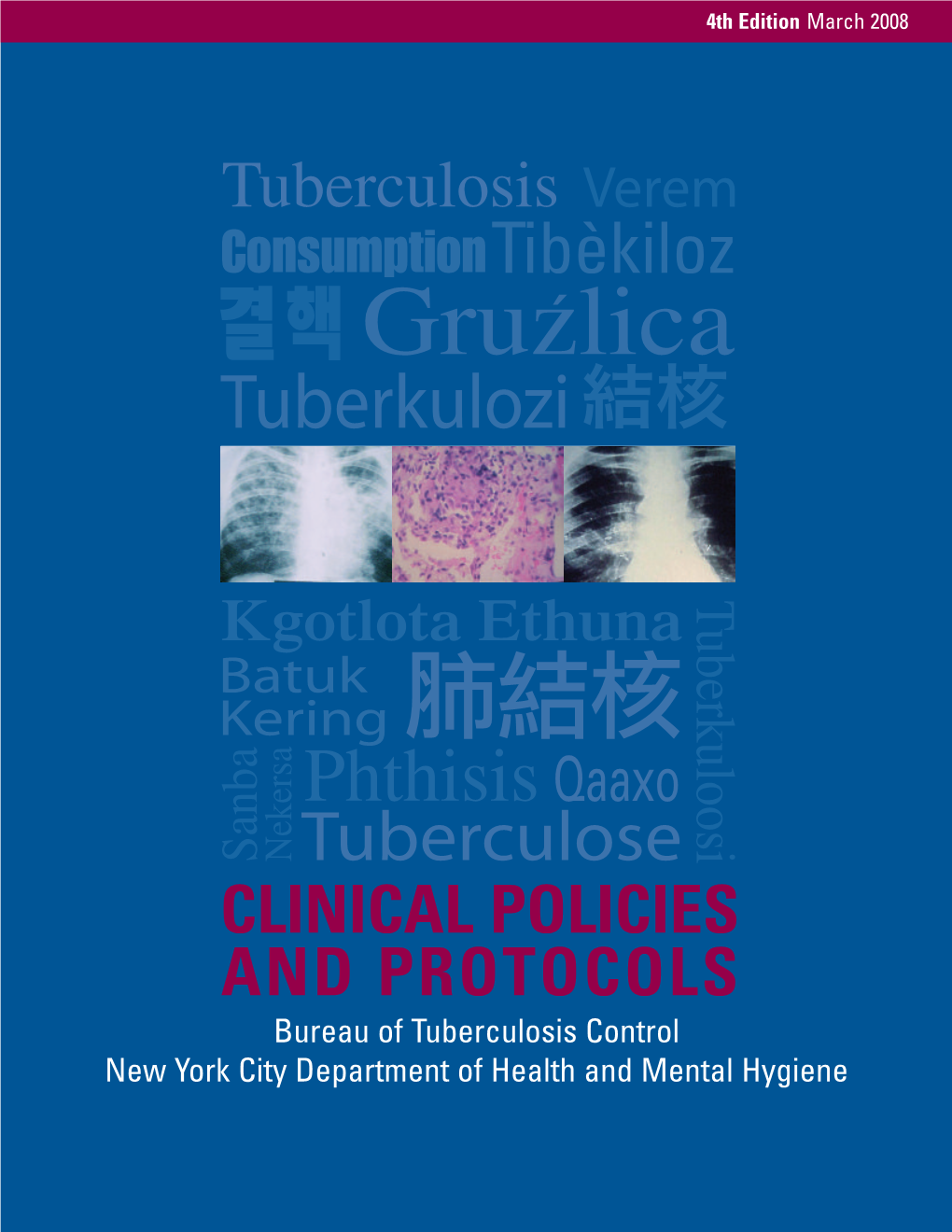
Tuberculosis (TB): Clinical Policies & Protocols
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

EVIDENCE from DACA Elira Kuka Na'ama S
NBER WORKING PAPER SERIES DO HUMAN CAPITAL DECISIONS RESPOND TO THE RETURNS TO EDUCATION? EVIDENCE FROM DACA Elira Kuka Na'ama Shenhav Kevin Shih Working Paper 24315 http://www.nber.org/papers/w24315 NATIONAL BUREAU OF ECONOMIC RESEARCH 1050 Massachusetts Avenue Cambridge, MA 02138 February 2018 We would like to thank Anna Aizer, Catalina Amuedo-Dorantes, Elizabeth Cascio, Aimee Chin, Chloe East, Hilary Hoynes, Chris Karbownik, Melissa Kearney, Ethan Lewis, Dan Millimet, Matt Notowidigdo, Francesc Ortega, Marianne Page, Bruce Sacerdote, Diane Schanzenbach, and Doug Staiger, as well as seminar participants at Northwestern MPES, University of Connecticut, Oklahoma State University, the US Census Bureau, and conference participants at the Barcelona GSE Summer Forum Migration meeting, UC Davis Alumni Conference, WEAI Conference, SEA Conference, SOLE Annual Meeting, and AEA Annual Meeting for helpful suggestions and feedback. We are also grateful to Marcella Alsan for her feedback and for generously sharing data on Secure Communities activation dates with us. The views expressed herein are those of the authors and do not necessarily reflect the views of the National Bureau of Economic Research. NBER working papers are circulated for discussion and comment purposes. They have not been peer- reviewed or been subject to the review by the NBER Board of Directors that accompanies official NBER publications. © 2018 by Elira Kuka, Na'ama Shenhav, and Kevin Shih. All rights reserved. Short sections of text, not to exceed two paragraphs, may be quoted without explicit permission provided that full credit, including © notice, is given to the source. Do Human Capital Decisions Respond to the Returns to Education? Evidence from DACA Elira Kuka, Na'ama Shenhav, and Kevin Shih NBER Working Paper No. -

World Bank Document
WPS6567 Policy Research Working Paper 6567 Public Disclosure Authorized Is Small Better? A Comparison of the Effect of Large and Small Dams Public Disclosure Authorized on Cropland Productivity in South Africa Elodie Blanc Eric Strobl Public Disclosure Authorized The World Bank Public Disclosure Authorized Development Economics Vice Presidency Partnerships, Capacity Building Unit August 2013 Policy Research Working Paper 6567 Abstract This study estimates and compares the effects of small effect on cropland within the vicinity. However, their and large irrigation dams on cropland productivity in existence can enhance the relatively small positive impact South Africa. To this end, a panel data set of South of local small dams. Although a cost-benefit analysis of African river basins is constructed. The econometric irrigation benefits shows that small dams may be more analysis reveals that although large dams increase viable than large ones, large dams can play a potentially cropland productivity downstream, they have a negative important role within a system of both types of dams. This paper is a product of the Partnerships, Capacity Building Unit, Development Economics Vice Presidency. It is part of a larger effort by the World Bank to provide open access to its research and make a contribution to development policy discussions around the world. Policy Research Working Papers are also posted on the Web at http://econ.worldbank.org. The authors may be contacted at is [email protected]. The Policy Research Working Paper Series disseminates the findings of work in progress to encourage the exchange of ideas about development issues. An objective of the series is to get the findings out quickly, even if the presentations are less than fully polished. -
