Strict Regio-Specificity of Human Epithelial 15-Lipoxygenase-2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Role of 15-Lipoxygenase/15-Hydroxyeicosatetraenoic Acid in Hypoxia-Induced Pulmonary Hypertension
J Physiol Sci (2012) 62:163–172 DOI 10.1007/s12576-012-0196-9 REVIEW Role of 15-lipoxygenase/15-hydroxyeicosatetraenoic acid in hypoxia-induced pulmonary hypertension Daling Zhu • Yajuan Ran Received: 29 September 2011 / Accepted: 25 January 2012 / Published online: 14 February 2012 Ó The Physiological Society of Japan and Springer 2012 Abstract Pulmonary arterial hypertension (PAH) is a Introduction rare disease with a complex aetiology characterized by elevated pulmonary artery resistance, which leads to right Pulmonary hypertension (PH) is a severe and frequently heart ventricular afterload and ultimately progressing to fatal disease characterized by elevated mean pulmonary right ventricular failure and often death. In addition to arterial (PA) pressure greater than 25 mmHg at rest or other factors, metabolites of arachidonic acid cascade play greater than 30 mmHg with exercise [1], and which con- an important role in the pulmonary vasculature, and dis- tributes to the morbidity and mortality of adult and pedi- ruption of signaling pathways of arachidonic acid plays a atric patients with various lung and heart diseases. central role in the pathogenesis of PAH. 15-Lipoxygenase According to the Venice Classification of Pulmonary (15-LO) is upregulated in pulmonary artery endothelial Hypertension in 2003, PH is currently classified into five cells and smooth muscle cells of PAH patients, and its categories as listed in Table 1. Importantly, many of these metabolite 15-hydroxyeicosatetraenoic acid (15-HETE) in diseases or conditions are associated with persistent or particular seems to play a central role in the contractile intermittent hypoxia, either globally or regionally, within machinery, and in the initiation and propagation of cell confined areas of the lung [2]. -

Eicosanoids in Carcinogenesis
4open 2019, 2,9 © B.L.D.M. Brücher and I.S. Jamall, Published by EDP Sciences 2019 https://doi.org/10.1051/fopen/2018008 Special issue: Disruption of homeostasis-induced signaling and crosstalk in the carcinogenesis paradigm “Epistemology of the origin of cancer” Available online at: Guest Editor: Obul R. Bandapalli www.4open-sciences.org REVIEW ARTICLE Eicosanoids in carcinogenesis Björn L.D.M. Brücher1,2,3,*, Ijaz S. Jamall1,2,4 1 Theodor-Billroth-Academy®, Germany, USA 2 INCORE, International Consortium of Research Excellence of the Theodor-Billroth-Academy®, Germany, USA 3 Department of Surgery, Carl-Thiem-Klinikum, Cottbus, Germany 4 Risk-Based Decisions Inc., Sacramento, CA, USA Received 21 March 2018, Accepted 16 December 2018 Abstract- - Inflammation is the body’s reaction to pathogenic (biological or chemical) stimuli and covers a burgeoning list of compounds and pathways that act in concert to maintain the health of the organism. Eicosanoids and related fatty acid derivatives can be formed from arachidonic acid and other polyenoic fatty acids via the cyclooxygenase and lipoxygenase pathways generating a variety of pro- and anti-inflammatory mediators, such as prostaglandins, leukotrienes, lipoxins, resolvins and others. The cytochrome P450 pathway leads to the formation of hydroxy fatty acids, such as 20-hydroxyeicosatetraenoic acid, and epoxy eicosanoids. Free radical reactions induced by reactive oxygen and/or nitrogen free radical species lead to oxygenated lipids such as isoprostanes or isolevuglandins which also exhibit pro-inflammatory activities. Eicosanoids and their metabolites play fundamental endocrine, autocrine and paracrine roles in both physiological and pathological signaling in various diseases. These molecules induce various unsaturated fatty acid dependent signaling pathways that influence crosstalk, alter cell–cell interactions, and result in a wide spectrum of cellular dysfunctions including those of the tissue microenvironment. -

