CSHCS Qualifying Diagnoses Effective 01/01/2021
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Recent Advances in Surgery the Blind-Loop Syndrome After Gastric
Recent advances in surgery Conducted by ALFRED BLALOCK, M.D. The blind-loop syndrome after gastric operations ince the earliest reports by Whitees time, several examples of the blind-loop ANATOMIC CONFIGURATION OF BLIND LOOPS Various examples of gastrointestinal blind and Wangensteen;O a side-arm loop has been employed as in Fig. 1, A, in which the loop is arranged so as to be self-filling. The side loop arrangement is the one which most 849 850 Recent advances in surgery Surgery ;.$ Nouernbcr 1961 & ad cumulated from observations on lesions at differing sites in the gastrointestinal tract. The principles involved apply, with varia- tions, to blind loops at all levels. The best- known feature of the blind-loop syndrome is megaloblastic anemia, which is due to dis- ruption of vitamin BI2 absorption. Normally, dietary vitamin B12 (Castle's extrinsic fac- tor) is absorbed after an incompletely under- stood interaction with intrinsic factor (Fig. 3, A), a mucoprotein secreted by the gastric rnu~osa.*~In man, the principal site of B,, absorption is the ileum.7* Vitamin B,, deficiency can develop by a number of alternative mechanisms. Rarely loops which have caGsed the blind-loop- syndrome.- is there dietary deficiency of this nutritional A, Anastomosis with formation of a self-filled stagnant loop, B, with jejunal diverticulosis, C, factor. Commonly, as in pernicious anemia with intestinal strictures, D, after enteroenteros- (Fig. 3, B) or after total gastrectomy,Sgthere tomies or fistulas, and E, after gastric operation. is absent intrinsic factor due to gastric atrophy or the absence. of the stomach, re- resembles a blind loop which develops after spectively. -

Reportable BD Tables Apr2019.Pdf
April 2019 Georgia Department of Public Health | Division of Health Protection | Maternal and Child Health Epidemiology Unit Reportable Birth Defects with ICD-10-CM Codes Reportable Birth Defects in Georgia with ICD-10-CM Diagnosis Codes Table D.1 Brain Malformations and Neural Tube Defects ICD-10-CM Diagnosis Codes Birth Defect ICD-10-CM 1. Brain Malformations and Neural Tube Defects Q00-Q05, Q07 Anencephaly Q00.0 Craniorachischisis Q00.1 Iniencephaly Q00.2 Frontal encephalocele Q01.0 Nasofrontal encephalocele Q01.1 Occipital encephalocele Q01.2 Encephalocele of other sites Q01.8 Encephalocele, unspecified Q01.9 Microcephaly Q02 Malformations of aqueduct of Sylvius Q03.0 Atresia of foramina of Magendie and Luschka (including Dandy-Walker) Q03.1 Other congenital hydrocephalus (including obstructive hydrocephaly) Q03.8 Congenital hydrocephalus, unspecified Q03.9 Congenital malformations of corpus callosum Q04.0 Arhinencephaly Q04.1 Holoprosencephaly Q04.2 Other reduction deformities of brain Q04.3 Septo-optic dysplasia of brain Q04.4 Congenital cerebral cyst (porencephaly, schizencephaly) Q04.6 Other specified congenital malformations of brain (including ventriculomegaly) Q04.8 Congenital malformation of brain, unspecified Q04.9 Cervical spina bifida with hydrocephalus Q05.0 Thoracic spina bifida with hydrocephalus Q05.1 Lumbar spina bifida with hydrocephalus Q05.2 Sacral spina bifida with hydrocephalus Q05.3 Unspecified spina bifida with hydrocephalus Q05.4 Cervical spina bifida without hydrocephalus Q05.5 Thoracic spina bifida without -

