2019 Texas FI PA Results Ready for Formatting 3-29-20
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-
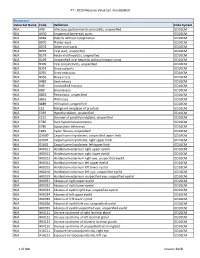
PT - 2020 Measure Value Set Avoidableed
PT - 2020 Measure Value Set_AvoidableED Numerator Value Set Name Code Definition Code System N/A A09 Infectious gastroenteritis and colitis, unspecified ICD10CM N/A A630 Anogenital (venereal) warts ICD10CM N/A B069 Rubella without complication ICD10CM N/A B070 Plantar wart ICD10CM N/A B078 Other viral warts ICD10CM N/A B079 Viral wart, unspecified ICD10CM N/A B179 Acute viral hepatitis, unspecified ICD10CM N/A B199 Unspecified viral hepatitis without hepatic coma ICD10CM N/A B309 Viral conjunctivitis, unspecified ICD10CM N/A B354 Tinea corporis ICD10CM N/A B355 Tinea imbricata ICD10CM N/A B356 Tinea cruris ICD10CM N/A B483 Geotrichosis ICD10CM N/A B49 Unspecified mycosis ICD10CM N/A B80 Enterobiasis ICD10CM N/A B852 Pediculosis, unspecified ICD10CM N/A B853 Phthiriasis ICD10CM N/A B889 Infestation, unspecified ICD10CM N/A C61 Malignant neoplasm of prostate ICD10CM N/A E039 Hypothyroidism, unspecified ICD10CM N/A E215 Disorder of parathyroid gland, unspecified ICD10CM N/A E780 Pure hypercholesterolemia ICD10CM N/A E786 Lipoprotein deficiency ICD10CM N/A E849 Cystic fibrosis, unspecified ICD10CM N/A G5600 Carpal tunnel syndrome, unspecified upper limb ICD10CM N/A G5601 Carpal tunnel syndrome, right upper limb ICD10CM N/A G5602 Carpal tunnel syndrome, left upper limb ICD10CM N/A H00011 Hordeolum externum right upper eyelid ICD10CM N/A H00012 Hordeolum externum right lower eyelid ICD10CM N/A H00013 Hordeolum externum right eye, unspecified eyelid ICD10CM N/A H00014 Hordeolum externum left upper eyelid ICD10CM N/A H00015 Hordeolum externum -
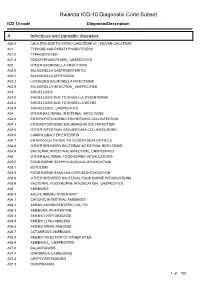
Rwanda ICD-10 Diagnostic Code Subset
Rwanda ICD-10 Diagnostic Code Subset ICD 10 code Diagnosis/Description A Infectious and parasitic diseases A00.0 CHOLERA DUE TO VIBRIO CHOLERAE 01_ BIOVAR CHOLERAE A01 TYPHOID AND PARATYPHOID FEVERS A01.0 TYPHOID FEVER A01.4 PARATYPHOID FEVER_ UNSPECIFIED A02 OTHER SALMONELLA INFECTIONS A02.0 SALMONELLA GASTROENTERITIS A02.1 SALMONELLA SEPTICEMIA A02.2 LOCALIZED SALMONELLA INFECTIONS A02.9 SALMONELLA INFECTION_ UNSPECIFIED A03 SHIGELLOSIS A03.0 SHIGELLOSIS DUE TO SHIGELLA DYSENTERIAE A03.2 SHIGELLOSIS DUE TO SHIGELLA BOYDII A03.9 SHIGELLOSIS_ UNSPECIFIED A04 OTHER BACTERIAL INTESTINAL INFECTIONS A04.0 ENTEROPATHOGENIC ESCHERICHIA COLI INFECTION A04.1 ENTEROTOXIGENIC ESCHERICHIA COLI INFECTION A04.4 OTHER INTESTINAL ESCHERICHIA COLI INFECTIONS A04.5 CAMPYLOBACTER ENTERITIS A04.7 ENTEROCOLITIS DUE TO CLOSTRIDIUM DIFFICILE A04.8 OTHER SPECIFIED BACTERIAL INTESTINAL INFECTIONS A04.9 BACTERIAL INTESTINAL INFECTION_ UNSPECIFIED A05 OTHER BACTERIAL FOOD-BORNE INTOXICATIONS A05.0 FOOD-BORNE STAPHYLOCOCCAL INTOXICATION A05.1 BOTULISM A05.4 FOOD-BORNE BACILLUS CEREUS INTOXICATION A05.8 OTHER SPECIFIED BACTERIAL FOOD-BORNE INTOXICATIONS A05.9 BACTERIAL FOOD-BORNE INTOXICATION_ UNSPECIFIED A06 AMEBIASIS A06.0 ACUTE AMEBIC DYSENTERY A06.1 CHRONIC INTESTINAL AMEBIASIS A06.2 AMEBIC NONDYSENTERIC COLITIS A06.3 AMEBOMA OF INTESTINE A06.4 AMEBIC LIVER ABSCESS A06.5 AMEBIC LUNG ABSCESS A06.6 AMEBIC BRAIN ABSCESS A06.7 CUTANEOUS AMEBIASIS A06.8 AMEBIC INFECTION OF OTHER SITES A06.9 AMEBIASIS_ UNSPECIFIED A07.0 BALANTIDIASIS A07.1 GIARDIASIS [LAMBLIASIS] -

A Very Rare Case of Dissecting Cellulitis of the Scalp in an Indonesian Man