Promotion, Turnover and Satisfaction in the Army Civilian Workforce
Dissertation Promotion, Turnover, and Satisfaction in the Army Civilian Workforce An Analysis of Features of Occupation Ladders and Employee Perspectives of the Work Environment Christina E. Steiner This document was submitted as a dissertation in December 2018 in partial fulfillment of the requirements of the doctoral degree in public policy analysis at the Pardee RAND Graduate School. The faculty committee that supervised and approved the dissertation consisted of of Lawrence M. Hanser (Chair), Shanthi Nataraj, Gery Ryan, and Curt Gilroy (outside reader). PARDEE RAND GRADUATE SCHOOL For more information on this publication, visit http://www.rand.org/pubs/rgs_dissertations/RGSD434.html Published 2019 by the RAND Corporation, Santa Monica, Calif. R® is a registered trademark Limited Print and Electronic Distribution Rights This document and trademark(s) contained herein are protected by law. This representation of RAND intellectual property is provided for noncommercial use only. Unauthorized posting of this publication online is prohibited. Permission is given to duplicate this document for personal use only, as long as it is unaltered and complete. Permission is required from RAND to reproduce, or reuse in another form, any of its research documents for commercial use. For information on reprint and linking permissions, please visit www.rand.org/pubs/permissions.html. The RAND Corporation is a research organization that develops solutions to public policy challenges to help make communities throughout the world safer and more secure, healthier and more prosperous. RAND is nonprofit, nonpartisan, and committed to the public interest. RAND’s publications do not necessarily reflect the opinions of its research clients and sponsors. -

March 25—Minutes
VIRTUAL MEETING OF THE BOARD OF DIRECTORS March 25, 2021 at 4:00 pm MINUTES Directors Present: Basil Seggos, Chair Vicki Been Leslie Wright for Director Kulleseid Michael Kuh Rose Harvey Sarah Nielson for Director Silver Aloysee Heredia Jarmoszuk Jeffrey Kaplan Purnima Kapur Lowell Kern Pamela Frederick Lawrence Goldberg Appearances: Hudson River Park Trust: Noreen Doyle, Acting President and CEO Daniel Kurtz, CFO and Executive Vice President, Finance & Real Estate Christine Fazio, General Counsel Also Present: Connie Fishman, Hudson River Park Friends Jeffrey LeFrancois, Advisory Council Chair 1 With a quorum being present, Chair Seggos called to order the March 25, 2021 meeting of the Hudson River Park Trust Board of Directors. He explained that due to the coronavirus pandemic and consistent with Governor Cuomo’s Executive Order 202.1 issued on March 12, 2020, this meeting is being held remotely via a Zoom teleconference enabling participation of the Directors and the general public. Chair Seggos then noted that all Directors have received the Agenda materials in advance of this meeting and are free to ask questions or comment at any time on the action items submitted for approval today. Chair Seggos further noted that questions or comments from the audience will not be entertained at this meeting. I note that the Board memos and resolutions on today’s agenda have been posted on the Trust website in the link entitled Board Meetings, Bylaws and Other Materials under Board Agendas and Minutes and thus are available to the public. Chair -

A Content Analysis of Liberals' and Conservatives' Respective