MICHIGAN BIRTH DEFECTS REGISTRY Cytogenetics Laboratory Reporting Instructions 2002
MICHIGAN BIRTH DEFECTS REGISTRY Cytogenetics Laboratory Reporting Instructions 2002 Michigan Department of Community Health Community Public Health Agency and Center for Health Statistics 3423 N. Martin Luther King Jr. Blvd. P. O. Box 30691 Lansing, Michigan 48909 Michigan Department of Community Health James K. Haveman, Jr., Director B-274a (March, 2002) Authority: P.A. 236 of 1988 BIRTH DEFECTS REGISTRY MICHIGAN DEPARTMENT OF COMMUNITY HEALTH BIRTH DEFECTS REGISTRY STAFF The Michigan Birth Defects Registry staff prepared this manual to provide the information needed to submit reports. The manual contains copies of the legislation mandating the Registry, the Rules for reporting birth defects, information about reportable and non reportable birth defects, and methods of reporting. Changes in the manual will be sent to each hospital contact to assist in complete and accurate reporting. We are interested in your comments about the manual and any suggestions about information you would like to receive. The Michigan Birth Defects Registry is located in the Office of the State Registrar and Division of Health Statistics. Registry staff can be reached at the following address: Michigan Birth Defects Registry 3423 N. Martin Luther King Jr. Blvd. P.O. Box 30691 Lansing MI 48909 Telephone number (517) 335-8678 FAX (517) 335-9513 FOR ASSISTANCE WITH SPECIFIC QUESTIONS PLEASE CONTACT Glenn E. Copeland (517) 335-8677 Cytogenetics Laboratory Reporting Instructions I. INTRODUCTION This manual provides detailed instructions on the proper reporting of diagnosed birth defects by cytogenetics laboratories. A report is required from cytogenetics laboratories whenever a reportable condition is diagnosed for patients under the age of two years. -

Long-Term Outcome After Neonatal Meconium Obstruction
Long-term Outcome After Neonatal Meconium Obstruction Julie R. Fuchs, MD, and Jacob C. Langer, MD ABSTRACT. Objective. It is unclear whether children meconium ileus and those undergoing resection or enter- with cystic fibrosis (CF) who present with neonatal ostomy. Patients with meconium obstruction who do not meconium ileus have a different long-term outcome from have CF have an excellent long-term prognosis. This those presenting later in childhood with pulmonary com- information will be useful in counseling the families of plications or failure to thrive. We examined a cohort of infants presenting with neonatal meconium obstruction. patients with meconium ileus, and compared their long- Pediatrics 1998;101(4). URL: http://www.pediatrics.org/ term outcome with children who had CF without meco- cgi/content/full/101/4/e7; cystic fibrosis, meconium ileus, nium ileus and neonates who had meconium obstruction meconium plug syndrome. without CF (meconium plug syndrome). Study Design. Comparative study using retrospective and follow-up interview data. ABBREVIATION. CF, cystic fibrosis. Patients. Group 1 consisted of 35 surviving CF pa- tients who presented with meconium ileus between 1966 econium obstruction in the neonate is a and 1992. Two control groups were also studied: 35 age- spectrum of disease that includes meco- and sex-matched CF patients without meconium ileus 1 (group 2), and 12 infants presenting with meconium plug Mnium ileus and meconium plug syndrome. syndrome during the same time period (group 3). Meconium ileus is characterized by extremely viscid, Outcome Measures. Pulmonary, gastrointestinal, nu- protein-rich inspissated meconium causing terminal tritional, and functional status were reviewed, and sur- ileal obstruction, and accounts for approximately gical complications were recorded. -
Diagnostic Codes
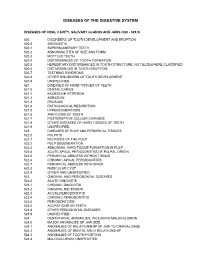
DISEASES OF THE DIGESTIVE SYSTEM DISEASES OF ORAL CAVITY, SALIVARY GLANDS AND JAWS (520 - 529.9) 520 DISORDERS OF TOOTH DEVELOPMENT AND ERUPTION 520.0 ANODONTIA 520.1 SUPERNUMERARY TEETH 520.2 ABNORMALITIES OF SIZE AND FORM 520.3 MOTTLED TEETH 520.4 DISTURBANCES OF TOOTH FORMATION 520.5 HEREDITARY DISTURBANCES IN TOOTH STRUCTURE, NOT ELSEWHERE CLASSIFIED 520.6 DISTURBANCES IN TOOTH ERUPTION 520.7 TEETHING SYNDROME 520.8 OTHER DISORDERS OF TOOTH DEVELOPMENT 520.9 UNSPECIFIED 521 DISEASES OF HARD TISSUES OF TEETH 521.0 DENTAL CARIES 521.1 EXCESSIVE ATTRITION 521.2 ABRASION 521.3 EROSION 521.4 PATHOLOGICAL RESORPTION 521.5 HYPERCEMENTOSIS 521.6 ANKYLOSIS OF TEETH 521.7 POSTERUPTIVE COLOUR CHANGES 521.8 OTHER DISEASES OF HARD TISSUES OF TEETH 521.9 UNSPECIFIED 522 DISEASES OF PULP AND PERIAPICAL TISSUES 522.0 PULPITIS 522.1 NECROSIS OF THE PULP 522.2 PULP DEGENERATION 522.3 ABNORMAL HARD TISSUE FORMATION IN PULP 522.4 ACUTE APICAL PERIODONTITIS OF PULPAL ORIGIN 522.5 PERIAPICAL ABSCESS WITHOUT SINUS 522.6 CHRONIC APICAL PERIODONTITIS 522.7 PERIAPICAL ABSCESS WITH SINUS 522.8 RADICULAR CYST 522.9 OTHER AND UNSPECIFIED 523 GINGIVAL AND PERIODONTAL DISEASES 523.0 ACUTE GINGIVITIS 523.1 CHRONIC GINGIVITIS 523.2 GINGIVAL RECESSION 523.3 ACUTE PERIODONTITIS 523.4 CHRONIC PERIODONTITIS 523.5 PERIODONTOSIS 523.6 ACCRETIONS ON TEETH 523.8 OTHER PERIODONTAL DISEASES 523.9 UNSPECIFIED 524 DENTOFACIAL ANOMALIES, INCLUDING MALOCCLUSION 524.0 MAJOR ANOMALIES OF JAW SIZE 524.1 ANOMALIES OF RELATIONSHIP OF JAW TO CRANIAL BASE 524.2 ANOMALIES OF DENTAL ARCH -