Leukotriene D4induced Caco2 Cell Proliferation Is Mediated By
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Diposit Digital de la Universitat de Barcelona Physiological Reports ISSN 2051-817X ORIGINAL RESEARCH Leukotriene D4-induced Caco-2 cell proliferation is mediated by prostaglandin E2 synthesis Marisol Cabral, Raquel Martın-Venegas & Juan J. Moreno Departament de Fisiologia, Facultat de Farmacia, Universitat de Barcelona, Barcelona, Spain Keywords Abstract 5-lipoxygenase, arachidonic acid cascade, cell cycle, cell growth, colon cancer. Leukotriene D4 (LTD4) is a pro-inflammatory mediator formed from arachi- donic acid through the action of 5-lipoxygenase (5-LOX). Its biological effects Correspondence are mediated by at least two G-coupled plasmatic cysteinyl LT receptors (Cys- Juan Jose Moreno, Departament de LT1-2R). It has been reported an upregulation of the 5-LOX pathway in tumor Fisiologia, Facultat de Farmacia, Universitat tissue unlike in normal colon mucosa. Colon tumors generally have an de Barcelona, Avda. Joan XXIII s/n, 08028 increased expression of CysLT1R and colon cancer patients with high expres- Barcelona, Spain. sion levels of CysLT R have poor prognosis. We previously observed that the Tel: +34 93 402 4505 1 Fax: +34 93 403 5901 cyclooxygenase pathway is involved in the control of intestinal epithelial can- E-mail: [email protected] cer cell growth through PGE2 production. The aim of this study was therefore to assess the effect of LTD4 binding with CysLT1R on Caco-2 cell growth. We Funding Information note a number of key findings from this research. We observed that at a con- This research was supported by Spanish centration similar to that found under inflammatory conditions, LTD4 was Ministry of Science and Innovation (BFU2007- able to induce Caco-2 cell proliferation and DNA synthesis. -

Epigenetic Regulations of Ahr in the Aspect of Immunomodulation
International Journal of Molecular Sciences Review Epigenetic Regulations of AhR in the Aspect of Immunomodulation Anna Wajda 1,* , Joanna Łapczuk-Roma ´nska 2 and Agnieszka Paradowska-Gorycka 1 1 Department of Molecular Biology, National Institute of Geriatrics, Rheumatology and Rehabilitation, 02-637 Warsaw, Poland; [email protected] 2 Department of Experimental and Clinical Pharmacology, Pomeranian Medical University, 70-111 Szczecin, Poland; [email protected] * Correspondence: [email protected] Received: 31 July 2020; Accepted: 28 August 2020; Published: 3 September 2020 Abstract: Environmental factors contribute to autoimmune disease manifestation, and as regarded today, AhR has become an important factor in studies of immunomodulation. Besides immunological aspects, AhR also plays a role in pharmacological, toxicological and many other physiological processes such as adaptive metabolism. In recent years, epigenetic mechanisms have provided new insight into gene regulation and reveal a new contribution to autoimmune disease pathogenesis. DNA methylation, histone modifications, chromatin alterations, microRNA and consequently non-genetic changes in phenotypes connect with environmental factors. Increasing data reveals AhR cross-roads with the most significant in immunology pathways. Although study on epigenetic modulations in autoimmune diseases is still not well understood, therefore future research will help us understand their pathophysiology and help to find new therapeutic strategies. Present literature review -

Environmental Pollution 275 (2021) 116665