Georgia State University ScholarWorks @ Georgia State University Sociology Theses Department of Sociology 1-6-2017 Red Show, Blue Show: A Content Analysis of Liberals’ and Conservatives’ Respective Television Favorites Nicholas Rogers Follow this and additional works at: https://scholarworks.gsu.edu/sociology_theses Recommended Citation Rogers, Nicholas, "Red Show, Blue Show: A Content Analysis of Liberals’ and Conservatives’ Respective Television Favorites." Thesis, Georgia State University, 2017. https://scholarworks.gsu.edu/sociology_theses/63 This Thesis is brought to you for free and open access by the Department of Sociology at ScholarWorks @ Georgia State University. It has been accepted for inclusion in Sociology Theses by an authorized administrator of ScholarWorks @ Georgia State University. For more information, please contact [email protected]. RED SHOW, BLUE SHOW: A CONTENT ANALYSIS OF LIBERALS’ AND CONSERVATIVES’ RESPECTIVE TELEVISION FAVORITES by NICK ROGERS Under the Direction of Ben L. Kail, PhD ABSTRACT Ideological partisans in the United States are increasingly “sorting” themselves along cultural lines, from the cable news stations they watch to the chain restaurants they prefer. How do partisans seem to “know” how to sort themselves along ideological lines in cultural realms that offer no obvious political cues? To investigate this question, I look to the realm of narrative television, where conservatives and liberals have certain unique favorite programs despite the programs lacking any overt political content. I employ a quantitative content analysis to demonstrate that the substance of these polarizing shows relate to the social traits of curiosity, conformity, relativism, dogmatism, tribalism, vigilance, and chastity, which have previously been demonstrated to correspond to political ideology. -

The Effects of Extreme Media on Political Behavior, Attitudes, and Media Selection
Georgia State University ScholarWorks @ Georgia State University Political Science Dissertations Department of Political Science Spring 1-23-2013 The Effects of Extreme Media on Political Behavior, Attitudes, and Media Selection James B. Taylor Georgia State University Follow this and additional works at: https://scholarworks.gsu.edu/political_science_diss Recommended Citation Taylor, James B., "The Effects of Extreme Media on Political Behavior, Attitudes, and Media Selection." Dissertation, Georgia State University, 2013. https://scholarworks.gsu.edu/political_science_diss/28 This Dissertation is brought to you for free and open access by the Department of Political Science at ScholarWorks @ Georgia State University. It has been accepted for inclusion in Political Science Dissertations by an authorized administrator of ScholarWorks @ Georgia State University. For more information, please contact [email protected]. THE EFFECTS OF EXTREME MEDIA ON POLITICAL BEHAVIOR, ATTITUDES, AND MEDIA SELECTION by JAMES BENJAMIN TAYLOR Under the Direction of Sean Richey ABSTRACT This dissertation examines the role of extreme media (i.e. political talk radio and cable news opinion shows) on the political attitudes of viewers and listeners. I investigate whether extreme media has both positive and negative externalities for democratic citizenship. Specif- ically, I use laboratory experiments, national survey data, and qualitative interviews to test the impact of extreme media on viewers' political knowledge, trust in government, efficacy, and political tolerance. I use laboratory experiments in controlled settings to uncover the impact of viewership on political knowledge, trust in government, and efficacy. I confirm these lab findings with the national survey data, by using propensity score matching and ordered probit models to demonstrate that exposure to extreme media produces political knowledge and efficacy, but decreases trust in government. -
