190.18 - Serum Iron Studies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
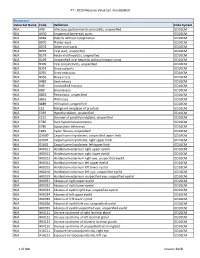
PT - 2020 Measure Value Set Avoidableed
PT - 2020 Measure Value Set_AvoidableED Numerator Value Set Name Code Definition Code System N/A A09 Infectious gastroenteritis and colitis, unspecified ICD10CM N/A A630 Anogenital (venereal) warts ICD10CM N/A B069 Rubella without complication ICD10CM N/A B070 Plantar wart ICD10CM N/A B078 Other viral warts ICD10CM N/A B079 Viral wart, unspecified ICD10CM N/A B179 Acute viral hepatitis, unspecified ICD10CM N/A B199 Unspecified viral hepatitis without hepatic coma ICD10CM N/A B309 Viral conjunctivitis, unspecified ICD10CM N/A B354 Tinea corporis ICD10CM N/A B355 Tinea imbricata ICD10CM N/A B356 Tinea cruris ICD10CM N/A B483 Geotrichosis ICD10CM N/A B49 Unspecified mycosis ICD10CM N/A B80 Enterobiasis ICD10CM N/A B852 Pediculosis, unspecified ICD10CM N/A B853 Phthiriasis ICD10CM N/A B889 Infestation, unspecified ICD10CM N/A C61 Malignant neoplasm of prostate ICD10CM N/A E039 Hypothyroidism, unspecified ICD10CM N/A E215 Disorder of parathyroid gland, unspecified ICD10CM N/A E780 Pure hypercholesterolemia ICD10CM N/A E786 Lipoprotein deficiency ICD10CM N/A E849 Cystic fibrosis, unspecified ICD10CM N/A G5600 Carpal tunnel syndrome, unspecified upper limb ICD10CM N/A G5601 Carpal tunnel syndrome, right upper limb ICD10CM N/A G5602 Carpal tunnel syndrome, left upper limb ICD10CM N/A H00011 Hordeolum externum right upper eyelid ICD10CM N/A H00012 Hordeolum externum right lower eyelid ICD10CM N/A H00013 Hordeolum externum right eye, unspecified eyelid ICD10CM N/A H00014 Hordeolum externum left upper eyelid ICD10CM N/A H00015 Hordeolum externum -

Recent Advances in Surgery the Blind-Loop Syndrome After Gastric
Recent advances in surgery Conducted by ALFRED BLALOCK, M.D. The blind-loop syndrome after gastric operations ince the earliest reports by Whitees time, several examples of the blind-loop ANATOMIC CONFIGURATION OF BLIND LOOPS Various examples of gastrointestinal blind and Wangensteen;O a side-arm loop has been employed as in Fig. 1, A, in which the loop is arranged so as to be self-filling. The side loop arrangement is the one which most 849 850 Recent advances in surgery Surgery ;.$ Nouernbcr 1961 & ad cumulated from observations on lesions at differing sites in the gastrointestinal tract. The principles involved apply, with varia- tions, to blind loops at all levels. The best- known feature of the blind-loop syndrome is megaloblastic anemia, which is due to dis- ruption of vitamin BI2 absorption. Normally, dietary vitamin B12 (Castle's extrinsic fac- tor) is absorbed after an incompletely under- stood interaction with intrinsic factor (Fig. 3, A), a mucoprotein secreted by the gastric rnu~osa.*~In man, the principal site of B,, absorption is the ileum.7* Vitamin B,, deficiency can develop by a number of alternative mechanisms. Rarely loops which have caGsed the blind-loop- syndrome.- is there dietary deficiency of this nutritional A, Anastomosis with formation of a self-filled stagnant loop, B, with jejunal diverticulosis, C, factor. Commonly, as in pernicious anemia with intestinal strictures, D, after enteroenteros- (Fig. 3, B) or after total gastrectomy,Sgthere tomies or fistulas, and E, after gastric operation. is absent intrinsic factor due to gastric atrophy or the absence. of the stomach, re- resembles a blind loop which develops after spectively. -