Environmental Pollution 275 (2021) 116665 Contents lists available at ScienceDirect Environmental Pollution journal homepage: www.elsevier.com/locate/envpol Metabolomics reveals the reproductive abnormality in female zebrafish exposed to environmentally relevant levels of climbazole* Ting Zou a, 1, Yan-Qiu Liang b, 1, Xiaoliang Liao a, Xiao-Fan Chen a, Tao Wang c, * Yuanyuan Song c, Zhi-Cheng Lin a, Zenghua Qi a, Zhi-Feng Chen a, d, , Zongwei Cai a, c a Guangdong Key Laboratory of Environmental Catalysis and Health Risk Control, School of Environmental Science and Engineering, Institute of Environmental Health and Pollution Control, Guangdong University of Technology, Guangzhou, 510006, China b Faculty of Chemistry and Environmental Science, Guangdong Ocean University, Zhanjiang, 524088, China c State Key Laboratory of Environmental and Biological Analysis, Department of Chemistry, Hong Kong Baptist University, Hong Kong Special Administrative Region, China d Guangdong Provincial Key Laboratory of Chemical Pollution and Environmental Safety, South China Normal University, Guangzhou, 510006, China article info abstract Article history: Climbazole (CBZ) ubiquitously detected in the aquatic environment may disrupt fish reproductive Received 15 November 2020 function. Thus far, the previous study has focused on its transcriptional impact of steroidogenesis-related Received in revised form genes on zebrafish, but the underlying toxic mechanism still needs further investigation at the metabolic 10 January 2021 level. In this study, adult zebrafish were chronically exposed to CBZ at concentrations of 0.1 (corre- Accepted 2 February 2021 sponding to the real concentration in surface water), 10, and 1000 mg/L and evaluated for reproductive Available online 5 February 2021 function by egg production, with subsequent ovarian tissue samples taken for histology, metabolomics, and other biochemical analysis. -
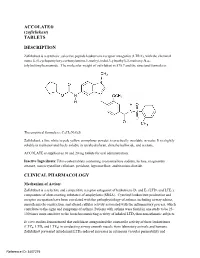
ACCOLATE® (Zafirlukast) TABLETS DESCRIPTION
ACCOLATE® (zafirlukast) TABLETS DESCRIPTION Zafirlukast is a synthetic, selective peptide leukotriene receptor antagonist (LTRA), with the chemical name 4-(5-cyclopentyloxy-carbonylamino-1-methyl-indol-3-ylmethyl)-3-methoxy-N-o tolylsulfonylbenzamide. The molecular weight of zafirlukast is 575.7 and the structural formula is: The empirical formula is: C31H33N3O6S Zafirlukast, a fine white to pale yellow amorphous powder, is practically insoluble in water. It is slightly soluble in methanol and freely soluble in tetrahydrofuran, dimethylsulfoxide, and acetone. ACCOLATE is supplied as 10 and 20 mg tablets for oral administration. Inactive Ingredients: Film-coated tablets containing croscarmellose sodium, lactose, magnesium stearate, microcrystalline cellulose, povidone, hypromellose, and titanium dioxide. CLINICAL PHARMACOLOGY Mechanism of Action: Zafirlukast is a selective and competitive receptor antagonist of leukotriene D4 and E4 (LTD4 and LTE4), components of slow-reacting substance of anaphylaxis (SRSA). Cysteinyl leukotriene production and receptor occupation have been correlated with the pathophysiology of asthma, including airway edema, smooth muscle constriction, and altered cellular activity associated with the inflammatory process, which contribute to the signs and symptoms of asthma. Patients with asthma were found in one study to be 25 100 times more sensitive to the bronchoconstricting activity of inhaled LTD4 than nonasthmatic subjects. In vitro studies demonstrated that zafirlukast antagonized the contractile activity of three leukotrienes (LTC4, LTD4 and LTE4) in conducting airway smooth muscle from laboratory animals and humans. Zafirlukast prevented intradermal LTD4-induced increases in cutaneous vascular permeability and Reference ID: 3407275 inhibited inhaled LTD4-induced influx of eosinophils into animal lungs. Inhalational challenge studies in sensitized sheep showed that zafirlukast suppressed the airway responses to antigen; this included both the early- and late-phase response and the nonspecific hyperresponsiveness. -

