Combatting Discrimination in Access to Medical Care During COVID-19
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Gendered Ageism in the Canadian Workforce the Economic, Social and Emotional Effects of Isolating Older Women from the Workplace
Gendered Ageism in the Canadian Workforce The economic, social and emotional effects of isolating older women from the workplace By Sophie Beaton Social Connectedness Fellow 2018 Samuel Centre for Social Connectedness www.socialconnectedness.org August 2018 Table of contents Abstract 3 Introduction 4 Gendered Ageism 5 Gendered Ageism in the Workforce 7 Methodology 9 Findings from Interviews 12 Discussion 21 Bibliography 26 1 Abstract This research was conducted to examine the impacts of gendered ageism in the workplace for women over 50. The aim of this research was to determine how older women are impacted on an economic, social and emotional level when they experience this type of discrimination at work. The findings show that women over 50 are both unfairly forced out of their positions and have unjustified difficulty reentering the workforce, which then negatively impacts components of their lives such as economic stability, self-esteem, social connectedness and emotional well- being. To alleviate these impacts, it is recommended that programs and policies are put in place that make it easier for women to pursue legal action against their employer, and that social groups are created that provide networking opportunities and emotional support for older women. Key Words: gender, age, discrimination, workforce, women, employment, isolation, stereotype 2 Introduction Across North America, the workforce is aging. As demographics shift, so will the working age population making it essential that older individuals continue to remain active -

AMA Journal of Ethics® January 2021, Volume 23, Number 1: E64-69
AMA Journal of Ethics® January 2021, Volume 23, Number 1: E64-69 MEDICINE AND SOCIETY: PEER-REVIEWED ARTICLE Cautions About Medicalized Dehumanization Alexandra Minna Stern, PhD Abstract Critical lessons can be gleaned by examining 2 of the most salient relationships between racism and medicine during the Holocaust: (1) connections between racism and dehumanization that have immediate, lethal, deleterious, longer-term consequences and (2) intersections of racism and other forms of hatred and bigotry, including discrimination against people with disabilities; lesbian, gay, bisexual, transgender, and queer people; and social and religious minorities. When considered in the US context, these lessons amplify need for reflection about the history of eugenics and human experimentation and about the persistence of racism and ableism in health care. To claim one AMA PRA Category 1 CreditTM for the CME activity associated with this article, you must do the following: (1) read this article in its entirety, (2) answer at least 80 percent of the quiz questions correctly, and (3) complete an evaluation. The quiz, evaluation, and form for claiming AMA PRA Category 1 CreditTM are available through the AMA Ed HubTM. Racism, Medicine, and Dehumanization During the Third Reich The murder of 6 million Jews and millions of other people in Nazi Germany was made possible by dehumanization on a pervasive and catastrophic scale. In her classic book, The Origins of Totalitarianism, Hannah Arendt analyzes historical conditions that gave rise to Nazism, arguing that an overriding impulse of Nazi ideology was to deprive its victims initially of their juridical and civil rights and next of their existential rights, ultimately denying perceived enemies of “the right to have rights.”1 This process turned social and human beings into “bare life,” naked and exposed to the regime’s brutalities.2,3 Nazi Germany, of course, was not the first dehumanizing regime. -

Why Is Ageism Unacceptable?
What is ageism? Ageism, discrimination based on a person’s age, has a dramatic detrimental effect on older people but this is often not acknowledged. We want to highlight age discrimination as a major issue that needs to be addressed in order to ensure the fair treatment of older people. Some of these situations may be familiar to you: Losing your job because of your age Being refused interest-free credit a new credit card or car insurance because of your age Finding that an organisations attitude to older people results in you receiving a lower quality of service Age limits on benefits such as Disability Living Allowance A doctor deciding not to refer you to a consultant because you are ‘too old Ageism is illegal in employment, training and education. Why is Ageism unacceptable? Ageism is not obvious. You may not be aware it's happening but it may result in you receiving different treatment. Until the Equality Bill comes into force in 2012, making ageism unlawful in the provision of products and services where it has negative or harmful consequences, there is no legal remedy to stop it. But we’re determined to highlight its effects and campaign against it. Ageism - often referred to as age discrimination - exists in many areas of life and not only causes personal hardship and injustice but also harms the economy. We are campaigning to end ageism in all walks of life. We believe older people should have equal rights to participate and enjoy all the benefits of a modern society. Am I being discriminated against? It’s not always easy to spot age discrimination as there are several kinds some of which are subtle and unintentional: Direct discrimination This means treating someone less favourably because of their age or because of the age they appear to be. -