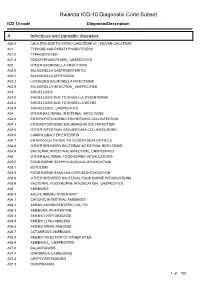
Rwanda ICD-10 Diagnostic Code Subset
Rwanda ICD-10 Diagnostic Code Subset ICD 10 code Diagnosis/Description A Infectious and parasitic diseases A00.0 CHOLERA DUE TO VIBRIO CHOLERAE 01_ BIOVAR CHOLERAE A01 TYPHOID AND PARATYPHOID FEVERS A01.0 TYPHOID FEVER A01.4 PARATYPHOID FEVER_ UNSPECIFIED A02 OTHER SALMONELLA INFECTIONS A02.0 SALMONELLA GASTROENTERITIS A02.1 SALMONELLA SEPTICEMIA A02.2 LOCALIZED SALMONELLA INFECTIONS A02.9 SALMONELLA INFECTION_ UNSPECIFIED A03 SHIGELLOSIS A03.0 SHIGELLOSIS DUE TO SHIGELLA DYSENTERIAE A03.2 SHIGELLOSIS DUE TO SHIGELLA BOYDII A03.9 SHIGELLOSIS_ UNSPECIFIED A04 OTHER BACTERIAL INTESTINAL INFECTIONS A04.0 ENTEROPATHOGENIC ESCHERICHIA COLI INFECTION A04.1 ENTEROTOXIGENIC ESCHERICHIA COLI INFECTION A04.4 OTHER INTESTINAL ESCHERICHIA COLI INFECTIONS A04.5 CAMPYLOBACTER ENTERITIS A04.7 ENTEROCOLITIS DUE TO CLOSTRIDIUM DIFFICILE A04.8 OTHER SPECIFIED BACTERIAL INTESTINAL INFECTIONS A04.9 BACTERIAL INTESTINAL INFECTION_ UNSPECIFIED A05 OTHER BACTERIAL FOOD-BORNE INTOXICATIONS A05.0 FOOD-BORNE STAPHYLOCOCCAL INTOXICATION A05.1 BOTULISM A05.4 FOOD-BORNE BACILLUS CEREUS INTOXICATION A05.8 OTHER SPECIFIED BACTERIAL FOOD-BORNE INTOXICATIONS A05.9 BACTERIAL FOOD-BORNE INTOXICATION_ UNSPECIFIED A06 AMEBIASIS A06.0 ACUTE AMEBIC DYSENTERY A06.1 CHRONIC INTESTINAL AMEBIASIS A06.2 AMEBIC NONDYSENTERIC COLITIS A06.3 AMEBOMA OF INTESTINE A06.4 AMEBIC LIVER ABSCESS A06.5 AMEBIC LUNG ABSCESS A06.6 AMEBIC BRAIN ABSCESS A06.7 CUTANEOUS AMEBIASIS A06.8 AMEBIC INFECTION OF OTHER SITES A06.9 AMEBIASIS_ UNSPECIFIED A07.0 BALANTIDIASIS A07.1 GIARDIASIS [LAMBLIASIS] -

Human Anatomy As Related to Tumor Formation Book Four
SEER Program Self Instructional Manual for Cancer Registrars Human Anatomy as Related to Tumor Formation Book Four Second Edition U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service National Institutesof Health SEER PROGRAM SELF-INSTRUCTIONAL MANUAL FOR CANCER REGISTRARS Book 4 - Human Anatomy as Related to Tumor Formation Second Edition Prepared by: SEER Program Cancer Statistics Branch National Cancer Institute Editor in Chief: Evelyn M. Shambaugh, M.A., CTR Cancer Statistics Branch National Cancer Institute Assisted by Self-Instructional Manual Committee: Dr. Robert F. Ryan, Emeritus Professor of Surgery Tulane University School of Medicine New Orleans, Louisiana Mildred A. Weiss Los Angeles, California Mary A. Kruse Bethesda, Maryland Jean Cicero, ART, CTR Health Data Systems Professional Services Riverdale, Maryland Pat Kenny Medical Illustrator for Division of Research Services National Institutes of Health CONTENTS BOOK 4: HUMAN ANATOMY AS RELATED TO TUMOR FORMATION Page Section A--Objectives and Content of Book 4 ............................... 1 Section B--Terms Used to Indicate Body Location and Position .................. 5 Section C--The Integumentary System ..................................... 19 Section D--The Lymphatic System ....................................... 51 Section E--The Cardiovascular System ..................................... 97 Section F--The Respiratory System ....................................... 129 Section G--The Digestive System ......................................... 163 Section -

Head and Neck Specimens
