Therapeutic Class Overview Leukotriene Modifiers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Role of 15-Lipoxygenase/15-Hydroxyeicosatetraenoic Acid in Hypoxia-Induced Pulmonary Hypertension
J Physiol Sci (2012) 62:163–172 DOI 10.1007/s12576-012-0196-9 REVIEW Role of 15-lipoxygenase/15-hydroxyeicosatetraenoic acid in hypoxia-induced pulmonary hypertension Daling Zhu • Yajuan Ran Received: 29 September 2011 / Accepted: 25 January 2012 / Published online: 14 February 2012 Ó The Physiological Society of Japan and Springer 2012 Abstract Pulmonary arterial hypertension (PAH) is a Introduction rare disease with a complex aetiology characterized by elevated pulmonary artery resistance, which leads to right Pulmonary hypertension (PH) is a severe and frequently heart ventricular afterload and ultimately progressing to fatal disease characterized by elevated mean pulmonary right ventricular failure and often death. In addition to arterial (PA) pressure greater than 25 mmHg at rest or other factors, metabolites of arachidonic acid cascade play greater than 30 mmHg with exercise [1], and which con- an important role in the pulmonary vasculature, and dis- tributes to the morbidity and mortality of adult and pedi- ruption of signaling pathways of arachidonic acid plays a atric patients with various lung and heart diseases. central role in the pathogenesis of PAH. 15-Lipoxygenase According to the Venice Classification of Pulmonary (15-LO) is upregulated in pulmonary artery endothelial Hypertension in 2003, PH is currently classified into five cells and smooth muscle cells of PAH patients, and its categories as listed in Table 1. Importantly, many of these metabolite 15-hydroxyeicosatetraenoic acid (15-HETE) in diseases or conditions are associated with persistent or particular seems to play a central role in the contractile intermittent hypoxia, either globally or regionally, within machinery, and in the initiation and propagation of cell confined areas of the lung [2]. -

Inhibitory Activity of Pranlukast and Montelukas Against Histamine
Showa Univ J Med Sci 21(2), 77~84, June 2009 Original Inhibitory Activity of Pranlukast and Montelukas Against Histamine Release and LTC4 Production from Human Basophils 1, 2 1 1 Satoshi HIBINO ), Ryoko ITO ), Taeru KITABAYASHI ), 1 2 Kazuo ITAHASHI ) and Toshio NAKADATE ) Abstract : Leukotriene receptor antagonists(LTRAs)are routinely used to treat bronchial asthma and are thought to act mostly by inhibiting leukotriene receptors. However, there is no preclinical or clinical evidence of the direct effect of LTRAs on histamine release from and leukotriene(LT)C4 produc- tion by basophils. We used anti-IgE antibody(Ab), FMLP, and C5a to induce histamine release, and anti-IgE Ab and FMLP to stimulate LTC 4 production. Basophils were exposed to different concentrations of pranlukast and montelu- kast, and then to anti-IgE Ab, FMLP, and C5a. Culture supernatant histamine and LTC 4 levels were measured by using a histamine ELISA kit and a LTC 4 EIA kit, respectively. Histamine release was expressed as a percentage of the total histamine content(%HR)induced by anti-IgE Ab, FMLP, or C5a. To evaluate the effects of pranlukast and montelukast on histamine release and LTC 4 production, we calculated the percent inhibition of histamine release and LTC 4 production, expressed as percent inhibition, at different concentrations of pranlukast and montelukast. Pranlukast significantly inhibited histamine release stimulated by FMLP and C5a, but had no effect on histamine release stimulated by anti-IgE Ab. By comparison, montelukast signicantly inhibited histamine release stimulated by FMLP, C5a, and anti-IgE Ab, in a concentration-dependent manner. Both pranlukast and montelukast signicantly inhibited LTC 4 production stimulated by anti-IgE Ab and FMLP. -

Eicosanoids in Carcinogenesis
4open 2019, 2,9 © B.L.D.M. Brücher and I.S. Jamall, Published by EDP Sciences 2019 https://doi.org/10.1051/fopen/2018008 Special issue: Disruption of homeostasis-induced signaling and crosstalk in the carcinogenesis paradigm “Epistemology of the origin of cancer” Available online at: Guest Editor: Obul R. Bandapalli www.4open-sciences.org REVIEW ARTICLE Eicosanoids in carcinogenesis Björn L.D.M. Brücher1,2,3,*, Ijaz S. Jamall1,2,4 1 Theodor-Billroth-Academy®, Germany, USA 2 INCORE, International Consortium of Research Excellence of the Theodor-Billroth-Academy®, Germany, USA 3 Department of Surgery, Carl-Thiem-Klinikum, Cottbus, Germany 4 Risk-Based Decisions Inc., Sacramento, CA, USA