Role of Arachidonic Acid and Its Metabolites in the Biological and Clinical Manifestations of Idiopathic Nephrotic Syndrome
International Journal of Molecular Sciences Review Role of Arachidonic Acid and Its Metabolites in the Biological and Clinical Manifestations of Idiopathic Nephrotic Syndrome Stefano Turolo 1,* , Alberto Edefonti 1 , Alessandra Mazzocchi 2, Marie Louise Syren 2, William Morello 1, Carlo Agostoni 2,3 and Giovanni Montini 1,2 1 Fondazione IRCCS Ca’ Granda-Ospedale Maggiore Policlinico, Pediatric Nephrology, Dialysis and Transplant Unit, Via della Commenda 9, 20122 Milan, Italy; [email protected] (A.E.); [email protected] (W.M.); [email protected] (G.M.) 2 Department of Clinical Sciences and Community Health, University of Milan, 20122 Milan, Italy; [email protected] (A.M.); [email protected] (M.L.S.); [email protected] (C.A.) 3 Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Pediatric Intermediate Care Unit, 20122 Milan, Italy * Correspondence: [email protected] Abstract: Studies concerning the role of arachidonic acid (AA) and its metabolites in kidney disease are scarce, and this applies in particular to idiopathic nephrotic syndrome (INS). INS is one of the most frequent glomerular diseases in childhood; it is characterized by T-lymphocyte dysfunction, alterations of pro- and anti-coagulant factor levels, and increased platelet count and aggregation, leading to thrombophilia. AA and its metabolites are involved in several biological processes. Herein, Citation: Turolo, S.; Edefonti, A.; we describe the main fields where they may play a significant role, particularly as it pertains to their Mazzocchi, A.; Syren, M.L.; effects on the kidney and the mechanisms underlying INS. AA and its metabolites influence cell Morello, W.; Agostoni, C.; Montini, G. -

Lipoxin A4: a Novel Anti-Inflammatory Molecule? Thorax: First Published As 10.1136/Thx.50.2.111 on 1 February 1995
Thorax 1995;50:111-112 illl Lipoxin A4: a novel anti-inflammatory molecule? Thorax: first published as 10.1136/thx.50.2.111 on 1 February 1995. Downloaded from Arachidonic acid is metabolised by the cyclooxygenase contractions.22 These studies support the view that LXA4 pathway to the prostaglandins and thromboxane A2 or via may act as a partial agonist at the same or similar site as one of the lipoxygenase pathways.' Three major lip- the sulphidopeptide leukotrienes. oxygenase pathways have been identified in mammalian The fact that 1 5-lipoxygenase is abundant in lung tissue tissue - namely, the 5-, 12-, and 15-lipoxygenases.2A The and that LXA4 has been recovered in the bronchoalveolar 5-lipoxygenase pathway metabolises arachidonic acid lavage fluid ofpatients with asthma and other lung diseases through two intermediates, 5-hydroperoxyeicosatetranoic suggests that LXA4 may be a potential mediator or mod- acid (5-HPETE) and leukotriene A4 (LTA4), to LTB4 and ulator of inflammation in the lung. In a recent study eight the sulphidopeptide leukotrienes LTC4, LTD4, and LTE4.5 subjects underwent inhalation challenge with LXA4,23 but The sulphidopeptide leukotrienes are potent spasmogens6 no effect was seen on specific conductance, rate of airflow for non-vascular smooth muscle and may play a part in at 25% vital capacity (V25), blood pressure, pulse, or the pathogenesis of bronchial asthma.7`10 asthmatic symptoms. There was, however, a significant The interactions between 5-lipoxygenase and 15-lip- shift of the specific conductance and V25 dose-response oxygenase on arachidonic acid metabolism have recently curve to the right after inhalation challenge with LTC4 been studied and a new series of biologically active me- combined with LXA4 compared with that after inhalation tabolites described." 12 These molecules have been termed challenge with LTC4 alone. -