Head and Neck Specimens DEFINITIONS AND GENERAL COMMENTS: All specimens, even of the same type, are unique, and this is particularly true for Head and Neck specimens. Thus, while this outline is meant to provide a guide to grossing the common head and neck specimens at UAB, it is not all inclusive and will not capture every scenario. Thus, careful assessment of each specimen with some modifications of what follows below may be needed on a case by case basis. When in doubt always consult with a PA, Chief/Senior Resident and/or the Head and Neck Pathologist on service. Specimen-derived margin: A margin taken directly from the main specimen-either a shave or radial. Tumor bed margin: A piece of tissue taken from the operative bed after the main specimen has been resected. This entire piece of tissue may represent the margin, or it could also be specifically oriented-check specimen label/requisition for any further orientation. Margin status as determined from specimen-derived margins has been shown to better predict local recurrence as compared to tumor bed margins (Surgical Pathology Clinics. 2017; 10: 1-14). At UAB, both methods are employed. Note to grosser: However, even if a surgeon submits tumor bed margins separately, the grosser must still sample the specimen margins. Figure 1: Shave vs radial (perpendicular) margin: Figure adapted from Surgical Pathology Clinics. 2017; 10: 1-14): Red lines: radial section (perpendicular) of margin Blue line: Shave of margin Comparison of shave and radial margins (Table 1 from Chiosea SI. Intraoperative Margin Assessment in Early Oral Squamous Cell Carcinoma. -

Long-Term Outcome After Neonatal Meconium Obstruction
Long-term Outcome After Neonatal Meconium Obstruction Julie R. Fuchs, MD, and Jacob C. Langer, MD ABSTRACT. Objective. It is unclear whether children meconium ileus and those undergoing resection or enter- with cystic fibrosis (CF) who present with neonatal ostomy. Patients with meconium obstruction who do not meconium ileus have a different long-term outcome from have CF have an excellent long-term prognosis. This those presenting later in childhood with pulmonary com- information will be useful in counseling the families of plications or failure to thrive. We examined a cohort of infants presenting with neonatal meconium obstruction. patients with meconium ileus, and compared their long- Pediatrics 1998;101(4). URL: http://www.pediatrics.org/ term outcome with children who had CF without meco- cgi/content/full/101/4/e7; cystic fibrosis, meconium ileus, nium ileus and neonates who had meconium obstruction meconium plug syndrome. without CF (meconium plug syndrome). Study Design. Comparative study using retrospective and follow-up interview data. ABBREVIATION. CF, cystic fibrosis. Patients. Group 1 consisted of 35 surviving CF pa- tients who presented with meconium ileus between 1966 econium obstruction in the neonate is a and 1992. Two control groups were also studied: 35 age- spectrum of disease that includes meco- and sex-matched CF patients without meconium ileus 1 (group 2), and 12 infants presenting with meconium plug Mnium ileus and meconium plug syndrome. syndrome during the same time period (group 3). Meconium ileus is characterized by extremely viscid, Outcome Measures. Pulmonary, gastrointestinal, nu- protein-rich inspissated meconium causing terminal tritional, and functional status were reviewed, and sur- ileal obstruction, and accounts for approximately gical complications were recorded. -
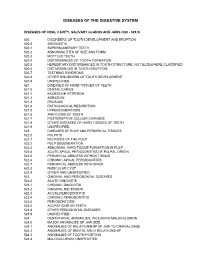