A Very Rare Case of Dissecting Cellulitis of the Scalp in an Indonesian Man Rizky Lendl Prayogo1, Lusiana1, Sri Linuwih Menaldi1, Sondang P. Sirait1, Eliza Miranda1 1Department of Dermatology and Venereology Faculty of Medicine Universitas Indonesia / Dr. Cipto Mangunkusumo National General Hospital, Jakarta, Indonesia Keywords: dissecting cellulitis of the scalp, dissecting folliculitis, follicular occlusion tetrad, diagnosis, isotretinoin Abstract: Dissecting cellulitis of the scalp (DCS), also known as dissecting folliculitis, perifolliculitis capitis abscedens et suffodiens (PCAS), or Hoffman’s disease, is a primary neutrophilic cicatricial alopecia without clear etiology. Along with hidradenitis suppurativa, acne conglobata, and pilonidal cyst, they were recognized as ‘follicular occlusion tetrad’. A 43-year-old Indonesian man presented to our department with four years history of persistent, slightly painful subcutaneous nodules, abscesses, and sinuses that discharged purulent exudate on vertex and occipital scalp. There was also associated patchy alopecia. He had severe acne during his adolescence to early adulthood. Trichoscopic evaluation showed yellowish and whitish area lacking of follicular openings. Histopathological examination showed follicular occlusion, dilatation, and rupture with mixed inflammatory infiltrates, mainly neutrophils. The diagnosis of DCS was confirmed by clinical, trichoscopic, and histopathological examinations. Isotretinoin 20 mg daily was given to normalize the follicular keratinization. Considering its very rare occurrence in an Indonesia man, this case was reported to emphasize the diagnosis of DCS. 1 INTRODUCTION should be considered (Otberg & Shapiro, 2012; Scheinfeld, 2014). Considering its low prevalence in DCS, also known as dissecting folliculitis, PCAS, Indonesia, we are intrigued to report a case or Hoffmann’s disease, is a very rare primary emphasizing the diagnosis of DCS. -

(12) Patent Application Publication (10) Pub. No.: US 2016/0038462 A1 ZHANG Et Al
US 20160038462A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2016/0038462 A1 ZHANG et al. (43) Pub. Date: Feb. 11, 2016 (54) USE OF NK-1 RECEPTOR ANTAGONISTS IN (60) Provisional application No. 61/838,784, filed on Jun. PRURTUS 24, 2013. (71) Applicant: TIGERCAT PHARMA, INC., South Publication Classification San Francisco, CA (US) (51) Int. Cl. (72) Inventors: Xiaoming ZHANG, Sunnyvale, CA A613 L/403 (2006.01) (US); Edward F. SCHNIPPER, A6II 45/06 (2006.01) Redwood City, CA (US); Andrew J. A619/00 (2006.01) PERLMAN, Stanford, CA (US); James (52) U.S. Cl. W. LARRICK, Sunnyvale, CA (US) CPC ............. A6 IK3I/403 (2013.01); A61 K9/0053 (2013.01); A61 K9/0014 (2013.01); A61 K (21) Appl. No.: 14/922,684 45/06 (2013.01) (57) ABSTRACT (22)22) Filed: Oct. 26,9 2015 The invention relates to methods for treatingg pruritusp with NK-1 receptor antagonists such as serlopitant. The invention O O further relates to pharmaceutical compositions comprising Related U.S. Application Data NK-1 receptorantagonists such as serlopitant. In addition, the (60) Division of application No. 14/312.942, filed on Jun. invention encompasses treatment of a pruritus-associated 24, 2014, now Pat. No. 9,198.898, which is a continu condition with serlopitant and an additional antipruritic ation-in-part of application No. 13/925,509, filed on agent, and the use of serlopitant as a sleep aid, optionally in Jun. 24, 2013, now Pat. No. 8,906,951. combination with an additional sleep-aiding agent. Patent Application Publication Feb. -

Differential Diagnosis of the Scalp Hair Folliculitis