Diversity, Equity and Inclusion – Glossary of Terms Ableism
Diversity, Equity and Inclusion – Glossary of Terms Ableism- discrimination against persons with mental and/or physical disabilities; social structures that favor able-bodied individuals. (The National Multicultural Institute) Acculturation- the process of learning and incorporating the language, values, beliefs, and behaviors that makes up a distinct culture. This concept is not to be confused with assimilation, where an individual or group may give up certain aspects of its culture in order to adapt to that of the prevailing culture. (The National Multicultural Institute) Affirmative Action- proactive policies and procedures for remedying the effect of past discrimination and ensuring the implementation of equal employment and educational opportunities, for recruiting, hiring, training and promoting women, minorities, people with disabilities and veterans in compliance with the federal requirements enforced by the Office of Federal Contract Compliance Programs (OFCCP). (Society for Human Resources Management) Ageism- discrimination against individuals because of their age, often based on stereotypes. (The National Multicultural Institute) Ally- a person who takes action against oppression out of a belief that eliminating oppression will benefit members of targeted groups and advantage groups. Allies acknowledge disadvantage and oppression of other groups than their own, take supportive action on their behalf, commit to reducing their own complicity or collusion in oppression of these groups, and invest in strengthening their own knowledge and awareness of oppression. (Center for Assessment and Policy Development) Anti-Oppression - Recognizing and deconstructing the systemic, institutional and personal forms of disempowerment used by certain groups over others; actively challenging the different forms of oppression. (Center for Anti-Oppressive Education) Bias - a positive or negative inclination towards a person, group, or community; can lead to stereotyping. -

What Does a Job Candidate's Age Signal to Employers?
DISCUSSION PAPER SERIES IZA DP No. 12849 What Does a Job Candidate’s Age Signal to Employers? Hannah Van Borm Ian Burn Stijn Baert DECEMBER 2019 DISCUSSION PAPER SERIES IZA DP No. 12849 What Does a Job Candidate’s Age Signal to Employers? Hannah Van Borm Ghent University Ian Burn University of Liverpool and SOFI Stijn Baert Ghent University, University of Antwerp, Université catholique de Louvain, IZA and IMISCOE DECEMBER 2019 Any opinions expressed in this paper are those of the author(s) and not those of IZA. Research published in this series may include views on policy, but IZA takes no institutional policy positions. The IZA research network is committed to the IZA Guiding Principles of Research Integrity. The IZA Institute of Labor Economics is an independent economic research institute that conducts research in labor economics and offers evidence-based policy advice on labor market issues. Supported by the Deutsche Post Foundation, IZA runs the world’s largest network of economists, whose research aims to provide answers to the global labor market challenges of our time. Our key objective is to build bridges between academic research, policymakers and society. IZA Discussion Papers often represent preliminary work and are circulated to encourage discussion. Citation of such a paper should account for its provisional character. A revised version may be available directly from the author. ISSN: 2365-9793 IZA – Institute of Labor Economics Schaumburg-Lippe-Straße 5–9 Phone: +49-228-3894-0 53113 Bonn, Germany Email: [email protected] www.iza.org IZA DP No. 12849 DECEMBER 2019 ABSTRACT What Does a Job Candidate’s Age Signal to Employers?* Research has shown that hiring discrimination is a barrier for older job candidates in many OECD countries. -

