Montreal Protocol on Substances That Deplete the Ozone Layer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Medication Coverage Policy
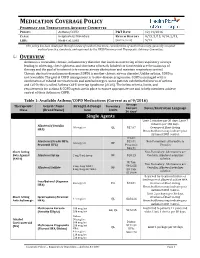
MEDICATION COVERAGE POLICY PHARMACY AND THERAPEUTICS ADVISORY COMMITTEE POLICY: Asthma/COPD P&T DATE 12/14/2016 CLASS: Respiratory Disorders REVIEW HISTORY 9/15, 5/15, 9/14, 2/13, LOB: Medi-Cal, SJHA (MONTH/YEAR) 5/12 This policy has been developed through review of medical literature, consideration of medical necessity, generally accepted medical practice standards, and approved by the HPSJ Pharmacy and Therapeutic Advisory Committee. OVERVIEW Asthma is a reversible, chronic, inflammatory disorder that involves narrowing of the respiratory airways leading to wheezing, chest tightness, and shortness of breath. Inhaled corticosteroids are the mainstay of therapy and the goal of treatment is to reverse airway obstruction and maintain respiratory control. Chronic obstructive pulmonary disease (COPD) is another chronic airway disorder. Unlike asthma, COPD is not reversible. The goal of COPD management is to slow disease progression. COPD is managed with a combination of inhaled corticosteroids and anticholinergics. Some patients exhibit both features of asthma and COPD; this is called Asthma-COPD Overlap Syndrome (ACOS). The below criteria, limits, and requirements for asthma & COPD agents are in place to ensure appropriate use and to help members achieve control of their Asthma or COPD. Table 1: Available Asthma/COPD Medications (Current as of 9/2016) Average Therapeutic Generic Name Strength & Dosage Formulary Cost per Limits Notes/Restriction Language Class (Brand Name) form 30 days* Single Agents Limit 2 inhalers per 30 days; Limit 7 -

Clinical Guideline for the Diagnosis, Evaluation and Management of Adults and Children with Asthma
Clinical Guideline for the Diagnosis, Evaluation and Management of Adults and Children with Asthma Color Key n Four Components of Asthma Care n Classifying Asthma Severity, Assessing Asthma Control and the Stepwise Approach for Managing Asthma in Children Aged 0– 4 years n Classifying Asthma Severity, Assessing Asthma Control and the Stepwise Approach for Managing Asthma in Children Aged 5–11 years n Classifying Asthma Severity, Assessing Asthma Control and the Stepwise Approach for Managing Asthma in Children >12 Years of Age & Adults n Long-Term Control Medications: Estimated Comparative Daily Dosages n Long-Term Control Medications: Usual Dosages n Quick-Relief Medications Guidelines are intended to be flexible. They serve as recommendations, not rigid criteria. Guidelines should be followed in most cases, but depending on the patient, and the circumstances, guidelines may need to be tailored to fit individual needs. 4750 11/18 Contents Criteria that suggest the diagnosis of asthma . 3 Goal of Therapy: Control of Asthma . 3 Four Components of Asthma Care 1. Assessment and Monitoring of Asthma Severity and Control . 4 2. Education for a Partnership in Care . 5 3. Control of Environmental Factors and Co-morbid Conditions that Affect Asthma . 5 4. Medications . 6 Bibliography . 6 Classifying Asthma Severity & Initiating Treatment in Children 0– 4 Years of Age . 7 Assessing Asthma Control & Adjusting Therapy in Children 0– 4 Years of Age . 7 Stepwise Approach for Managing Asthma in Children 0– 4 Years of Age . 8 Classifying Asthma Severity & Initiating Treatment in Children 5–11 Years of Age . 9 Assessing Asthma Control & Adjusting Therapy in Children 5–11 Years of Age . -
Comparison of Effect of Leukotriene Biosynthesis Blockers and Inhibitors of Phosphodiesterase Enzyme in Patients with Bronchial Hyperreactivity
ID Design Press, Skopje, Republic of Macedonia Open Access Macedonian Journal of Medical Sciences. 2018 May 20; 6(5):777-781. https://doi.org/10.3889/oamjms.2018.187 eISSN: 1857-9655 Clinical Science Comparison of Effect of Leukotriene Biosynthesis Blockers and Inhibitors of Phosphodiesterase Enzyme in Patients with Bronchial Hyperreactivity Naim Morina1, Arsim Haliti1, Ali Iljazi2, Drita Islami3, Sadi Bexheti4, Adnan Bozalija1*, Hilmi Islami3 1Department of Pharmacy, Faculty of Medicine, University of Prishtina, Prishtina, Kosovo; 2Kosovo Occupational Health Institute, Gjakovo, Kosovo; 3Department of Pharmacology, Faculty of Medicine, University of Prishtina, Kosovo; 4Department of Anatomy, Faculty of Medicine, University of Prishtina, Kosovo Abstract Citation: Morina N, Haliti A, Iljazi A, Islami D, Bexheti S, AIM: Blocking effect of leukotriene biosynthesis–zileuton and blocking the effect of phosphodiesterase enzyme– Bozalija A, Islami H. Comparison of Effect of Leukotriene diprophylline in the treatment of patients with bronchial asthma and bronchial increased reactivity, and tiotropium Biosynthesis Blockers and Inhibitors of Phosphodiesterase Enzyme in Patients with Bronchial bromide as an antagonist of the muscarinic receptor studied in this work. Hyperreactivity. Open Access Maced J Med Sci. 2018 May 20; 6(5):777-781. METHODS: Parameters of the lung function are determined with Body plethysmography. The resistance of the https://doi.org/10.3889/oamjms.2018.187 airways (Raw) was registered and measured was intrathoracic gas volume (ITGV), and specific resistance Keywords: Bronchial asthma; Zileuton; Diprophylline and tiotropium bromide (SRaw) was also calculated. For the research, administered was zileuton (tabl. 600 mg) and diprophylline (tabl. 150 mg). *Correspondence: Adnan Bozalija. Department of Pharmacy, Faculty of Medicine, University of Prishtina, Prishtina, Kosovo. -