Received 21 March 2018, Accepted 16 December 2018 Abstract- - Inflammation is the body’s reaction to pathogenic (biological or chemical) stimuli and covers a burgeoning list of compounds and pathways that act in concert to maintain the health of the organism. Eicosanoids and related fatty acid derivatives can be formed from arachidonic acid and other polyenoic fatty acids via the cyclooxygenase and lipoxygenase pathways generating a variety of pro- and anti-inflammatory mediators, such as prostaglandins, leukotrienes, lipoxins, resolvins and others. The cytochrome P450 pathway leads to the formation of hydroxy fatty acids, such as 20-hydroxyeicosatetraenoic acid, and epoxy eicosanoids. Free radical reactions induced by reactive oxygen and/or nitrogen free radical species lead to oxygenated lipids such as isoprostanes or isolevuglandins which also exhibit pro-inflammatory activities. Eicosanoids and their metabolites play fundamental endocrine, autocrine and paracrine roles in both physiological and pathological signaling in various diseases. These molecules induce various unsaturated fatty acid dependent signaling pathways that influence crosstalk, alter cell–cell interactions, and result in a wide spectrum of cellular dysfunctions including those of the tissue microenvironment. -
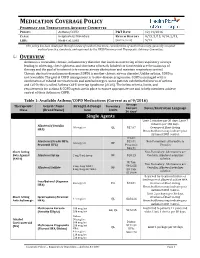
Medication Coverage Policy
MEDICATION COVERAGE POLICY PHARMACY AND THERAPEUTICS ADVISORY COMMITTEE POLICY: Asthma/COPD P&T DATE 12/14/2016 CLASS: Respiratory Disorders REVIEW HISTORY 9/15, 5/15, 9/14, 2/13, LOB: Medi-Cal, SJHA (MONTH/YEAR) 5/12 This policy has been developed through review of medical literature, consideration of medical necessity, generally accepted medical practice standards, and approved by the HPSJ Pharmacy and Therapeutic Advisory Committee. OVERVIEW Asthma is a reversible, chronic, inflammatory disorder that involves narrowing of the respiratory airways leading to wheezing, chest tightness, and shortness of breath. Inhaled corticosteroids are the mainstay of therapy and the goal of treatment is to reverse airway obstruction and maintain respiratory control. Chronic obstructive pulmonary disease (COPD) is another chronic airway disorder. Unlike asthma, COPD is not reversible. The goal of COPD management is to slow disease progression. COPD is managed with a combination of inhaled corticosteroids and anticholinergics. Some patients exhibit both features of asthma and COPD; this is called Asthma-COPD Overlap Syndrome (ACOS). The below criteria, limits, and requirements for asthma & COPD agents are in place to ensure appropriate use and to help members achieve control of their Asthma or COPD. Table 1: Available Asthma/COPD Medications (Current as of 9/2016) Average Therapeutic Generic Name Strength & Dosage Formulary Cost per Limits Notes/Restriction Language Class (Brand Name) form 30 days* Single Agents Limit 2 inhalers per 30 days; Limit 7 -

Clinical Guideline for the Diagnosis, Evaluation and Management of Adults and Children with Asthma
Clinical Guideline for the Diagnosis, Evaluation and Management of Adults and Children with Asthma Color Key n Four Components of Asthma Care n Classifying Asthma Severity, Assessing Asthma Control and the Stepwise Approach for Managing Asthma in Children Aged 0– 4 years n Classifying Asthma Severity, Assessing Asthma Control and the Stepwise Approach for Managing Asthma in Children Aged 5–11 years n Classifying Asthma Severity, Assessing Asthma Control and the Stepwise Approach for Managing Asthma in Children >12 Years of Age & Adults n Long-Term Control Medications: Estimated Comparative Daily Dosages n Long-Term Control Medications: Usual Dosages n Quick-Relief Medications Guidelines are intended to be flexible. They serve as recommendations, not rigid criteria. Guidelines should be followed in most cases, but depending on the patient, and the circumstances, guidelines may need to be tailored to fit individual needs. 4750 11/18 Contents Criteria that suggest the diagnosis of asthma . 3 Goal of Therapy: Control of Asthma . 3 Four Components of Asthma Care 1. Assessment and Monitoring of Asthma Severity and Control . 4 2. Education for a Partnership in Care . 5 3. Control of Environmental Factors and Co-morbid Conditions that Affect Asthma . 5 4. Medications . 6 Bibliography . 6 Classifying Asthma Severity & Initiating Treatment in Children 0– 4 Years of Age . 7 Assessing Asthma Control & Adjusting Therapy in Children 0– 4 Years of Age . 7 Stepwise Approach for Managing Asthma in Children 0– 4 Years of Age . 8 Classifying Asthma Severity & Initiating Treatment in Children 5–11 Years of Age . 9 Assessing Asthma Control & Adjusting Therapy in Children 5–11 Years of Age . -