Diagnostic Codes
DISEASES OF THE DIGESTIVE SYSTEM DISEASES OF ORAL CAVITY, SALIVARY GLANDS AND JAWS (520 - 529.9) 520 DISORDERS OF TOOTH DEVELOPMENT AND ERUPTION 520.0 ANODONTIA 520.1 SUPERNUMERARY TEETH 520.2 ABNORMALITIES OF SIZE AND FORM 520.3 MOTTLED TEETH 520.4 DISTURBANCES OF TOOTH FORMATION 520.5 HEREDITARY DISTURBANCES IN TOOTH STRUCTURE, NOT ELSEWHERE CLASSIFIED 520.6 DISTURBANCES IN TOOTH ERUPTION 520.7 TEETHING SYNDROME 520.8 OTHER DISORDERS OF TOOTH DEVELOPMENT 520.9 UNSPECIFIED 521 DISEASES OF HARD TISSUES OF TEETH 521.0 DENTAL CARIES 521.1 EXCESSIVE ATTRITION 521.2 ABRASION 521.3 EROSION 521.4 PATHOLOGICAL RESORPTION 521.5 HYPERCEMENTOSIS 521.6 ANKYLOSIS OF TEETH 521.7 POSTERUPTIVE COLOUR CHANGES 521.8 OTHER DISEASES OF HARD TISSUES OF TEETH 521.9 UNSPECIFIED 522 DISEASES OF PULP AND PERIAPICAL TISSUES 522.0 PULPITIS 522.1 NECROSIS OF THE PULP 522.2 PULP DEGENERATION 522.3 ABNORMAL HARD TISSUE FORMATION IN PULP 522.4 ACUTE APICAL PERIODONTITIS OF PULPAL ORIGIN 522.5 PERIAPICAL ABSCESS WITHOUT SINUS 522.6 CHRONIC APICAL PERIODONTITIS 522.7 PERIAPICAL ABSCESS WITH SINUS 522.8 RADICULAR CYST 522.9 OTHER AND UNSPECIFIED 523 GINGIVAL AND PERIODONTAL DISEASES 523.0 ACUTE GINGIVITIS 523.1 CHRONIC GINGIVITIS 523.2 GINGIVAL RECESSION 523.3 ACUTE PERIODONTITIS 523.4 CHRONIC PERIODONTITIS 523.5 PERIODONTOSIS 523.6 ACCRETIONS ON TEETH 523.8 OTHER PERIODONTAL DISEASES 523.9 UNSPECIFIED 524 DENTOFACIAL ANOMALIES, INCLUDING MALOCCLUSION 524.0 MAJOR ANOMALIES OF JAW SIZE 524.1 ANOMALIES OF RELATIONSHIP OF JAW TO CRANIAL BASE 524.2 ANOMALIES OF DENTAL ARCH -

Dysfunction of the Continent Ileostomy: Clinical Features and Bacteriology*
Gut: first published as 10.1136/gut.24.3.193 on 1 March 1983. Downloaded from Gut, 1983, 24, 193-201 Dysfunction of the continent ileostomy: clinical features and bacteriology* DARLENE G KELLY, S F PHILLIPS. K A KELLY, W M WEINSTEIN, AND MARY J R GILCHRIST From the Gastroenterology Unit and Department of Laboratorv Medicine, Mayo Clinic and Mayo Foundation, Rochester, Minnesota, and the Departmlent of Medicine, University of California, Los Angeles, California, USA SUMMARY The pathogenesis and treatment of dysfunction of the continent ileostomy was investigated in 12 patients, five of whom had asymptomatic malabsorption and seven of whom had acute complaints. The number of anaerobic bacteria in jejunal aspirates was increased in patients with pouch malfunction (range 103 to 108/g aspirate), but the microbiology of ileal effluent and the morphology of the ileal mucosa could not be correlated with dysfunction. Bile acid breath tests and lactose tolerance tests were not, however, reliable indicators of jejunal bacterial overgrowth. The symptoms, the malabsorption, and the number of jejunal and ileal anaerobic bacteria decreased in patients during treatment with metronidazole, implicating overgrowth of anaerobic bacterial flora in the pathogenesis of the syndrome. The continent ileostomy (ileal pouch), devised by vitamin B12,9 12 proliferation of anaerobic bacteria http://gut.bmj.com/ Kock,' has been used as an alternative to con- in the pouch,9 inflammation in the pouch,7 ventional ileostomy for selected patients with incontinence,"' difficulty with intubation,1' and ulcerative colitis and familial polyposis.2-5 The bloody discharge.5 We previously reported reservoir functions satisfactorily in most patients, diarrhoea with some features of malabsorption in but malfunction of the 'nipple valve' may occur in up approximately one-third of asymptomatic patients to a third of patients and lead to incontinence. -

