor, Christopher J. B. 1961- Voices from an Old Warrior: Why KC-135 Safety Matters Includes bibliographic references. 1. Military art and science--safety, history 2. Military history 3. Aviation--history 2nd Edition – First Printing January 2014 1st Edition (digital only) December 2013 Printed on the ©Espresso Book Machine, Mizzou Bookstore, Mizzou Publishing, University of Missouri, 911 E. Rollins Columbia, MO 65211, http://www.themizzoustore.com/t-Mizzou-Media-About.aspx Copyright MMXIII Galleon's Lap O'Fallon, IL [email protected] Printer's disclaimer Opinions, conclusions, and recommendations expressed or implied within are solely those of the author. They do not represent the opinions of Mizzou Publishing, or the University of Missouri. Publisher's disclaimer, rights, copying, reprinting, etc Opinions, conclusions, and recommendations expressed or implied within are solely those of the author, except where cited otherwise. They do not represent any U.S. Govt department or agency. This book may be copied or quoted without further permission for non-profit personal use, Air Force safety training, or academic research, with credit to the author and Galleon's Lap. To copy/reprint for any other purpose will require permission. Author's disclaimers Sources can be conflicting, especially initial newspaper reports compared to official information released to the public later. Some names may have a spelling error and I apologize for that. I changed many of the name spellings because I occasionally found more definitive sources written by family members. -

Sanctuary Lost: the Air War for ―Portuguese‖ Guinea, 1963-1974
Sanctuary Lost: The Air War for ―Portuguese‖ Guinea, 1963-1974 Dissertation Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University By Matthew Martin Hurley, MA Graduate Program in History The Ohio State University 2009 Dissertation Committee: Professor John F. Guilmartin, Jr., Advisor Professor Alan Beyerchen Professor Ousman Kobo Copyright by Matthew Martin Hurley 2009 i Abstract From 1963 to 1974, Portugal and the African Party for the Independence of Guinea and Cape Verde (Partido Africano da Independência da Guiné e Cabo Verde, or PAIGC) waged an increasingly intense war for the independence of ―Portuguese‖ Guinea, then a colony but today the Republic of Guinea-Bissau. For most of this conflict Portugal enjoyed virtually unchallenged air supremacy and increasingly based its strategy on this advantage. The Portuguese Air Force (Força Aérea Portuguesa, abbreviated FAP) consequently played a central role in the war for Guinea, at times threatening the PAIGC with military defeat. Portugal‘s reliance on air power compelled the insurgents to search for an effective counter-measure, and by 1973 they succeeded with their acquisition and employment of the Strela-2 shoulder-fired surface-to-air missile, altering the course of the war and the future of Portugal itself in the process. To date, however, no detailed study of this seminal episode in air power history has been conducted. In an international climate plagued by insurgency, terrorism, and the proliferation of sophisticated weapons, the hard lessons learned by Portugal offer enduring insight to historians and current air power practitioners alike. -

The Queen's Regulations for the Royal Air Force Fifth Edition 1999
UNCONTROLLED WHEN PRINTED The Queen’s Regulations for the Royal Air Force Fifth Edition 1999 Amendment List No 30 QR(RAF AL30/Jun 12 UNCONTROLLED WHEN PRINTED UNCONTROLLED WHEN PRINTED INTENTIONALLY BLANK QR(RAF AL30/Jun 12 UNCONTROLLED WHEN PRINTED UNCONTROLLED WHEN PRINTED Contents CHAPTER 1 INTRODUCTION........................................................................................................................................................................................1-1 CHAPTER 2 STRUCTURE OF THE SERVICES AND ORGANIZATION OF THE ROYAL AIR FORCE...........................................................2-1 CHAPTER 3 GENERAL INSTRUCTIONS FOR OFFICERS.......................................................................................................................................3-1 SECTION 1 - INSTRUCTIONS FOR COMMANDERS.................................................................................................................3-1 SECTION 2 - INSTRUCTIONS FOR OFFICERS GENERALLY...............................................................................................3-17 SECTION 3 - INSTRUCTIONS RELATING TO PARTICULAR BRANCHES OF THE SERVICE.....................................3-18 CHAPTER 4 COMMAND, CORRESPONDING RANK AND PRECEDENCE..........................................................................................................4-1 CHAPTER 5 CEREMONIAL............................................................................................................................................................................................5-1 -