USCIS Publishes Customer Satisfaction Survey on E-Verify
Department of Homeland Security U.S. Citizenship and Immigration Services Customer Satisfaction Survey – E-Verify Final Report October 15, 2010 USCIS – E-Verify 2010 Customer Satisfaction Survey This page intentionally left blank. CFI Group Final Report USCIS – E-Verify 2010 Customer Satisfaction Survey Table of Contents Executive Summary 3 Overall Findings and Recommendations 5 DetailedReport 7 Introduction & Methodology 9 Respondent Background 11 Customer Satisfaction Index 14 CustomerSatisfaction Model 15 DriversofSatisfaction 19 PriorityMatrix 27 Marketing/Outreach 28 Outcomes 29 Appendices Appendix A: Survey Questionnaire 30 Appendix B: Non-Modeled Responses 44 Appendix C: Results Tables 58 Appendix D: Verbatim Comments 72 CFI Group 1 Final Report USCIS – E-Verify 2010 Customer Satisfaction Survey This page intentionally left blank. CFI Group 2 Final Report USCIS – E-Verify 2010 Customer Satisfaction Survey EXECUTIVE SUMMARY CFI Group 3 Final Report USCIS – E-Verify 2010 Customer Satisfaction Survey This page intentionally left blank. CFI Group 4 Final Report USCIS – E-Verify 2010 Customer Satisfaction Survey Overall Findings and Recommendations This report focuses on the customer satisfaction of companies currently enrolled in the E-Verify program. The Customer Satisfaction Index for E-Verify is 82. This is a positive result, especially when compared to benchmarks such as the latest federal government satisfaction index, which is 69. Even more so when considering that many of the users signed up not voluntarily, but because of a requirement from local, state or federal government or a parent company. In addition to rating overall satisfaction with E-Verify, users evaluated different areas of performance involving E-Verify depending on whether that particular area applied to the user. -
The Day After Tomorrow
OF ECONOMIC POLICY IN THE OF ECONOMIC POLICY INTHE A HANDBOOK ONTHEFUTURE AFTER THE DAY Public Disclosure Authorized Public Disclosure Authorized Public Disclosure Authorized Public Disclosure Authorized CANUTOANDMARCELOGIUGALE,EDITORS OTAVIANO DEVELOPING WORLD TOMORROW THE DAY AFTER TOMORROW THE DAY AFTER TOMORROW A Handbook on the Future of Economic Policy in the Developing World OTAVIANO CANUTO AND MARCELO GIUGALE Editors © 2010 The International Bank for Reconstruction and Development / The World Bank 1818 H Street NW Washington DC 20433 Telephone: 202-473-1000 Internet: www.worldbank.org All rights reserved 1 2 3 4 13 12 11 10 This volume is a product of the staff of the International Bank for Reconstruction and Develop- ment / The World Bank. The fi ndings, interpretations, and conclusions expressed in this volume do not necessarily refl ect the views of the Executive Directors of The World Bank or the governments they represent. The World Bank does not guarantee the accuracy of the data included in this work. The boundaries, colors, denominations, and other information shown on any map in this work do not imply any judgement on the part of The World Bank concerning the legal status of any territory or the endorse- ment or acceptance of such boundaries. Rights and Permissions The material in this publication is copyrighted. Copying and/or transmitting portions or all of this work without permission may be a violation of applicable law. The International Bank for Recon- struction and Development / The World Bank encourages dissemination of its work and will nor- mally grant permission to reproduce portions of the work promptly. -