(12) Patent Application Publication (10) Pub. No.: US 2016/0038462 A1 ZHANG Et Al
US 20160038462A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2016/0038462 A1 ZHANG et al. (43) Pub. Date: Feb. 11, 2016 (54) USE OF NK-1 RECEPTOR ANTAGONISTS IN (60) Provisional application No. 61/838,784, filed on Jun. PRURTUS 24, 2013. (71) Applicant: TIGERCAT PHARMA, INC., South Publication Classification San Francisco, CA (US) (51) Int. Cl. (72) Inventors: Xiaoming ZHANG, Sunnyvale, CA A613 L/403 (2006.01) (US); Edward F. SCHNIPPER, A6II 45/06 (2006.01) Redwood City, CA (US); Andrew J. A619/00 (2006.01) PERLMAN, Stanford, CA (US); James (52) U.S. Cl. W. LARRICK, Sunnyvale, CA (US) CPC ............. A6 IK3I/403 (2013.01); A61 K9/0053 (2013.01); A61 K9/0014 (2013.01); A61 K (21) Appl. No.: 14/922,684 45/06 (2013.01) (57) ABSTRACT (22)22) Filed: Oct. 26,9 2015 The invention relates to methods for treatingg pruritusp with NK-1 receptor antagonists such as serlopitant. The invention O O further relates to pharmaceutical compositions comprising Related U.S. Application Data NK-1 receptorantagonists such as serlopitant. In addition, the (60) Division of application No. 14/312.942, filed on Jun. invention encompasses treatment of a pruritus-associated 24, 2014, now Pat. No. 9,198.898, which is a continu condition with serlopitant and an additional antipruritic ation-in-part of application No. 13/925,509, filed on agent, and the use of serlopitant as a sleep aid, optionally in Jun. 24, 2013, now Pat. No. 8,906,951. combination with an additional sleep-aiding agent. Patent Application Publication Feb. -

Head and Neck: Summary Stage 2018 Coding Manual V2.0
HEAD AND NECK DEFINITION OF ANATOMIC SITES WITHIN THE HEAD AND NECK Note: Not all sites in the lip, oral cavity, pharynx and salivary glands are listed below. All sites to which a Summary Stage chapter applies are listed at the beginning of the chapter. LIP, ORAL CAVITY and PHARYNX The oral cavity extends from the skin-vermilion junction of the lips to the junction of the hard and soft palate above and to the line of circumvallate papillae below. LIP AND ORAL CAVITY Site ICD-O Description LIPS C00_ Vermilion surface, mucosal lip, labial (mucosa) upper and lower, form the upper and lower anterior wall of the oral cavity. They consist of an exposed surface of modified epidermis beginning at the junction of the vermilion border with the skin and including only the vermilion surface or that portion of the lip that meets the opposing lip. The lips extend from commissure to commissure. COMMISSURE C006 (corner of mouth) is the point of union of upper and lower lips and is part of the lip OF LIP ANTERIOR C02_ (mobile or oral tongue) consists of the freely movable portion of the tongue which 2/3 OF extends anteriorly from the line of circumvallate papillae to the root of the tongue at the TONGUE junction of the floor of the mouth. It is composed of four areas: tip, lateral borders, dorsum, and undersurface or ventral surface (non-villous surface). UPPER GUM C030 (upper alveolar ridge) is the covering mucosa of the alveolar process of the maxilla, extending from the line of attachment of mucosa in the upper gingival buccal gutter to the junction of the hard palate. -