SOCIAL ACCEPTANCE of AGE DISCRIMINATION by NICK M
SOCIAL ACCEPTANCE OF AGE DISCRIMINATION By NICK M. WISDOM Bachelor of Science in Psychology Oklahoma Christian University Edmond, OK 2005 Master of Science in Clinical Psychology Oklahoma State University Stillwater, OK 2008 Submitted to the Faculty of the Graduate College of the Oklahoma State University in partial fulfillment of the requirements for the Degree of DOCTOR OF PHILOSOPHY July, 2010 SOCIAL ACCEPTANCE OF AGE DISCRIMINATION: Dissertation Approved: Dr. John Chaney Dissertation Adviser Dr. Jennifer L. Callahan Dr. James W. Grice Dr. Alex Bishop Outside Committee Member Dr. Mark E. Payton Dean of the Graduate College ii TABLE OF CONTENTS Chapter Page I. INTRODUCTION ......................................................................................................1 II. REVIEW OF LITERATURE....................................................................................6 Terror Management Theory .....................................................................................7 Social-Developmental Perspective ..........................................................................9 Communication ......................................................................................................12 Ageism in the Media ..............................................................................................14 Ageism in Health Care ...........................................................................................17 Ageism in the Workplace .......................................................................................20 -
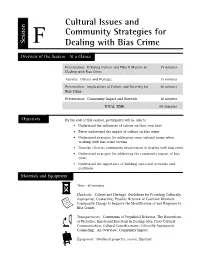
Cultural Issues and Community Strategies for Dealing with Bias Crime
Cultural Issues and Community Strategies for Session F Dealing with Bias Crime Overview of the Session: At a Glance Presentation: Defining Culture and Why It Matters in 15 minutes Dealing with Bias Crime Activity: Culture and Heritage 15 minutes Presentation: Implications of Culture and Diversity for 20 minutes Bias Crime Presentation: Community Impact and Outreach 10 minutes TOTAL TIME 60 minutes Objectives By the end of this session, participants will be able to: • Understand the influences of culture on their own lives • Better understand the impact of culture on bias crime • Understand strategies for addressing cross-cultural issues when working with bias crime victims • Describe effective community involvement in dealing with bias crime • Understand strategies for addressing the community impact of bias crime • Understand the importance of building successful networks and coalitions Materials and Equipment Time: 60 minutes Handouts: Culture and Heritage; Guidelines for Providing Culturally Appropriate Counseling; Possible Network or Coalition Members; Community Change to Improve the Identification of and Response to Bias Crimes Transparencies: Continuum of Prejudicial Behavior; The Dimensions of Prejudice; Emotional Reactions in Dealing with Cross-Cultural Communication; Cultural Considerations; Culturally Appropriate Counseling: An Overview; Community Impact Equipment: Overhead projector; screen; flipchart Session F. Cultural Issues and Community Strategies for Dealing with Bias Crime Instructor’s Notes I. Presentation: Defining Culture and Why It Matters in Dealing with Bias Crime (15 minutes) Explain that this session will provide an understanding of culture, diversity, prejudice, and bigotry, and their relationship to bias crime. The session will not comprehensively deal with specific cultural groups and their history, customs, or beliefs, but rather provide an overview. -