Montelukast, a Leukotriene Receptor Antagonist, Reduces the Concentration of Leukotrienes in the Respiratory Tract of Children with Persistent Asthma
Montelukast, a leukotriene receptor antagonist, reduces the concentration of leukotrienes in the respiratory tract of children with persistent asthma Benjamin Volovitz, MD,a,b Elvan Tabachnik, MD,c Moshe Nussinovitch, MD,b Biana Shtaif, MSc,b Hanna Blau, MD,a Irit Gil-Ad, PhD,b Abraham Weizman, MD,b and Itzhak Varsano, MDa,b Petah Tikva, Tel Aviv, and Rehovot, Israel Background: Leukotrienes are bronchoactive mediators secreted by inflammatory cells in the respiratory mucosa on Abbreviations used exposure to asthma triggers. BAL: Bronchoalveolar lavage Objective: We investigated the effect of montelukast, a CysLT1: Cysteinyl leukotriene 1 (receptor) leukotriene receptor antagonist, on the release of leukotrienes ECP: Eosinophilic cationic protein in the respiratory mucosa of children with persistent asthma. LTC4: Leukotriene C4 Method: Twenty-three children aged 6 to 11 years with moder- LTD4: Leukotriene D4 ately severe asthma were treated in a cross-over design start- LTE4: Leukotriene E4 ing, after a 2-week run in period, with either montelukast (n = 12) or cromolyn (n = 11) for 4 weeks with a 2-week washout period between treatments. Twelve of them were then treated Cysteinyl leukotrienes are potent proinflammatory with either montelukast or beclomethasone for 6 months. The mediators produced from a variety of inflammatory use of β -agonists was recorded on a diary card. The concen- 2 cells, including mast cells, eosinophils, basophils and tration of leukotriene C4 (LTC4) was measured by HPLC in nasal washes obtained before and at the end of each treatment macrophages. Leukotriene C4 (LTC4) is metabolized period. Eosinophilic cationic protein (ECP) was measured in enzymatically to leukotriene D4 (LTD4) and subsequent- the nasal washes by RIA. -

Serum Leukotriene Metabolism and Type I Hypersensitivity Reactions in Different Animal Species
University of Montana ScholarWorks at University of Montana Graduate Student Theses, Dissertations, & Professional Papers Graduate School 1989 Serum leukotriene metabolism and Type I hypersensitivity reactions in different animal species Thulasi Sarojam Unnitan The University of Montana Follow this and additional works at: https://scholarworks.umt.edu/etd Let us know how access to this document benefits ou.y Recommended Citation Unnitan, Thulasi Sarojam, "Serum leukotriene metabolism and Type I hypersensitivity reactions in different animal species" (1989). Graduate Student Theses, Dissertations, & Professional Papers. 3533. https://scholarworks.umt.edu/etd/3533 This Thesis is brought to you for free and open access by the Graduate School at ScholarWorks at University of Montana. It has been accepted for inclusion in Graduate Student Theses, Dissertations, & Professional Papers by an authorized administrator of ScholarWorks at University of Montana. For more information, please contact [email protected]. Maureen and Mike MANSFIELD TJBRARY Copying allowed as provided under provisions of the Fair Use Section of the U.S. COPYRIGHT LAW, 1976. Any copying for commercial purposes or financial gain may be undertaken only with the author's written consent. MontanaUniversity of SERUM LEUKOTRIENE METABOLISM AND TYPE I HYPERSENSITIVITY REACTIONS IN DIFFERENT ANIMAL SPECIES By Thulasi Sarojam Unnithan M.B.B.S., Trivandrum Medical College, India, 1981 Presented in partial fulfillment of the requirements for the degree of Master of Science University of Montana, 1989 8^'an, Graduate School ($hL& . & Date UMI Number: EP34626 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent on the quality of the copy submitted. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. -