Montreal Protocol on Substances That Deplete the Ozone Layer
MONTREAL PROTOCOL ON SUBSTANCES THAT DEPLETE THE OZONE LAYER UNEP 2006 REPORT OF THE MEDICAL TECHNICAL OPTIONS COMMITTEE 2006 ASSESSMENT UNEP 2006 REPORT OF THE MEDICAL TECHNICAL OPTIONS COMMITTEE 2006 ASSESSMENT 2006 MTOC Assessment Report iii Montreal Protocol On Substances that Deplete the Ozone Layer Report of the UNEP Medical Technical Options Committee 2006 Assessment ASSESSMENT REPORT The text of this report is composed in Times New Roman. Co-ordination: Medical Technical Options Committee Composition and layout: Helen Tope Reproduction: UNON Nairobi Date: January 2007 Under certain conditions, printed copies of this report are available from: UNITED NATIONS ENVIRONMENT PROGRAMME Ozone Secretariat, P.O. Box 30552, Nairobi, Kenya This document is also available in portable document format from the UNEP Ozone Secretariat's website: http://ozone.unep.org/Assessment_Panels/TEAP/Reports/MTOC/ No copyright involved. This publication may be freely copied, abstracted and cited, with acknowledgement of the source of the material. ISBN: 978-92-807-2828-6 Job No: OZO/0954/NA Cover photograph © Luo Hong. iv 2006 MTOC Assessment Report Disclaimer The United Nations Environment Programme (UNEP), the Technology and Economic Assessment Panel (TEAP) Co-chairs and members, the Technical Options Committees Co-chairs and members, the TEAP Task Forces Co-chairs and members, and the companies and organisations that employ them do not endorse the performance, worker safety, or environmental acceptability of any of the technical options discussed. Every industrial operation requires consideration of worker safety and proper disposal of contaminants and waste products. Moreover, as work continues - including additional toxicity evaluation - more information on health, environmental and safety effects of alternatives and replacements will become available for use in selecting among the options discussed in this document. -
Comparison of Effect of Leukotriene Biosynthesis Blockers and Inhibitors of Phosphodiesterase Enzyme in Patients with Bronchial Hyperreactivity
ID Design Press, Skopje, Republic of Macedonia Open Access Macedonian Journal of Medical Sciences. 2018 May 20; 6(5):777-781. https://doi.org/10.3889/oamjms.2018.187 eISSN: 1857-9655 Clinical Science Comparison of Effect of Leukotriene Biosynthesis Blockers and Inhibitors of Phosphodiesterase Enzyme in Patients with Bronchial Hyperreactivity Naim Morina1, Arsim Haliti1, Ali Iljazi2, Drita Islami3, Sadi Bexheti4, Adnan Bozalija1*, Hilmi Islami3 1Department of Pharmacy, Faculty of Medicine, University of Prishtina, Prishtina, Kosovo; 2Kosovo Occupational Health Institute, Gjakovo, Kosovo; 3Department of Pharmacology, Faculty of Medicine, University of Prishtina, Kosovo; 4Department of Anatomy, Faculty of Medicine, University of Prishtina, Kosovo Abstract Citation: Morina N, Haliti A, Iljazi A, Islami D, Bexheti S, AIM: Blocking effect of leukotriene biosynthesis–zileuton and blocking the effect of phosphodiesterase enzyme– Bozalija A, Islami H. Comparison of Effect of Leukotriene diprophylline in the treatment of patients with bronchial asthma and bronchial increased reactivity, and tiotropium Biosynthesis Blockers and Inhibitors of Phosphodiesterase Enzyme in Patients with Bronchial bromide as an antagonist of the muscarinic receptor studied in this work. Hyperreactivity. Open Access Maced J Med Sci. 2018 May 20; 6(5):777-781. METHODS: Parameters of the lung function are determined with Body plethysmography. The resistance of the https://doi.org/10.3889/oamjms.2018.187 airways (Raw) was registered and measured was intrathoracic gas volume (ITGV), and specific resistance Keywords: Bronchial asthma; Zileuton; Diprophylline and tiotropium bromide (SRaw) was also calculated. For the research, administered was zileuton (tabl. 600 mg) and diprophylline (tabl. 150 mg). *Correspondence: Adnan Bozalija. Department of Pharmacy, Faculty of Medicine, University of Prishtina, Prishtina, Kosovo. -

Montelukast Sodium) Tablets, Chewable Tablets, and Oral