ABSTRACT AGEISM in the NOVELS of JANE AUSTEN This Project
ABSTRACT AGEISM IN THE NOVELS OF JANE AUSTEN This project seeks to examine displays of ageism within Jane Austen’s six core novels. Ageism is defined as prejudice and discrimination against an individual based upon age. First, I studied a specific character who demonstrates ageism, Emma Woodhouse. The possession of wealth blinds her to her obligations towards the elderly Mrs. Bates and singlewoman Miss Bates, while also enabling her father’s hypochondria via benign ageism. Secondly, I examine Jane Austen’s commentary (through her narration) on older men and older women. During these assessments, I found that ageist attitudes come in two varieties in the novels of Jane Austen: characters who are overtly ageist are to be seen as erring in judgment (no matter how benign the behavior), while Austen’s use of ageist stereotypes serves to promote the independence of her heroines by weakening their figures of authority. Monica Renee Medina May 2011 AGEISM IN THE NOVELS OF JANE AUSTEN by Monica Renee Medina A thesis submitted in partial fulfillment of the requirements for the degree of Master of Arts in English in the College of Arts and Humanities California State University, Fresno May 2011 APPROVED For the Department of English: We, the undersigned, certify that the thesis of the following student meets the required standards of scholarship, format, and style of the university and the student's graduate degree program for the awarding of the master's degree. Monica Renee Medina Thesis Author Ruth Jenkins (Chair) English Laurel Hendrix English Clare-Marie Wall English For the University Graduate Committee: Dean, Division of Graduate Studies AUTHORIZATION FOR REPRODUCTION OF MASTER’S THESIS X I grant permission for the reproduction of this thesis in part or in its entirety without further authorization from me, on the condition that the person or agency requesting reproduction absorbs the cost and provides proper acknowledgment of authorship. -

Legacies of the Holocaust in Health Care
Legacies of the Holocaust in Health Care January 2021, Volume 23, Number 1: E1-81 From the Editor Why Does Medical Participation in the Holocaust Still Matter? 3 Tessa Chelouche, MD and Matthew K. Wynia, MD, MPH Case and Commentary How Should Clinicians’ Involvement in the Holocaust Inform Contemporary Responsibilities to Protect Public Safety? 6 Matthew K. Wynia, MD, MPH How Should History of Physician Involvement in the Holocaust Inform How Physicians Approach Employers? 12 Mark G. Kuczewski, PhD and Amy Blair, MD How Should a Physician Respond to Discovering Her Patient Has Been Forcibly Sterilized? 18 Rebecca Kluchin, PhD Medical Education Teaching Health Professions Students About the Holocaust 26 William S. Silvers, MD, Matthew K. Wynia, MD, MPH, Mark A. Levine, MD, and Meleah Himber, MEd How Should Students Learn About Contemporary Implications of Health Professionals’ Roles in the Holocaust? 31 Robert Baker, PhD Health Law Health Professionals, Human Rights Violations at the US-Mexico Border, and Holocaust Legacy 38 Susannah Sirkin, MEd, Kathryn Hampton, MSt, and Ranit Mishori, MD, MHS AMA Journal of Ethics, January 2021 1 AMA Code Says AMA Code of Medical Ethics’ Opinions Related to the Legacies of the Holocaust in Health Care 46 Scott J. Schweikart, JD, MBE and Danielle Hahn Chaet, MSB State of the Art and Science “Prevention” and Human Gene Editing Governance 49 Eric T. Juengst, PhD How Should We Regard Information Gathered in Nazi Experiments? 55 Arthur L. Caplan, PhD Medicine and Society Teaching Hard Truths About Medicine and the Holocaust 59 Tessa Chelouche, MD Cautions About Medicalized Dehumanization 64 Alexandra Minna Stern, PhD Art of Medicine What Art Museums Can Teach Today’s Clinicians About How to Orient Themselves to Their Professions’ Roles in the Holocaust 70 Martina Lentino Viewpoint A Call to Commemorate International Holocaust Remembrance Day, January 27, in All Health Science Schools 75 Matthew K. -