Opposition Parties and Anti-Government Protests in Comparative Perspective
OPPOSITION PARTIES AND ANTI-GOVERNMENT PROTESTS IN COMPARATIVE PERSPECTIVE by Yen-Pin Su B.A., National Taiwan University, 2001 M.A., National Taiwan University, 2005 Submitted to the Graduate Faculty of the Dietrich School of Arts and Sciences in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Pittsburgh 2014 UNIVERSITY OF PITTSBURGH THE DIETRICH SCHOOL OF ARTS AND SCIENCES This dissertation was presented by Yen-Pin Su It was defended on March 26, 2014 and approved by Steven Finkel, Daniel Wallace Professor, Political Science John Markoff, Distinguished University Professor, Sociology Co-Dissertation Advisor: Scott Morgenstern, Associate Professor, Political Science Co-Dissertation Advisor: Aníbal Pérez-Liñán, Associate Professor, Political Science ii Copyright © by Yen-Pin Su 2014 iii OPPOSITION PARTIES AND ANTI-GOVERNMENT PROTESTS IN COMPARATIVE PERSPECTIVE Yen-Pin Su, PhD University of Pittsburgh, 2014 My dissertation adopts an interdisciplinary approach to examine the relationship between political parties and social movements in democratic countries. This work touches on the debates about why protest movements emerge and the literature on the consequences of party politics. It draws on rational choice and political process theories to explain the variation in anti- government protests in the context of democracies. I argue that the mobilization capacity of opposition parties matters for understanding the differing levels of protests. Specifically, focusing on the size and unity of the opposition camp as two unique dimensions of mobilization capacity, I contend that a larger opposition camp should encourage more anti-government protests only if the camp is more united. Moreover, I argue that, because of the differences in socio-economic backgrounds, political development trajectories, and the role of parties as mobilization agents, the effects of opposition mobilization capacity should work differently in developed countries and developing countries. -

View All Four Women Again, but with Another Purpose in Mind
DEMYSTIFYING THE NOTION, “THE WEST IS BETTER”: A GERMAN ORAL HISTORY PROJECT Jennifer Stanek A Thesis Submitted to the Graduate College of Bowling Green State University in partial fulfillment of the requirements of the degree of MASTER OF ARTS May 2011 Committee: Dr. Christina Guenther, Advisor Dr. Kristie Foell ii ABSTRACT Dr. Christina Guenther, Advisor I began my project in 2004 as an oral history project, involving four German women, with the purpose of finding out what motivated them either to flee East Germany before the construction of the Berlin Wall or stay. Five years later I wished to revive my project and interview all four women again, but with another purpose in mind. What had started out as a desire to understand my own family’s past turned into a desire to gain a better idea of the complexity of the notion, “the West is better,” and, therefore, an even better understanding of what moved a people across dangerous borders. In this thesis I examine what the idea, “the West is better,” meant to real individuals, who chose a life in the West either before the construction of the Wall on August 13, 1961 or in the 1980s before the fall of the Wall. I examine how this notion applied to their experiences specifically, the GDR-refugees’ contribution to the creation and perpetuation of this idea, and how this concept has affected the German people since 1949. The notion, “the West is better,” assumed much mythical character during the existence of the GDR, which it largely has not shed. -