Dysfunction of the Continent Ileostomy: Clinical Features and Bacteriology*
Gut: first published as 10.1136/gut.24.3.193 on 1 March 1983. Downloaded from Gut, 1983, 24, 193-201 Dysfunction of the continent ileostomy: clinical features and bacteriology* DARLENE G KELLY, S F PHILLIPS. K A KELLY, W M WEINSTEIN, AND MARY J R GILCHRIST From the Gastroenterology Unit and Department of Laboratorv Medicine, Mayo Clinic and Mayo Foundation, Rochester, Minnesota, and the Departmlent of Medicine, University of California, Los Angeles, California, USA SUMMARY The pathogenesis and treatment of dysfunction of the continent ileostomy was investigated in 12 patients, five of whom had asymptomatic malabsorption and seven of whom had acute complaints. The number of anaerobic bacteria in jejunal aspirates was increased in patients with pouch malfunction (range 103 to 108/g aspirate), but the microbiology of ileal effluent and the morphology of the ileal mucosa could not be correlated with dysfunction. Bile acid breath tests and lactose tolerance tests were not, however, reliable indicators of jejunal bacterial overgrowth. The symptoms, the malabsorption, and the number of jejunal and ileal anaerobic bacteria decreased in patients during treatment with metronidazole, implicating overgrowth of anaerobic bacterial flora in the pathogenesis of the syndrome. The continent ileostomy (ileal pouch), devised by vitamin B12,9 12 proliferation of anaerobic bacteria http://gut.bmj.com/ Kock,' has been used as an alternative to con- in the pouch,9 inflammation in the pouch,7 ventional ileostomy for selected patients with incontinence,"' difficulty with intubation,1' and ulcerative colitis and familial polyposis.2-5 The bloody discharge.5 We previously reported reservoir functions satisfactorily in most patients, diarrhoea with some features of malabsorption in but malfunction of the 'nipple valve' may occur in up approximately one-third of asymptomatic patients to a third of patients and lead to incontinence. -

A Rare Case of Multiple Perforated Jejunal Diverticulae - Case Report
International Journal of Recent Trends in Science And Technology, ISSN 2277-2812 E-ISSN 2249-8109, Volume 10, Issue 3, 2014 pp 458-460 A Rare Case of Multiple Perforated Jejunal Diverticulae - Case Report B. Easwaran 1, G. P. Sekar 2, K. Senthil Kumaran 3, B. Selvaraj 4 1Professor and HOD, 2,4 Associate Professor, 3Assisstant Professor, Department of Surgery, SVMCH, Pondicherry, INDIA. *Corresponding Address: [email protected] Case report Abstract: Jejunal diverticula are very rare with an incidence of less rate 70/Min and BP was 100/60 mm HG. Systemic 1 than 0.5% and are usually asymptomatic. The etiology remains examination was normal. The abdomen was soft, unclear. Since they arise from herniation of the mucosa and distended and tenderness was present in all quadrants. A submucosa through a weak portion of the bowel they are classified as false diverticula of the pulsion type. Complications occur in 10 3 hours later guarding and rigidity also developed to 30% of patients (Ref. 22 ). They are chronic abdominal pain, Blind .clinically free fluid was also present. The bowel sounds loop syndrome, malabsorption, steatorrhoea, megaloblastic anemia, were sluggish. There was tenderness on per rectal hemorrhage, diverticulitis, obstruction, abscess formation, examination. Lab tests revealed impaired renal profile intussusception, volvulus 23 , small bowel obstruction due to 24,25,26,27 (urea 130 mg/d L; creatinine 4.5mg/d L) .Other blood enteroliths and rarely perforation. Jejunal diverticula have a tests were normal. Abdominal x-ray showed air under higher rate of complication than other small bowel diverticula 22 . Diagnosing complicated acute jejunal diverticulosis based on right dome of diaphragm, dilated small bowel loops. -