FDA Briefing Document Pulmonary-Allergy Drugs Advisory Committee Meeting
FDA Briefing Document Pulmonary-Allergy Drugs Advisory Committee Meeting August 31, 2020 sNDA 209482: fluticasone furoate/umeclidinium/vilanterol fixed dose combination to reduce all-cause mortality in patients with chronic obstructive pulmonary disease NDA209482/S-0008 PADAC Clinical and Statistical Briefing Document Fluticasone furoate/umeclidinium/vilanterol fixed dose combination for all-cause mortality DISCLAIMER STATEMENT The attached package contains background information prepared by the Food and Drug Administration (FDA) for the panel members of the advisory committee. The FDA background package often contains assessments and/or conclusions and recommendations written by individual FDA reviewers. Such conclusions and recommendations do not necessarily represent the final position of the individual reviewers, nor do they necessarily represent the final position of the Review Division or Office. We have brought the supplemental New Drug Application (sNDA) 209482, for fluticasone furoate/umeclidinium/vilanterol, as an inhaled fixed dose combination, for the reduction in all-cause mortality in patients with COPD, to this Advisory Committee in order to gain the Committee’s insights and opinions, and the background package may not include all issues relevant to the final regulatory recommendation and instead is intended to focus on issues identified by the Agency for discussion by the advisory committee. The FDA will not issue a final determination on the issues at hand until input from the advisory committee process has been considered -

Intracolonic Administration of Zileuton, a Selective 5-Lipoxygenase Inhibitor, Accelerates Healing in a Rat Model of Chronic Colitis
Gut 1996; 38: 899-904 899 Intracolonic administration of zileuton, a selective 5-lipoxygenase inhibitor, accelerates healing in a rat model of chronic colitis Gut: first published as 10.1136/gut.38.6.899 on 1 June 1996. Downloaded from X Bertran, J Mafe', F Fernandez-Bafiares, E Castella, R Bartoli, I Ojanguren, M Esteve, M A Gassull Abstract models of colitis that the concentration of Background-5-Lipoxygenase products leukotrienes (mainly leukotriene B4 (LTB4)) in play a part in inflammatory response. the inflamed mucosa is within the range known Aims-The effect of intracolonic admini- to induce biological effects (chemokinesis, cell stration of zileuton (a 5-lipoxygenase aggregation, increasing of vascular permeabil- inhibitor) on colonic damage and ity), and these concentrations are similar to eicosanoid local release was assessed in a those seen in human IBD.2-7 In addition, rat model ofcolitis. drugs known to be effective in the treatment of Methods-Ninety rats with trinitroben- IBD are capable of reducing intestinal zenesulphonic acid induced colitis were leukotriene production in both experimental randomised to receive placebo, 5-amino- models of colitis and human IBD.36 On the salicylic acid (50 mglkg), or zileuton other hand, administration ofpotent and selec- (50 mg/kg) intracolonically for four weeks. tive inhibitors of leukotriene synthesis results Local eicosanoid release was monitored in a reduction of macroscopic and histological by intracolonic dialysis throughout the colonic damage in experimental colitis.6 8-11 study. The colon was removed for macro- Zileuton, N-(1-(benzo[b]thien-2-yl)ethyl)- scopic and histological assessment at N-hydroxyurea (Abbott Laboratories, Abbott weeks 1, 2, and 4 after colitis induction in Park, IL), is a drug that selectively inhibits the 10 rats of each group. -