Combat-Related Reproductive Trauma: Implications for Quality of Life and the Reproductive Narrative
Bryn Mawr College Scholarship, Research, and Creative Work at Bryn Mawr College Bryn Mawr College Dissertations and Theses 2018 Combat-Related Reproductive Trauma: Implications for Quality of Life and the Reproductive Narrative Laura S. Covington Bryn Mawr College, [email protected] Follow this and additional works at: https://repository.brynmawr.edu/dissertations Part of the Social Work Commons Custom Citation Covington, Laura S. "Combat-Related Reproductive Trauma: Implications for Quality of Life and the Reproductive Narrative." PhD Diss., Bryn Mawr College, 2018. This paper is posted at Scholarship, Research, and Creative Work at Bryn Mawr College. https://repository.brynmawr.edu/dissertations/188 For more information, please contact [email protected]. Combat-Related Reproductive Trauma: Implications for Quality of Life and the Reproductive Narrative by Laura S. Covington March 2018 Submitted to the Faculty of the Graduate School of Social Work and Social Research of Bryn Mawr College in partial fulfillment of the requirements for the Degree of Doctor of Philosophy COPYRIGHT 2018 Laura S. Covington Copyright Notice: The dissertation submitted as part of the requirements for a degree is the property of the College. However, the author of the dissertation owns and retains the copyright in the dissertation, without further registration formalities. ii Abstract Little research exists on the experiences of a combat-related injury that impairs fertility. This dissertation is a qualitative exploration of the lived experiences of military members after a genitourinary (GU) injury. It addresses the biological, psychological, and social impact on quality of life during recovery and subsequent attitudes about family development and sexual functioning. -

Migration, International Trade and Capital Formation: Cause Or Effect?
IZA DP No. 6975 Migration, International Trade and Capital Formation: Cause or Effect? Gabriel Felbermayr Volker Grossmann Wilhelm Kohler October 2012 DISCUSSION PAPER SERIES Forschungsinstitut zur Zukunft der Arbeit Institute for the Study of Labor Migration, International Trade and Capital Formation: Cause or Effect? Gabriel Felbermayr University of Munich, Ifo Institute and GEP Nottingham Volker Grossmann University of Fribourg, IZA and CESifo Wilhelm Kohler University of Tübingen, CESifo and GEP Nottingham Discussion Paper No. 6975 October 2012 IZA P.O. Box 7240 53072 Bonn Germany Phone: +49-228-3894-0 Fax: +49-228-3894-180 E-mail: [email protected] Any opinions expressed here are those of the author(s) and not those of IZA. Research published in this series may include views on policy, but the institute itself takes no institutional policy positions. The IZA research network is committed to the IZA Guiding Principles of Research Integrity. The Institute for the Study of Labor (IZA) in Bonn is a local and virtual international research center and a place of communication between science, politics and business. IZA is an independent nonprofit organization supported by Deutsche Post Foundation. The center is associated with the University of Bonn and offers a stimulating research environment through its international network, workshops and conferences, data service, project support, research visits and doctoral program. IZA engages in (i) original and internationally competitive research in all fields of labor economics, (ii) development of policy concepts, and (iii) dissemination of research results and concepts to the interested public. IZA Discussion Papers often represent preliminary work and are circulated to encourage discussion.