Acta Clin Croat 2011; 50:395-402 Review DIFFERENTIAL DIAGNOSIS OF THE SCALP HAIR FOLLICULITIS Liborija Lugović-Mihić1, Freja Barišić2, Vedrana Bulat1, Marija Buljan1, Mirna Šitum1, Lada Bradić1 and Josip Mihić3 1University Department of Dermatovenereology, 2University Department of Ophthalmology, Sestre milosrdnice University Hospital Center, Zagreb; 3Department of Neurosurgery, Dr Josip Benčević General Hospital, Slavonski Brod, Croatia SUMMARY – Scalp hair folliculitis is a relatively common condition in dermatological practice and a major diagnostic and therapeutic challenge due to the lack of exact guidelines. Generally, inflammatory diseases of the pilosebaceous follicle of the scalp most often manifest as folliculitis. There are numerous infective agents that may cause folliculitis, including bacteria, viruses and fungi, as well as many noninfective causes. Several noninfectious diseases may present as scalp hair folli- culitis, such as folliculitis decalvans capillitii, perifolliculitis capitis abscendens et suffodiens, erosive pustular dermatitis, lichen planopilaris, eosinophilic pustular folliculitis, etc. The classification of folliculitis is both confusing and controversial. There are many different forms of folliculitis and se- veral classifications. According to the considerable variability of histologic findings, there are three groups of folliculitis: infectious folliculitis, noninfectious folliculitis and perifolliculitis. The diagno- sis of folliculitis occasionally requires histologic confirmation and cannot be based -

A Deep Learning System for Differential Diagnosis of Skin Diseases
A deep learning system for differential diagnosis of skin diseases 1 1 1 1 1 1,2 † Yuan Liu , Ayush Jain , Clara Eng , David H. Way , Kang Lee , Peggy Bui , Kimberly Kanada , ‡ 1 1 1 Guilherme de Oliveira Marinho , Jessica Gallegos , Sara Gabriele , Vishakha Gupta , Nalini 1,3,§ 1 4 1 1 Singh , Vivek Natarajan , Rainer Hofmann-Wellenhof , Greg S. Corrado , Lily H. Peng , Dale 1 1 † 1, 1, 1, R. Webster , Dennis Ai , Susan Huang , Yun Liu * , R. Carter Dunn * *, David Coz * * Affiliations: 1 G oogle Health, Palo Alto, CA, USA 2 U niversity of California, San Francisco, CA, USA 3 M assachusetts Institute of Technology, Cambridge, MA, USA 4 M edical University of Graz, Graz, Austria † W ork done at Google Health via Advanced Clinical. ‡ W ork done at Google Health via Adecco Staffing. § W ork done at Google Health. *Corresponding author: [email protected] **These authors contributed equally to this work. Abstract Skin and subcutaneous conditions affect an estimated 1.9 billion people at any given time and remain the fourth leading cause of non-fatal disease burden worldwide. Access to dermatology care is limited due to a shortage of dermatologists, causing long wait times and leading patients to seek dermatologic care from general practitioners. However, the diagnostic accuracy of general practitioners has been reported to be only 0.24-0.70 (compared to 0.77-0.96 for dermatologists), resulting in over- and under-referrals, delays in care, and errors in diagnosis and treatment. In this paper, we developed a deep learning system (DLS) to provide a differential diagnosis of skin conditions for clinical cases (skin photographs and associated medical histories). -

190.18 - Serum Iron Studies