Reduced 15-Lipoxygenase 2 and Lipoxin A4/Leukotriene B4 Ratio in Children with Cystic Fibrosis
ORIGINAL ARTICLE CYSTIC FIBROSIS Reduced 15-lipoxygenase 2 and lipoxin A4/leukotriene B4 ratio in children with cystic fibrosis Fiona C. Ringholz1, Paul J. Buchanan1, Donna T. Clarke1, Roisin G. Millar1, Michael McDermott2, Barry Linnane1,3,4, Brian J. Harvey5, Paul McNally1,2 and Valerie Urbach1,6 Affiliations: 1National Children’s Research Centre, Crumlin, Dublin, Ireland. 2Our Lady’s Children’s Hospital, Crumlin, Dublin, Ireland. 3Midwestern Regional Hospital, Limerick, Ireland. 4Centre for Interventions in Infection, Inflammation and Immunity (4i), Graduate Entry Medical School, University of Limerick, Limerick, Ireland. 5Molecular Medicine Laboratories, Royal College of Surgeons in Ireland, Beaumont Hospital, Dublin, Ireland. 6Institut National de la Sante´ et de la Recherche Me´dicale, U845, Faculte´ de Me´decine Paris Descartes, Paris, France. Correspondence: Valerie Urbach, National Children’s Research Centre, Crumlin, Dublin 12, Ireland. E-mail: [email protected] ABSTRACT Airway disease in cystic fibrosis (CF) is characterised by impaired mucociliary clearance, persistent bacterial infection and neutrophilic inflammation. Lipoxin A4 (LXA4) initiates the active resolution of inflammation and promotes airway surface hydration in CF models. 15-Lipoxygenase (LO) plays a central role in the ‘‘class switch’’ of eicosanoid mediator biosynthesis from leukotrienes to lipoxins, initiating the active resolution of inflammation. We hypothesised that defective eicosanoid mediator class switching contributes to the failure to resolve inflammation in CF lung disease. Using bronchoalveolar lavage (BAL) samples from 46 children with CF and 19 paediatric controls we demonstrate that the ratio of LXA4 to leukotriene B4 (LTB4) is depressed in CF BAL (p,0.01), even in the absence of infection (p,0.001). -

Ioi70902.Pdf
ORIGINAL INVESTIGATION Montelukast, a Once-Daily Leukotriene Receptor Antagonist, in the Treatment of Chronic Asthma A Multicenter, Randomized, Double-blind Trial Theodore F. Reiss, MD; Paul Chervinsky, MD; Robert J. Dockhorn, MD; Sumiko Shingo, MS; Beth Seidenberg, MD; Thomas B. Edwards, MD; for the Montelukast Clinical Research Study Group Objectives: To determine the clinical effect of oral mon- Results: Montelukast improved airway obstruction telukast sodium, a leukotriene receptor antagonist, in asth- (forced expiratory volume in 1 second, morning and matic patients aged 15 years or more. evening peak expiratory flow rate) and patient-reported end points (daytime asthma symptoms, “as-needed” Design: Randomized, multicenter, double-blind, placebo- b-agonist use, nocturnal awakenings) (P,.001 com- controlled, parallel-group study. A 2-week, single- pared with placebo). Montelukast provided near- blind, placebo run-in period was followed by a 12- maximal effect in these end points within the first day week, double-blind treatment period (montelukast of treatment. Tolerance and rebound worsening of asthma sodium, 10 mg, or matching placebo, once daily at bed- did not occur. Montelukast improved outcome end points, time) and a 3-week, double-blind, washout period. including asthma exacerbations, asthma control days (P,.001 compared with placebo), and decreased periph- Setting/Patients: Fifty clinical centers randomly allo- eral blood eosinophil counts (P,.001 compared with pla- cated 681 patients with chronic, stable asthma to receive pla- cebo). The incidence of adverse events and discontinu- cebo or montelukast after demonstrating a forced expira- ations from therapy were similar in the montelukast and tory volume in 1 second 50% to 85% of the predicted value, placebo groups.