HOUSE of REPRESENTATIVES-Tuesday, August 7, 1984
22660 CONGRESSIONAL RECORD-HOUSE August 7, 1984 HOUSE OF REPRESENTATIVES-Tuesday, August 7, 1984 CONFERENCE REPORT ON H.R. Fort Jackson, South Carolina, $35, 760,000. UNITED STATES ARMY CORPS OF ENGINEERS 5604 Fort Knox, Kentucky, $13, 600, 000. Cold Regions Laboratory, New Hampshire, Fort Leavenworth, Kansas, $11,000,000. $3,600,000. Pursuant to the order of Monday, Fort Lee, Virginia, $1,150,000. BALLISTIC MISSILE DEFENSE SYSTEM COMMAND August 6, Mr. PRICE submitted the fol Fort Leonard Wood, Missouri, $6,450,000. lowing conference report and state Fort McClellan, Alabama, $6,300,000. Various locations, $12,800,000. ment on the bill <H.R. 5604) to author Fort Pickett, Virginia, $2,400,000. CLASSIFIED PROJECTS Fort Rucker, Alabama, $2,600,000. Various locations, $3,800,000. ize certain construction at military in Fort Sill, Oklahoma, $27,400,000. stallations for fiscal year 1985, and for Fort Story, Virginia, $6,100,000. OUTSIDE THE UNITED STATES other purposes: MILITARY DISTRICT OF WASHINGTON UNITED STATES ARMY, JAPAN CONFERENCE REPORT CH. REPT. No. 98-962) Fort Myer, Virginia, $700,000. Japan, $1,900,000. The committee of conference on the dis UNITED STATES ARMY MATERIEL DEVELOPMENT EIGHTH UNITED STATES ARMY agreeing votes of the two Houses on the AND READINESS COMMAND Korea, $115,840,000. amendment of the Senate to the bill <H.R. Aberdeen Proving Ground, Maryland, UNITED STATES ARMY, SOUTHERN COMMAND 5604) to authorize certain construction at $65,400,000. Military installations for fiscal year 1985, Anniston Army Depot, Alabama, Honduras, $4,300,000. and for other purposes, having met, after $4,500,000. -
Bomber Command Act of Remembrance Saturday 31 October 2020, 1100
Bomber Command Act of Remembrance Saturday 31 October 2020, 1100 Bomber Command Memorial , Green Park, London Officiant: Rev (Sqn Ldr) Chrissie Lacey, Station Chaplain, RAF High Wycombe Bidding As we give thanks for God’s great works, we remember those who served in Bomber Command and subsequent formations who have lived and died in his service, and in the service of others; we pray for all who suffer through war, and are in need; we ask for his help and blessing that we may do his will, and that the whole world may acknowledge him as Lord and King. Reading From Psalm 103. Read by Warrant Officer Bill Gould The Lord is full of compassion and mercy, slow to anger and of great goodness. As a father is tender towards his children, so is the Lord tender to those who fear him. For he knows of what we are made; he remembers that we are but dust. Our days are like the grass; we flourish like a flower of the field; when the wind goes over it, it is gone and its place will know it no more. But, the merciful goodness of the Lord endures for ever and ever toward those that fear him. Act of Remembrance We remember before God all who served in Bomber Command, on the ground and in the air, and all those effected, especially all those who died, during the bombing campaign to cripple the intentions of those who intended to harm. We remember those who have served in the Bomber role subsequently in theatres of war both far and wide, and who did not return. -

Air Force Weather, Our Heritage 1937-2012.” AFWA Agreed to This Approach in December 2009
AIR FORCE WEATHER OUR HERITAGE 1937 TO 2012 “DIRECTORATE OF WEATHER” Jul 1937 - 1950 May 1958 - 1978 Apr 1991 - Present Air Weather Service Air Force Weather Agency 14 Apr 1943 - 15 Oct 1997 15 Oct 1997 - Present Air Force, Reserve, & Guard Component Weather Units 1 Oct 1991 to Present “MEETING THE CHALLENGE FOR 75 YEARS” TABLE OF CONTENTS COVER PAGE FRONTISPIECE ………….…………………………………………ii SIGNATURE TITLE PAGE ………………………………………..iii DEDICATION……………………………………………………...iv TABLE OF CONTENTS………………………………………….…xii SECRETARY OF DEFENSE LETTER…………………………..…xv FOREWARD……………………………………………………...xvi PREFACE..…………………………………………………..…..xvii ACKNOWLEDGEMENTS…...…………………………………....xix CHAPTER 1—The Roots and Lineage of Air Force Weather……1-1 CHAPTER 2—Chronology1937 – 1946……………………………2-1 CHAPTER 3—Chronology 1947 – 1956……………………….…..3-1 CHAPTER 4—Chronology 1957 – 1966……………………….…..4-1 CHAPTER 5—Chronology 1967 – 1976……………………..…….5-1 CHAPTER 6—Chronology 1977 – 1986………………………..….6-1 CHAPTER 7—Chronology 1987 – 1996……………………….…..7-1 CHAPTER 8—Chronology 1997 – 2006……………………….…..8-1 CHAPTER 9—Chronology 2007 – 2012………………………..….9-1 CHAPTER 10—Air Force Weather Leadership and Staff……....10-1 USAF Directorates of Weather……………………………………10-1 xii Major Air Command Weather Functional Managers……………..10- 32 Air Weather Service Commanders…………………………..…...10- 34 Air Force Weather Agency Commanders………………………...10- 51 USAF Directorate of Weather Staff…………………………...…10- 68 Air Weather Service Staff…………………………………….…10- 71 Air Force Weather Agency Staff………………………………....10- 77 CHAPTER 11—Air Force -