Merck Sharp & Dohme Corp., a subsidiary of o MERCK & CO., INC. Whitehouse Station, NJ 08889/ USA HIGHLIGHTS OF PRESCRIBING INFORMATION .....................DOSAGE FORMS AND STRENGTHS..................... These highlights do not include all the information needed to use . SINGULAIR 10-mg Film-Coated Tablets SINGULAIR safely and effectively. See full prescribing information . SINGULAIR 5-mg and 4-mg Chewable Tablets for SINGULAIR. SINGULAIR 4.mg Oral Granules SINGULAIRiI .............................. CONTRAINDICATIONS .............................. (montelukast sodium) tablets, chewable tablets, and oral . Hypersensitivity to any component of this product (4). granules ....................... WARNINGS AND PRECAUTIONS ....................... Initial U.S. Approval: 1998 . Do not prescribe SINGULAIR to treat an acute asthma attack. .......................... RECENT MAJOR CHANGES........................... Advise patients to have appropriate rescue medication available Warnings and Precautions, Neuropsychiatric Events (5.4) 04/2010 (5.1). Inhaled corticosteroid may be reduced gradually. Do not abruptly ...........................INDICATIONS AND USAGE ........................... substitute SINGULAIR for inhaled or oral corticosteroids (5.2). SINGULAIRiI is a leukotriene receptor antagonist indicated for: . Patients with known aspirin sensitivity should continue to avoid . Prophylaxis and chronic treatment of asthma in patients aspirin or non-steroidal anti-inflammatory agents while taking 12 months of age and older (1.1). SINGULAIR (5.3). Acute prevention of exercise-induced bronchoconstriction (EIS) in Neuropsychiatric events have been reported with SINGULAIR. patients 15 years of age and older (1.2). Instruct patients to be alert for neuropsychiatric events. Evaluate Relief of symptoms of allergic rhinitis (AR): seasonal allergic the risks and benefits of continuing treatment with SINGULAIR if rhinitis (SAR) in patients 2 years of age and older, and perennial such events occur (5.4 and 6.2). -

Serum Leukotriene Metabolism and Type I Hypersensitivity Reactions in Different Animal Species
University of Montana ScholarWorks at University of Montana Graduate Student Theses, Dissertations, & Professional Papers Graduate School 1989 Serum leukotriene metabolism and Type I hypersensitivity reactions in different animal species Thulasi Sarojam Unnitan The University of Montana Follow this and additional works at: https://scholarworks.umt.edu/etd Let us know how access to this document benefits ou.y Recommended Citation Unnitan, Thulasi Sarojam, "Serum leukotriene metabolism and Type I hypersensitivity reactions in different animal species" (1989). Graduate Student Theses, Dissertations, & Professional Papers. 3533. https://scholarworks.umt.edu/etd/3533 This Thesis is brought to you for free and open access by the Graduate School at ScholarWorks at University of Montana. It has been accepted for inclusion in Graduate Student Theses, Dissertations, & Professional Papers by an authorized administrator of ScholarWorks at University of Montana. For more information, please contact [email protected]. Maureen and Mike MANSFIELD TJBRARY Copying allowed as provided under provisions of the Fair Use Section of the U.S. COPYRIGHT LAW, 1976. Any copying for commercial purposes or financial gain may be undertaken only with the author's written consent. MontanaUniversity of SERUM LEUKOTRIENE METABOLISM AND TYPE I HYPERSENSITIVITY REACTIONS IN DIFFERENT ANIMAL SPECIES By Thulasi Sarojam Unnithan M.B.B.S., Trivandrum Medical College, India, 1981 Presented in partial fulfillment of the requirements for the degree of Master of Science University of Montana, 1989 8^'an, Graduate School ($hL& . & Date UMI Number: EP34626 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent on the quality of the copy submitted. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. -

FDA Briefing Document Pulmonary-Allergy Drugs Advisory Committee Meeting
FDA Briefing Document Pulmonary-Allergy Drugs Advisory Committee Meeting August 31, 2020 sNDA 209482: fluticasone furoate/umeclidinium/vilanterol fixed dose combination to reduce all-cause mortality in patients with chronic obstructive pulmonary disease NDA209482/S-0008 PADAC Clinical and Statistical Briefing Document Fluticasone furoate/umeclidinium/vilanterol fixed dose combination for all-cause mortality DISCLAIMER STATEMENT The attached package contains background information prepared by the Food and Drug Administration (FDA) for the panel members of the advisory committee. The FDA background package often contains assessments and/or conclusions and recommendations written by individual FDA reviewers. Such conclusions and recommendations do not necessarily represent the final position of the individual