Medicare National Coverage Determinations (NCD) Coding Policy Manual and Change Report (ICD-10-CM) 190.18 - Serum Iron Studies HCPCS Codes (Alphanumeric, CPT AMA) Code Description 82728 Ferritin 83540 Iron 83550 Iron Binding capacity 84466 Transferrin ICD-10-CM Codes Covered by Medicare Program The ICD-10-CM codes in the table below can be viewed on CMS’ website as part of Downloads: Lab Code List, at http://www.cms.gov/Medicare/Coverage/CoverageGenInfo/LabNCDsICD10.html Code Description A01.00 Typhoid fever, unspecified A01.01 Typhoid meningitis A01.02 Typhoid fever with heart involvement A01.03 Typhoid pneumonia A01.04 Typhoid arthritis A01.05 Typhoid osteomyelitis A01.09 Typhoid fever with other complications A01.1 Paratyphoid fever A A01.2 Paratyphoid fever B A01.3 Paratyphoid fever C A01.4 Paratyphoid fever, unspecified A02.0 Salmonella enteritis A02.1 Salmonella sepsis A02.20 Localized salmonella infection, unspecified NCD 190.18 January 2021 Changes ICD-10-CM Version – Red Fu Associates, Ltd. January 2021 1 Medicare National Coverage Determinations (NCD) Coding Policy Manual and Change Report (ICD-10-CM) Code Description A02.21 Salmonella meningitis A02.22 Salmonella pneumonia A02.23 Salmonella arthritis A02.24 Salmonella osteomyelitis A02.25 Salmonella pyelonephritis A02.29 Salmonella with other localized infection A02.8 Other specified salmonella infections A02.9 Salmonella infection, unspecified A04.0 Enteropathogenic Escherichia coli infection A04.1 Enterotoxigenic Escherichia coli infection A04.2 Enteroinvasive Escherichia -

Alopecia with Perifollicular Papules and Pustules
Tyler A. Moss, DO; Thomas M. Alopecia with perifollicular Beachkofsky, MD; Samuel F. Almquist, MD; Oliver J. Wisco, DO; papules and pustules Michael R. Murchland, MD A.T. Still University, Our 23-year-old patient thought his hair loss was Kirksville College of Osteopathic Medicine, probably “genetic.” But that didn’t explain the painful Kirksville, Mo (Dr. Moss); Kunsan AB, Republic of pustules. Korea (Dr. Beachkofsky); Wilford Hall Medical Center, Lackland AFB, Tex (Drs. Almquist, Wisco, and Murchland) A 23-year-old African American man Physical examination revealed multiple sought care at our medical center because perifollicular papules and pustules on the [email protected] he had been losing hair over the vertex of his vertex of his scalp with interspersed patches DEPARTMENT EDITOR scalp for the past several years. He indicated of alopecia (FIGURE 1). Th ere were no lesions Richard P. Usatine, MD that his father had early-onset male patterned elsewhere on his body and his past medical University of Texas Health alopecia. As a result, he considered his hair history was otherwise unremarkable. Science Center at San Antonio loss “genetic.” However, he described waxing and waning fl ares of painful pustules associ- ● The authors reported no WHAT IS YOUR DIAGNOSIS? potential confl ict of interest ated with occasional spontaneous bleeding relevant to this article. and discharge of purulent material that oc- ● HOW WOULD YOU MANAGE curred in the same area as the hair loss. THIS PATIENT? FIGURE 1 Alopecia with a painful twist A B PHOTOS COURTESY OF: OLIVER J. WISCO, DO PHOTOS COURTESY This 23-year-old patient said that he had spontaneous bleeding and discharge of purulent material in the area of his hair loss. -
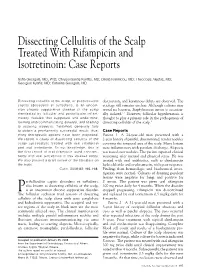
Dissecting Cellulitis of the Scalp Treated with Rifampicin and Isotretinoin: Case Reports