Statistical Analysis Plan
Cover Page for Statistical Analysis Plan Sponsor name: Novo Nordisk A/S NCT number NCT03061214 Sponsor trial ID: NN9535-4114 Official title of study: SUSTAINTM CHINA - Efficacy and safety of semaglutide once-weekly versus sitagliptin once-daily as add-on to metformin in subjects with type 2 diabetes Document date: 22 August 2019 Semaglutide s.c (Ozempic®) Date: 22 August 2019 Novo Nordisk Trial ID: NN9535-4114 Version: 1.0 CONFIDENTIAL Clinical Trial Report Status: Final Appendix 16.1.9 16.1.9 Documentation of statistical methods List of contents Statistical analysis plan...................................................................................................................... /LQN Statistical documentation................................................................................................................... /LQN Redacted VWDWLVWLFDODQDO\VLVSODQ Includes redaction of personal identifiable information only. Statistical Analysis Plan Date: 28 May 2019 Novo Nordisk Trial ID: NN9535-4114 Version: 1.0 CONFIDENTIAL UTN:U1111-1149-0432 Status: Final EudraCT No.:NA Page: 1 of 30 Statistical Analysis Plan Trial ID: NN9535-4114 Efficacy and safety of semaglutide once-weekly versus sitagliptin once-daily as add-on to metformin in subjects with type 2 diabetes Author Biostatistics Semaglutide s.c. This confidential document is the property of Novo Nordisk. No unpublished information contained herein may be disclosed without prior written approval from Novo Nordisk. Access to this document must be restricted to relevant parties.This -

November 2000
Vol.XVIII No. 3 NOVEMBER 2000 Scientific Journal of MEDICAL & VISION RESEARCH FOUNDATIONS 18, COLLEGE ROAD, CHENNAI - 600 006, INDIA Presurgical photograph taken at 28 days of life Age 13 months after skin grafting,showing no showing complete left cryptophthalmos. adhesions and good cosmetic outcome. Editorial Perspective — Treatment of Malignant Melanoma of Choroid — Mahesh P Shanmugam Prepucial Skin Graft for Fornicial and Socket Reconstruction in Complete Cryptophthalmos with Congenital Cystic Eye - A Case Report — Nirmala Subramanian, Surbhit Choudhry and Lakshmi Mahesh Detection of Cytomegalovirus (CMV) from Ocular Fluid of Two Patients with Progressive Outer Retinal Necrosis (PORN) — Jyotirmay Biswas, Surbhit Choudhry, K Priya and Lingam Gopal Unilateral Neuroretinitis following Chicken Pox - Report of a Case — Sumeet Chopra, Jyotirmay Biswas, Sudha K Ganesh and Satya Karna Human Genome Project: A Medical Revolution — G Kumaramanickavel Yeast - a Valuable tool for differential diagnosis of glycosuria and galactosuira — S. Ramakrishnan, K.N. Sulochana, R. Punitham and S.B. Vasanthi Last Page — Literature search on the Internet — Rajesh Fogla Editorial The event of this year, some dub it as that of the century _ the unraveling of the Human Genome finds a mention in this issue of Insight also. Dr. Kumaramanickavel has lucidly written about the implications of this discovery to Medicine and in particular Ophthalmology. Scientists especially the Genetic scientists predict the end of the scalpel and the pill. He has also introduced a new term _ Predictive Medicine. The concept is interesting _ predict the onset of the disease and annul it before it occurs. No doubt the darker side of this technology is foreboding to think of,but as Dr. -