Repor T Resumes
REPOR TRESUMES ED 017 390 PS 000 493 KINDERGARTEN OVERSEAS, ASTUDY OF THE REQUIREMENTSFOR ESTABLISHING KINDERGARTENAS PART OF THE DEPARTMENTOF DEFENSE OVERSEAS DEPENDENTSSCHOOLS. FINAL REPORT. BY- DUNWORTH, JOHN BALL STATE UNIV., MUNCIE,IND. SEP 67 REPORT NUMBER BR-7-0938 PUB DATE . CONTRACT OEC-1-7-1905 EDRS PRICE MF-$1.50 HC-$14.40 358P. DESCRIPTORS- *PROGRAM PROPOSALS,*FEASIBILITY STUDIES,SCHOOL SURVEYS, CURRICULUM GUIDES,*KINDERGARTEN, *FOREIGN COUNTIRES, *ESTIMATED COSTS,PERSONNEL NEEDS, FACILITY INVENTORY, SCHOOL EXPANSION,DEPARTMENT OF DEFENSE, MADE TO THIS REPORT PRESENTSTHE RESULTS OF A STUDY DETERMINE THE REQUIREMENTSFOR EXPANDING OVERSEASDEPENDENT OBJECTIVES OF SCHOOLS TO INCLUDEKINDERGARTEN. THE SPECIFIC THE STUDY WERE (1) TODETERMINE PERSONNELREQUIREMENTS, (2) TO DETERMINE FACILITYREQUIREMENTS,(3) TO DETERMINE EQUIPMENT AND EDUCATIONALMATERIAL REQUIREMENTS,(4) TO DEVELOP A CURRICULUM GUIDE,(5) TO ESTIMATE COSTS.CHAPTERS II AND III DISCUSS THERATIONALE FOR ESTABLISHING KINDERGARTENS AND THE METHODOLOGYUSED IN THE STUDY. CHAPTER CURRICULUM GUIDE THAT WASDEVELOPED, AND f IV PRESENTS THE INCLUDESA SECTION COVERINGTHE INSTRUCTIONALMATERIALS REQUIREMENTS. CHAPTER VCONSIDERS THE PERSONNELREQUIREMENTS, BOTH PROFESSIONAL ANDPARAPROFESSIONAL. CHAPTERVI PRESENTS THE COST ESTIMATES,BROKEN DOWN BY MILITARYOVERSEAS DISTRICTS. INDIVIDUAL SCHOOL SITEREPORTS AND OVERALL THERE ARE MONETARY REQUIREMENTSAREGIVEN FOR EACH DISTRICT. APPENDICES. (DR) f CD lg' N. r--1 CD wC=I /Final Report ,' Project Number 7-0938 ,' Contract Number OEC-1.7-070938-1905 -

Royal Air Force Historical Society Journal 42
ROYAL AIR FORCE HISTORICAL SOCIETY JOURNAL 42 2 The opinions expressed in this publication are those of the contributors concerned and are not necessarily those held by the Royal Air Force Historical Society. Crown Copyright/MOD. The photographs on pages 41, 43, 47, 50, 53, 97, 99, 104 and 106 have been reproduced with permission of the Controller of Her Majesty’s Stationery Office. First published in the UK in 2008 by the Royal Air Force Historical Society All rights reserved. No part of this book may be reproduced or transmitted in any form or by any means, electronic or mechanical including photocopying, recording or by any information storage and retrieval system, without permission from the Publisher in writing. ISSN 1361 4231 Printed by Advance Book Printing Unit 9 Northmoor Park Church Road Northmoor OX29 5UH 3 ROYAL AIR FORCE HISTORICAL SOCIETY President Marshal of the Royal Air Force Sir Michael Beetham GCB CBE DFC AFC Vice-President Air Marshal Sir Frederick Sowrey KCB CBE AFC Committee Chairman Air Vice-Marshal N B Baldwin CB CBE FRAeS Vice-Chairman Group Captain J D Heron OBE Secretary Group Captain K J Dearman FRAeS Membership Secretary Dr Jack Dunham PhD CPsychol AMRAeS Treasurer J Boyes TD CA Members Air Commodore H A Probert MBE MA *J S Cox Esq BA MA *Dr M A Fopp MA FMA FIMgt *Group Captain N Parton BSc (Hons) MA MDA MPhil CEng FRAeS RAF *Wing Commander A J C Walters BSc MA FRAeS RAF Wing Commander C Cummings Editor & Publications Wing Commander C G Jefford MBE BA Manager *Ex Officio 4 CONTENTS THE IMPORTANT OMISSIONS -