Monteleucast and Zileuton Retard the Progression of Atherosclerosis Via Down Regulation of the Inflammatory and Oxidative Pathwa
& Experim l e ca n i t in a l l C C f a Journal of Clinical & Experimental Hadi et al., J Clin Exp Cardiolog 2013, 4:6 o r d l i a o DOI: 10.4172/2155-9880.1000250 n l o r g u y o J Cardiology ISSN: 2155-9880 Research Article Open Access Monteleucast and Zileuton Retard the Progression of Atherosclerosis via Down Regulation of the Inflammatory and Oxidative Pathways Najah R Hadi1*, Bassim I Mohammad2, Ahmad Almudhafer1, Naser Yousif3 and Ahmed M Sultan2 1Kufa College of Medicine, Iraq 2Al-Qadesiyah University, Iraq 3Colorado University, USA Abstract Background: Atherosclerosis and its thrombotic complications are responsible for remarkably high numbers of deaths. Leukotrines are involved in different stages of atherosclerosis. Therefore this study was undertaken to evaluate the effect of montelukast and zileuton on the progression of atherosclerosis. Materials and methods: Thirty-five male rabbits were used in this study. These animals randomized into 5 groups (7 rabbits each). Rabbits in first group were maintained on normal rabbit chow diet and used as normal diet control group (NC). While the rabbits in other four groups were fed on atherogenic diet (2% cholesterol) for 8 weeks. The second group, Atherogenic Control Group (AC) rabbits received atherogenic diet alone. Third group, Positive Control Group (PC) rabbits received atherogenic diet and ethanol as vehicle. Forth group, Montelukast Treated Group (MT) rabbits received montelukast 1.5 mg per kg daily and the fifth group, Zileuton Treated Group (ZT) rabbits received zileuton 150 mg per kg daily. At the end of 8th weeks animals were sacrificed, blood sample was collected to measure the following parameters: lipid profile, plasma GSH, MDA, and hsCRP. -

Leukotriene Modifiers (Accolate®, Singulair®, Zileuton®)
Leukotriene Modifiers (Accolate®, Singulair®, Zileuton®) What are They? Leukotriene modifiers reduce swelling and inflammation in the airways to prevent asthma symptoms. You may not notice a change in your asthma symptoms for one to two week, after starting to use them. • These medicines will not stop a sudden asthma attack. Albuterol should be used for sudden asthma attacks. • Only regular daily use of the leukotriene modifiers will prevent asthma symptoms. • It is important that you do not stop or decrease the dose of these medications without contacting your doctor. How should they be used? • Zafirlukast (Accolate®) is a tablet that is taken by mouth twice a day on an empty stomach (1 hour before you eat or 2 hours after you eat). It is very important to take this medicine on an empty stomach. o Zafirlukast must be taken every day even if you don’t have asthma symptoms. If you forget to take your dose on time, do not take twice as much the next time. Take the regularly scheduled dose as soon as you remember, then get back to your regular schedule. o Side effects . Zafirlukast (Accolate®) causes very few side effects. Some people may have headaches, nausea, or diarrhea. Although these side effects are quite uncommon, it is important for you to let your doctor know if you are experiencing any of these while taking zafirlukast. • Montelukast (Singulair®) o A tablet that is taken once a day at nighttime. o You can take Montelukast with or without food. o Montelukast must be taken every day even if you don’t have asthma symptoms. -