A Rare Case of Multiple Perforated Jejunal Diverticulae - Case Report
International Journal of Recent Trends in Science And Technology, ISSN 2277-2812 E-ISSN 2249-8109, Volume 10, Issue 3, 2014 pp 458-460 A Rare Case of Multiple Perforated Jejunal Diverticulae - Case Report B. Easwaran 1, G. P. Sekar 2, K. Senthil Kumaran 3, B. Selvaraj 4 1Professor and HOD, 2,4 Associate Professor, 3Assisstant Professor, Department of Surgery, SVMCH, Pondicherry, INDIA. *Corresponding Address: [email protected] Case report Abstract: Jejunal diverticula are very rare with an incidence of less rate 70/Min and BP was 100/60 mm HG. Systemic 1 than 0.5% and are usually asymptomatic. The etiology remains examination was normal. The abdomen was soft, unclear. Since they arise from herniation of the mucosa and distended and tenderness was present in all quadrants. A submucosa through a weak portion of the bowel they are classified as false diverticula of the pulsion type. Complications occur in 10 3 hours later guarding and rigidity also developed to 30% of patients (Ref. 22 ). They are chronic abdominal pain, Blind .clinically free fluid was also present. The bowel sounds loop syndrome, malabsorption, steatorrhoea, megaloblastic anemia, were sluggish. There was tenderness on per rectal hemorrhage, diverticulitis, obstruction, abscess formation, examination. Lab tests revealed impaired renal profile intussusception, volvulus 23 , small bowel obstruction due to 24,25,26,27 (urea 130 mg/d L; creatinine 4.5mg/d L) .Other blood enteroliths and rarely perforation. Jejunal diverticula have a tests were normal. Abdominal x-ray showed air under higher rate of complication than other small bowel diverticula 22 . Diagnosing complicated acute jejunal diverticulosis based on right dome of diaphragm, dilated small bowel loops. -

A Retrospective Comparison of Tumor Recurrence and Patient Survival After
Yale University EliScholar – A Digital Platform for Scholarly Publishing at Yale Yale Medicine Thesis Digital Library School of Medicine 1987 A retrospective comparison of tumor recurrence and patient survival after treatment with preoperative radiation therapy and surgery, or surgery and postoperative radiation therapy for squamous cell carcinoma of the pyriform sinus and hypopharynx Jesse George Wardlow Jr. Yale University Follow this and additional works at: http://elischolar.library.yale.edu/ymtdl Recommended Citation Wardlow, Jesse George Jr., "A retrospective comparison of tumor recurrence and patient survival after treatment with preoperative radiation therapy and surgery, or surgery and postoperative radiation therapy for squamous cell carcinoma of the pyriform sinus and hypopharynx" (1987). Yale Medicine Thesis Digital Library. 3284. http://elischolar.library.yale.edu/ymtdl/3284 This Open Access Thesis is brought to you for free and open access by the School of Medicine at EliScholar – A Digital Platform for Scholarly Publishing at Yale. It has been accepted for inclusion in Yale Medicine Thesis Digital Library by an authorized administrator of EliScholar – A Digital Platform for Scholarly Publishing at Yale. For more information, please contact [email protected]. A RETROSPECTIVE COMPARISON OF Permission for photocopying or microfilming of purpose of individual scholarly consultation or reference is hereby granted by the author. This permission is not to be interpreted as affecting publication of this work, or otherwise placing