Early Children's Literature and Aging
Creative Education, 2016, 7, 2604-2612 http://www.scirp.org/journal/ce ISSN Online: 2151-4771 ISSN Print: 2151-4755 Early Children’s Literature and Aging Sandra L. McGuire Professor Emeritus, The University of Tennessee, Knoxville, USA How to cite this paper: McGuire, S. L. (2016). Abstract Early Children’s Literature and Aging. Crea- tive Education, 7, 2604-2612. Increased longevity is a worldwide phenomenon placing emphasis on the need for http://dx.doi.org/10.4236/ce.2016.717245 preparation for life’s later years and for maximizing the potentials of these years. Today’s children will be the older adults of tomorrow. A resource that can help to Received: October 14, 2016 Accepted: November 4, 2016 educate them about aging and prepare them for the long life ahead is early children’s Published: November 7, 2016 literature (Preschool-Primary). This literature can provide children with a holistic view of aging, teach them about aging and the aging process, promote positive atti- Copyright © 2016 by author and tudes about aging, and promote positive aging. Selecting early children’s literature Scientific Research Publishing Inc. This work is licensed under the Creative for aging content, resources for finding early children’s literature to promote positive Commons Attribution International aging, and examples of early children’s literature to promote positive aging are pre- License (CC BY 4.0). sented. http://creativecommons.org/licenses/by/4.0/ Open Access Keywords Aging, Aging Education, Ageism, Positive Aging, Early Children’s Literature, Book Award for Best Children’s Literature on Aging 1. Introduction There is a universality to aging; we are all doing it! Today’s children will be the older adults of tomorrow. -

Review of UK Hate Crime Law to Consider Misogyny and Ageism Misandry and Prejudice Against Goths Could Also Be Added to Legislation
Review of UK hate crime law to consider misogyny and ageism Misandry and prejudice against goths could also be added to legislation Jamie Grierson Home affairs correspondent Tue 16 Oct 2018 00.01 BST Goths, men, women and elderly people could receive protection under hate crime laws after officials announced a wide-ranging review of current legislation. The Law Commission, the independent body that recommends legal reforms, will look at whether there are any gaps in hate crime legislation as part of a package of measures announced by the Home Office on Tuesday. Both misogyny (prejudice against women) and misandry (prejudice against men) will be considered by the review, as will attitudes towards alternative lifestyles such as goth subculture, and age. Race, religion, trans identity, sexual orientation and disability are the so-called “protected characteristics” covered by current legislation. The home secretary, Sajid Javid, said: “Hate crime goes directly against the longstanding British values of unity, tolerance and mutual respect, and I am committed to stamping this sickening behaviour out. Our refreshed action plan sets out how we will tackle the root causes of prejudice and racism, support hate crime victims and ensure offenders face the full force of the law.” There have been growing calls for misogyny to be treated as a hate crime, and for street harassment of women to be recognised as a specific offence. Other measures announced by the Home Office include extending its places of worship scheme, which provides funding for protective security measures to religious institutions vulnerable to attack, from three to four years. -

Violence Against Older Women
HelpAge discussion paper November 2017 Violence against older women Contents Key messages 1 Introduction • Older women are frequently subjected to one or more forms of violence, abuse 2 Violence, abuse and and neglect based on their age, gender and other characteristics. This can neglect of older women be driven by ageism, sexism, the intersection of different characteristics or as a result of accumulated discrimination across their life course. 3 Gaps in data, policy and response • Violence against older women is not adequately addressed in the majority of research, policy and programmes to prevent and address violence against 3 The right to freedom women and girls. from violence, abuse and neglect • International, regional and national legal frameworks fail to adequately 4 Recommendations address the violence, abuse and neglect to which older women are subjected. Introduction “Women have often faced a lifetime of coercion, bullying and violence. In older age, women are often afraid to talk about what has happened to them and have learnt to accept this ‘silent’ form of punishment.” Woman, 61, UK Older women may be subjected to violence, abuse and neglect due to a number of factors, including but not limited to their age, gender, disability, place of origin, marital status, class or sexual orientation. Commitments under the Sustainable Development Goal 5 to “achieve gender equality and empower all women and girls” saw a removal of an upper age cap from indicators on violence against women and girls. Yet women over 49 remain routinely ignored in data collection, despite accounting for nearly a quarter of the world’s female population.1 This discussion paper aims to highlight the types of violence, abuse and neglect older women experience; and offers recommendations for a collaborative approach to close the data, policy and programme gaps that prevent women living lives free from violence, including in older age.