Zileuton for the Prophylaxis and Chronic Treatment of Asthma
Asthma Zileuton for the Prophylaxis and Chronic Treatment of Asthma a report by Bradley E Chipps, MD, FAAP, FAAAAI, FCCP Capital Allergy and Respiratory Disease Center Zileuton is the only commercially available leukotriene synthesis inhibitor pulmonary function, and will be able to lead a normal life, carrying on all approved for the prophylaxis and treatment of chronic asthma in adults activities desired.1 Risk refers to the potential for negative outcomes, which and adolescents aged 12 years and above. According to the updated and include symptom exacerbations and associated urgent care (i.e. comprehensive 2007 Expert Panel Report 3 (EPR3): Guidelines for the unscheduled office visits, emergency department visits, hospitalizations), as Diagnosis and Management of Asthma, zileuton is an alternative well as any adverse events associated with treatment.1 therapeutic option to be added to inhaled corticosteroids (ICS) to enhance asthma control for patients who remain uncontrolled despite According to the EPR3, patients who have more than one exacerbation of using recommended therapy.1 This article will examine the role of symptoms a year requiring a short course of oral corticosteroids (OCS) are zileuton in asthma management in relation to asthma control as an considered not well controlled.1 Between May 2006 and May 2007 almost unmet patient need. 1.7 million asthma patients received at least one prescription for OCS. This represented the largest single reason for OCS use in the US.4 What should Uncontrolled Asthma Remains an Unmet Need the physician do when the patient’s asthma remains uncontrolled despite Despite almost 20 years of global and national guidelines for managing optimal therapy? The EPR3 presents a revised step-care approach to therapy, asthma, and despite scientific contributions to understanding its with six steps, each accounting for a progressive drop in asthma control. -

Pharmacology and Therapeutics of Bronchodilators
1521-0081/12/6403-450–504$25.00 PHARMACOLOGICAL REVIEWS Vol. 64, No. 3 Copyright © 2012 by The American Society for Pharmacology and Experimental Therapeutics 4580/3762238 Pharmacol Rev 64:450–504, 2012 ASSOCIATE EDITOR: DAVID R. SIBLEY Pharmacology and Therapeutics of Bronchodilators Mario Cazzola, Clive P. Page, Luigino Calzetta, and M. Gabriella Matera Department of Internal Medicine, Unit of Respiratory Clinical Pharmacology, University of Rome ‘Tor Vergata,’ Rome, Italy (M.C., L.C.); Department of Pulmonary Rehabilitation, San Raffaele Pisana Hospital, Istituto di Ricovero e Cura a Carattere Scientifico, Rome, Italy (M.C., L.C.); Sackler Institute of Pulmonary Pharmacology, Institute of Pharmaceutical Science, King’s College London, London, UK (C.P.P., L.C.); and Department of Experimental Medicine, Unit of Pharmacology, Second University of Naples, Naples, Italy (M.G.M.) Abstract............................................................................... 451 I. Introduction: the physiological rationale for using bronchodilators .......................... 452 II. -Adrenergic receptor agonists .......................................................... 455 A. A history of the development of -adrenergic receptor agonists: from nonselective  Downloaded from adrenergic receptor agonists to 2-adrenergic receptor-selective drugs.................... 455  B. Short-acting 2-adrenergic receptor agonists........................................... 457 1. Albuterol........................................................................ 457 -

COPD/Asthma Class Update
Drug Use Research & Management Program Oregon State University, 500 Summer Street NE, E35, Salem, Oregon 97301-1079 Phone 503-947-5220 | Fax 503-947-1119 © Copyright 2012 Oregon State University. All Rights Reserved Class Update: Asthma/COPD Medications Month/Year of Review: July 2014 Last Oregon Review: May 2012/November 2013 PDL Classes: Asthma Controller, Asthma Rescue, COPD Source Documents: OSU College of Pharmacy New drug(s): Anoro® Ellipta® (umeclidinium/vilanterol) Manufacturer: GSK/Theravance Dossier Received: Yes Current Status of PDL Classes: Chronic Obstructive Pulmonary Disease (COPD): Preferred Agents: IPRATROPIUM BROMIDE HFA AER AD, IPRATROPIUM BROMIDE SOLUTION, IPRATROPIUM/ALBUTEROL SULFATE AMPUL-NEB, TIOTROPIUM BROMIDE(SPIRIVA®) CAP W/DEV, IPRATROPIUM/ALBUTEROL (COMBIVENT®) RESPIMAT Non-Preferred Agents: AFORMOTEROL (BROVANA®), FORMOTEROL (PERFOROMIST), ROFLUMILAST (DALIRESP®), INDACATEROL (ARCAPTA®) NEOHALER, ACLIDINIUM (TUDORZA®) PRESSAIR, VILANTEROL/FLUTICASONE (BREO®) ELLIPTA Asthma Controllers and Asthma Rescue Preferred Agents: BECLOMETHASONE DIPROPIONATE(QVAR®), BUDESONIDE (PULMICORT FLEXHALER®), BUDESONIDE / FORMOTEROL FUMARATE (SYMBICORT®), FLUTICASONE PROPIONATE(FLOVENT HFA®), FLUTICASONE PROPIONATE(FLOVENT DISKUS®), FLUTICASONE/SALMETEROL(ADVAIR DISKUS®), FLUTICASONE/SALMETEROL(ADVAIR HFA®), FORMOTEROL (FORADIL®) AEROLIZER, MONTELUKAST SODIUM TAB CHEW/TABLET, SALMETEROL XINAFOATE (SEREVENT®), ALBUTEROL SULFATE SOLUTION/VIAL NEBS, PIRBUTEROL ACETATE, PROAIR® HFA, VENTOLIN® HFA Non-preferred Agents: CICLESONIDE -