Dissecting Cellulitis of the Scalp Treated With Rifampicin and Isotretinoin: Case Reports Sofia Georgala, MD, PhD; Chrysovalantis Korfitis, MD; Dikaia Ioannidou, MD; Theodosis Alestas, MD; Georgios Kylafis, MD; Caterina Georgala, MD Dissecting cellulitis of the scalp, or perifolliculitis destruction, and keratinous debris are observed. The capitis abscedens et suffodiens, is an uncom- etiology still remains unclear. Although cultures may mon chronic suppurative disease of the scalp reveal no bacteria, Staphylococcus aureus is occasion- manifested by follicular and perifollicular inflam- ally isolated.1,2 However, follicular hyperkeratosis is matory nodules that suppurate and undermine, thought to play a primary role in the pathogenesis of forming intercommunicating sinuses, and leading dissecting cellulitis of the scalp.3 to scarring alopecia. Treatment generally fails to obtain a permanently successful result; thus, Case Reports many therapeutic options have been proposed. Patient 1—A 24-year-old man presented with a We report 4 cases of dissecting cellulitis of the 2-year history of painful, disseminated, tender nodules scalp successfully treated with oral rifampicin covering the temporal area of the scalp. Many lesions and oral isotretinoin. To our knowledge, this is were inflammatory with purulent discharge. Alopecia the first report of oral rifampicin used concomi- was noted over nodules. The patient reported clinical tantly with oral isotretinoin in this disease entity. worsening after mental and physical stress. He was We also present a brief review of the literature on treated with oral antibiotics, such as clindamycin the topic. hydrochloride and erythromycin, with poor response. Cutis. 2008;82:195-198. Findings from hematologic and biochemical inves- tigation were normal. -

The Clinical Conundrum of Pruritus Victoria Garcia-Albea, Karen Limaye
FEATURE ARTICLE The Clinical Conundrum of Pruritus Victoria Garcia-Albea, Karen Limaye ABSTRACT: Pruritus is a common complaint for derma- Pruritus is also the most common symptom in derma- tology patients. Diagnosing the cause of pruritus can tological disease and can be a symptom of several sys- be difficult and is often frustrating for patients and pro- temic diseases (Bernhard, 1994). The overall incidence viders. Even after the diagnosis is made, it can be a chal- of pruritus is unknown because there are no epidemio- lenge to manage and relieve pruritus. This article reviews logical databases for pruritus (Norman, 2003). According common and uncommon causes of pruritus and makes to a 2003 study, pruritus and xerosis are the most com- recommendations for proper and thorough evaluation mon dermatological problems encountered in nursing and management. home patients (Norman, 2003). Key words: Itch, Pruritus INTRODUCTION ETIOLOGY Pruritus (itch) is the most frequent symptom in derma- The skin is equipped with a network of afferent sensory tology (Serling, Leslie, & Maurer, 2011). Itch is the pre- and efferent autonomic nerve branches that respond to dominant symptom associated with acute and chronic various chemical mediators found in the skin (Bernhard, cutaneous disease and is a major symptom in systemic dis- 1994). It is believed that maximal itch production is ease (Elmariah & Lerner, 2011; Steinhoff, Cevikbas, Ikoma, achieved at the basal layer of the epidermis, below which & Berger, 2011). It can be a frustration for both the patient pain is perceived (Bernhard, 1994). Autonomic nerves in- and the clinician. This article will attempt to provide an nervate hair follicles, pili erector muscles, blood vessels, overview of pruritus, a method for thorough and com- eccrine, apocrine, and sebaceous glands (Bernhard, 1994). -

Blood Glucose Testing 2020.Pdf