reviewers, nor do they necessarily represent the final position of the Review Division or Office. We have brought the supplemental New Drug Application (sNDA) 209482, for fluticasone furoate/umeclidinium/vilanterol, as an inhaled fixed dose combination, for the reduction in all-cause mortality in patients with COPD, to this Advisory Committee in order to gain the Committee’s insights and opinions, and the background package may not include all issues relevant to the final regulatory recommendation and instead is intended to focus on issues identified by the Agency for discussion by the advisory committee. The FDA will not issue a final determination on the issues at hand until input from the advisory committee process has been considered -

Intracolonic Administration of Zileuton, a Selective 5-Lipoxygenase Inhibitor, Accelerates Healing in a Rat Model of Chronic Colitis
Gut 1996; 38: 899-904 899 Intracolonic administration of zileuton, a selective 5-lipoxygenase inhibitor, accelerates healing in a rat model of chronic colitis Gut: first published as 10.1136/gut.38.6.899 on 1 June 1996. Downloaded from X Bertran, J Mafe', F Fernandez-Bafiares, E Castella, R Bartoli, I Ojanguren, M Esteve, M A Gassull Abstract models of colitis that the concentration of Background-5-Lipoxygenase products leukotrienes (mainly leukotriene B4 (LTB4)) in play a part in inflammatory response. the inflamed mucosa is within the range known Aims-The effect of intracolonic admini- to induce biological effects (chemokinesis, cell stration of zileuton (a 5-lipoxygenase aggregation, increasing of vascular permeabil- inhibitor) on colonic damage and ity), and these concentrations are similar to eicosanoid local release was assessed in a those seen in human IBD.2-7 In addition, rat model ofcolitis. drugs known to be effective in the treatment of Methods-Ninety rats with trinitroben- IBD are capable of reducing intestinal zenesulphonic acid induced colitis were leukotriene production in both experimental randomised to receive placebo, 5-amino- models of colitis and human IBD.36 On the salicylic acid (50 mglkg), or zileuton other hand, administration ofpotent and selec- (50 mg/kg) intracolonically for four weeks. tive inhibitors of leukotriene synthesis results Local eicosanoid release was monitored in a reduction of macroscopic and histological by intracolonic dialysis throughout the colonic damage in experimental colitis.6 8-11 study. The colon was removed for macro- Zileuton, N-(1-(benzo[b]thien-2-yl)ethyl)- scopic and histological assessment at N-hydroxyurea (Abbott Laboratories, Abbott weeks 1, 2, and 4 after colitis induction in Park, IL), is a drug that selectively inhibits the 10 rats of each group. -

Ioi70902.Pdf
ORIGINAL INVESTIGATION Montelukast, a Once-Daily Leukotriene Receptor Antagonist, in the Treatment of Chronic Asthma A Multicenter, Randomized, Double-blind Trial Theodore F. Reiss, MD; Paul Chervinsky, MD; Robert J. Dockhorn, MD; Sumiko Shingo, MS; Beth Seidenberg, MD; Thomas B. Edwards, MD; for the Montelukast Clinical Research Study Group Objectives: To determine the clinical effect of oral mon- Results: Montelukast improved airway obstruction telukast sodium, a leukotriene receptor antagonist, in asth- (forced expiratory volume in 1 second, morning and matic patients aged 15 years or more. evening peak expiratory flow rate) and patient-reported end points (daytime asthma symptoms, “as-needed” Design: Randomized, multicenter, double-blind, placebo- b-agonist use, nocturnal awakenings) (P,.001 com- controlled, parallel-group study. A 2-week, single- pared with placebo). Montelukast provided near- blind, placebo run-in period was followed by a 12- maximal effect in these end points within the first day week, double-blind treatment period (montelukast of treatment. Tolerance and rebound worsening of asthma sodium, 10 mg, or matching placebo, once daily at bed- did not occur. Montelukast improved outcome end points, time) and a 3-week, double-blind, washout period. including asthma exacerbations, asthma control days (P,.001 compared with placebo), and decreased periph- Setting/Patients: Fifty clinical centers randomly allo- eral blood eosinophil counts (P,.001 compared with pla- cated 681 patients with chronic, stable asthma to receive pla- cebo). The incidence of adverse events and discontinu- cebo or montelukast after demonstrating a forced expira- ations from therapy were similar in the montelukast and tory volume in 1 second 50% to 85% of the predicted value, placebo groups.