Antileukotriene Agents in Asthma: the Dart That Kills the Elephant?
Antileukotriene agents in asthma: The dart that kills the elephant? Education Paolo M. Renzi, MD Éducation Abstract From the Research Centre and the Pulmonary Unit, THE PERSISTENCE OF AIRWAY INFLAMMATION is believed to cause the mechanical Centre hospitalier de changes and symptoms of asthma. After decades of research, a new class of med- l’Université de Montréal ication has emerged that focuses on leukotrienes, mediators of inflammation. These Hospitals, Université de substances are potent inducers of bronchoconstriction, increased vascular perme- Montréal, and the Meakins ability and mucus production, and they potentiate the influx of inflammatory cells Christie Laboratories, McGill in the airways of patients with asthma. In this article the author reviews the devel- University, Montreal, Que. opment, mechanism of action, and clinical and toxic effects of the leukotriene syn- thesis inhibitors and receptor antagonists that are entering the North American market. These agents can decrease airway response to antigen, airway hyperre- This article has been peer reviewed. sponsiveness and exercise-induced asthma. They are also effective inhibitors of ASA-induced symptoms. Although few published studies are available, the an- CMAJ 1999;160:217-23 tileukotrienes seem almost as effective in the management of chronic asthma as ß See related article page 209 low-dose inhaled corticosteroids, and their use permits a decrease in the frequency of use or dose of corticosteroids. Further evaluation and clinical experience will determine the position of targeted inhibition of the leukotriene pathway in the treatment of asthma. Résumé ON CROIT QUE LA PERSISTANCE DE L’INFLAMMATION des voies respiratoires provoque les changements mécaniques et les symptômes de l’asthme. -

Pranlukast, a Novel Leukotriene Receptor Antagonist 525
Thorax 1997;52:523±527 523 Pranlukast, a novel leukotriene receptor Thorax: first published as 10.1136/thx.52.6.523 on 1 June 1997. Downloaded from antagonist: results of the ®rst European, placebo controlled, multicentre clinical study in asthma N C Barnes, J-C Pujet on behalf of an International Study Group Abstract asthma. It increased FEV1 within one hour Background ± Leukotriene receptor ant- of dosing, improved patient summary agonists have been shown to protect symptom and night-time asthma scores, against bronchoconstriction induced by and reduced the use of rescue broncho- antigens, exercise, and cold air. There are dilators, thus providing further evidence relatively few clinical studies reported in of a role for leukotrienes in the patho- patients with asthma. The present study genesis of asthma. is the ®rst clinical evaluation of pranlukast (Thorax 1997;52:523±527) (SB 205312, ONO-1078) outside Japan in patients with asthma. Keywords: leukotriene receptor antagonist, asthma, Methods ± A randomised, double blind, pranlukast, SB 205312, ONO-1078. placebo controlled, parallel group, multi- centre four week study of the safety and tolerability of oral pranlukast, 225 or Since the structure of leukotrienes was de- 337.5 mg twice daily, was performed in scribed in 1979,1 considerable eVort has been patients with mild to moderate asthma. made to develop drugs that block the leuko- Preliminary eYcacy data were obtained; triene receptor or inhibit synthesis of leuko- the main eYcacy variables evaluated were trienes. Challenge studies using a number forced expiratory volume in one second of leukotriene receptor antagonists or 5-lip- http://thorax.bmj.com/ (FEV1) and morning domiciliary (home) oxygenase inhibitors have shown that leuko- peak expiratory ¯ow rates (PEFR).