National Coverage Determination Procedure Code: 82947, 82948, 82962 Blood Glucose Testing CMS Policy Number: 190.20 See also: Medicare Preventive Services Back to NCD List Description: This policy is intended to apply to blood samples used to determine glucose levels. Blood glucose determination may be done using whole blood, serum or plasma. It may be sampled by capillary puncture, as in the fingerstick method, or by vein puncture or arterial sampling. The method for assay may be by color comparison of an indicator stick, by meter assay of whole blood or a filtrate of whole blood, using a device approved for home monitoring, or by using a laboratory assay system using serum or plasma. The convenience of the meter or stick color method allows a patient to have access to blood glucose values in less than a minute or so and has become a standard of care for control of blood glucose, even in the inpatient setting. Indications: Blood glucose values are often necessary for the management of patients with diabetes mellitus, where hyperglycemia and hypoglycemia are often present. They are also critical in the determination of control of blood glucose levels in patient with impaired fasting glucose (FPG 110-125 mg/dL), patient with insulin resistance syndrome and/or carbohydrate intolerance (excessive rise in glucose following ingestion of glucose/glucose sources of food), in patient with a hypoglycemia disorder such as nesidioblastosis or insulinoma, and in patients with a catabolic or malnutrition state. In addition to conditions listed, glucose testing may be medically necessary in patients with tuberculosis, unexplained chronic or recurrent infections, alcoholism, coronary artery disease (especially in women), or unexplained skin conditions (i.e.: pruritis, skin infections, ulceration and gangrene without cause). -
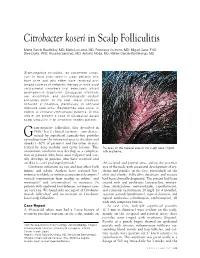
Citrobacter Koseri in Scalp Folliculitis
Citrobacter koseri in Scalp Folliculitis Marta Garcia-Bustinduy, MD; Maria Lecuona, MD; Francisco Guimera, MD; Miguel Saez, PhD; Sara Dorta, PhD; Rosalba Sanchez, MD; Antonio Noda, MD; Rafael Garcia-Montelongo, MD Gram-negative folliculitis, an uncommon condi- tion, is most often seen in older patients who have acne and who either have received pro- longed courses of antibiotic therapy or have used antibacterial cleansers that selectively inhibit gram-positive organisms. Citrobacter infections are uncommon, and dermatologists seldom encounter them. In the past, these infections occurred in hospitals, particularly in neonatal intensive care units. Bacteremias also occur in elderly or immunocompromised patients. In this article, we present a case of Citrobacter koseri scalp folliculitis in an otherwise healthy patient. ram-negative folliculitis, first described in 1968,1 has 2 clinical varieties—one charac- G terized by superficial comedo-free pustules extending from the infranasal area to the chin and cheeks (~80% of patients) and the other charac- terized by deep nodular and cystic lesions. This Pustules on the parietal area of the scalp were ringed uncommon condition may develop as a complica- with erythema. tion in patients who have acne vulgaris2 and usu- ally develops in patients who have received oral antibiotics over prolonged periods.3 the occipital and parietal areas, and on the posterior Citrobacter infections are rare and may affect both area of the neck, with occasional development of ery- infants and adults. Authors have reported bac- thema and papules on the face, particularly on the teremias in elderly or immunocompromised patients,4 chin and cheeks. Folliculitis decalvans and rosacea vertical transmission from mother to infant,5 and had been clinically diagnosed.