Annual Review 2012/13
Royal Air Force Benevolent Fund Annual Review 2012/13 OUR GOALS IN 2012 Continuing – hOW DID WE DO? CONTENTS to repay ‘the Carry out a full strategic review of the RAF Benevolent Fund’s welfare provision to ensure that we continue to meet the needs of the RAF family debt we owe’ whilst ensuring the charity’s financial security. Our review of the Benevolent Fund was completed and FORMER MEMBERS s readers are all too well aware, we are living in very Front cover image: implemented in 2012. By taking sensible, pragmatic OF THE RAF challenging financial times, which appear likely to continue Former SAC and decisions, we have been able to maintain the broad range 2012: facing the A for some time. The pressure on everyone’s pockets, whether RAFBF beneficiary, of welfare work that we undertake and remain “best in challenges together 02 “I am pleased individuals or commercial organisations, has been felt keenly in John Robertson class” in all that we do. We have protected those whom the charitable sector, where fundraising is becoming ever tougher. (centre) with we have helped in the past and continue to provide vital Mick McConnell: I am pleased to say that the Royal Air Force Benevolent Fund’s very to say that the Paralympic sailing support to new beneficiaries. dogged determination 03 generous and loyal supporters have continued to provide us with team-mates Hannah RAFBF’s very the means to undertake our vital welfare work for members of Stodel and Stephen Reaching out to the RAF family 04 the RAF family in need in 2012. -

Ministry of Defence Annual Report and Accounts 2007-08
Ministry of Defence Annual Report and Accounts 2007-2008 Volume I: Annual Performance Report Presented pursuant to the GRA Act 2000 c.20, s.6 Ministry of Defence Annual Report and Accounts Volume I including the Annual Performance Report and Consolidated Departmental Resource Accounts 2007-08 (For the year ended 31 March 2008) Laid in accordance with the Government Resources and Accounts Act 2000 Ordered by the House of Commons to be printed 21 July 2008 London: The Stationery Office 21 July 2008 HC 850-I £51.45 Not to be sold separately © Crown Copyright 2008 The text in this document (excluding the Royal Arms and other departmental or agency logos) may be reproduced free of charge in any format or medium providing it is reproduced accurately and not used in a misleading context. The material must be acknowledged as Crown copyright and the title of the document specified. Where we have identified any third party copyright material you will need to obtain permission from the copyright holders concerned. For any other use of this material please write to Office of Public Sector Information, Information Policy Team, Kew, Richmond, Surrey TW9 4DU or e-mail: [email protected] ISBN: 978 0 10 295509 5 Introduction i. The Ministry of Defence’s Annual Report and Accounts is a comprehensive overview of Defence and how the Department has used the resources authorised by Parliament from April 2007 to March 2008. It has two main sections: the first comprises the Department’s Annual Performance Report for 2007-08, including performance against our Public Service Agreement (PSA) targets. -

HQ Air Command RAF High Wycombe Walters Ash Buckinghamshire HP14 4UE United Kingdom
HQ Air Command RAF High Wycombe Walters Ash Buckinghamshire HP14 4UE United Kingdom E-mail: Air-DResSec- Ref: 11-02-2014-143342-006 [email protected] Mr David Gurtler E-mail address: request-196920- 24 February 2014 [email protected] Dear Mr Gurtler Thank you for your email of 11 February requesting the following information about the number of civilian aircraft movements that took place at RAF Northolt in 2013: 1. The total number of civilian aircraft movements for the year. 2. The total number of military aircraft movements for the year. 3. The total number of 'exempt' civilian movements for the year (notably those carrying royalty, heads of state, or other dignitaries) 4. The number of civilian aircraft movements for each month and the percentage increase that number was compared to the corresponding month in 2012. I am treating your correspondence as a request for information under the Freedom of Information Act 2000 (FOIA). A search for the information has been completed and I can confirm that the information requested is held by the MOD The total number of civilian aircraft movements for 2013 was 10,843. This figure includes commercial, London Air Ambulance (LAA), Police, Government, and military chartered civilian flights. The total number of military aircraft movements for 2013 was 4,127. This figure includes RAF, Army, RN and other military movements. The total number of non-commercial civilian movements for 2013 was 952 (this figure is included within the 10,843 total civilian movements figure). This figure includes for example, LAA, Police, flight checkers, Government and military chartered aircraft.