Ophthalmic Ultrasound
Policy: 94047 Initial Effective Date: 10/20/1994 SUBJECT: Ophthalmic Ultrasound - A-scan ultrasound biometry - A-scan ultrasound - quantitative Annual Review Date: 11/11/2019 - B-scan ultrasound - Corneal pachymetry - Optical coherence biometry Last Revised Date: 11/11/2019 Definition: Ophthalmic ultrasonography, also known as echography, uses high-frequency sound waves (ultrasound) to produce images of ocular structures. The two main types of ultrasound used in ophthalmologic practice are A-Scan and B- scan. Ophthalmic ultrasound includes the following techniques: • A-scan ultrasound biometry: A-scan (time amplitude scan) ultrasound is a one-dimensional recording of the time taken for echoes to be reflected back to the transducer from surfaces of the eye (cornea, anterior lens, posterior lens, and retina) with vertical spikes that correspond to each tissue interface zone. A-scan ultrasound can be performed using either an applanation or immersion technique. The applanation technique is performed using a probe placed directly on the surface of the cornea. The immersion technique involves placing a saline filled scleral shell between the probe and the eye. Intraocular lens power calculation is the determination of the appropriate intraocular lens prior to cataract surgery. Standard intraocular lens power formulas use axial length and corneal curvature along with an intraocular lens constant to predict postoperative intraocular lens position. Precise ophthalmic biometry is essential to achieve the desired refractive outcome in cataract surgery. In A-scan biometry, axial length is the distance between the corneal and retinal echo. • Quantitative A-scan ultrasound: The other major use of A-scan ultrasonography is to characterize the internal structure of intraocular and orbital lesions. -

190.18 - Serum Iron Studies
Medicare National Coverage Determinations (NCD) Coding Policy Manual and Change Report (ICD-10-CM) 190.18 - Serum Iron Studies HCPCS Codes (Alphanumeric, CPT AMA) Code Description 82728 Ferritin 83540 Iron 83550 Iron Binding capacity 84466 Transferrin ICD-10-CM Codes Covered by Medicare Program The ICD-10-CM codes in the table below can be viewed on CMS’ website as part of Downloads: Lab Code List, at http://www.cms.gov/Medicare/Coverage/CoverageGenInfo/LabNCDsICD10.html Code Description A01.00 Typhoid fever, unspecified A01.01 Typhoid meningitis A01.02 Typhoid fever with heart involvement A01.03 Typhoid pneumonia A01.04 Typhoid arthritis A01.05 Typhoid osteomyelitis A01.09 Typhoid fever with other complications A01.1 Paratyphoid fever A A01.2 Paratyphoid fever B A01.3 Paratyphoid fever C A01.4 Paratyphoid fever, unspecified A02.0 Salmonella enteritis A02.1 Salmonella sepsis A02.20 Localized salmonella infection, unspecified NCD 190.18 January 2021 Changes ICD-10-CM Version – Red Fu Associates, Ltd. January 2021 1 Medicare National Coverage Determinations (NCD) Coding Policy Manual and Change Report (ICD-10-CM) Code Description A02.21 Salmonella meningitis A02.22 Salmonella pneumonia A02.23 Salmonella arthritis A02.24 Salmonella osteomyelitis A02.25 Salmonella pyelonephritis A02.29 Salmonella with other localized infection A02.8 Other specified salmonella infections A02.9 Salmonella infection, unspecified A04.0 Enteropathogenic Escherichia coli infection A04.1 Enterotoxigenic Escherichia coli infection A04.2 Enteroinvasive Escherichia -

A Rare Case of Left Sided Anophthalmos with Congenital
86 P-ISSN 0972-0200 A Rare Case of Left Sided Anophthalmos with Congenital Cystic Eyeball with Right Sided Microphthalmos Umesh Harakuni, Smitha K.S., Nagbhushan Chougule, Madhura Patil, Preetha Sudhakaran, Maria Sequeira Linda Department of Ophthalmology, Jawaharlal Nehru Medical College, Belgaum, Karnataka, India Congenital cystic eye, also known as anophthalmos with cyst, is an extremely rare congenital anomaly, first described by Mann in 1939 with a prevalence of 3 per 1,00,000. Congenital micropthalmos is also a rare condition with prevalence rates of 1.4 - 3.5 per 10,000 births. The objective is to report a Summary case of a 19 year old male who was born to non-consanguineous marriage, presenting with left sided anophthalmos with right sided microphthalmos, with horizontal nystagmus and healed perforated Brief Communication corneal ulcer. Differential diagnosis include encephalocele, dermoid cyst, congenital cystic eye and tumors. Early visual rehabilitation is advised. Delhi J Ophthalmol 2019;29;86-88; Doi http://dx.doi.org/10.7869/djo.430 Keywords: Anophthalmos, Microphthalmos, Congenital cystic eyeball Case Report A 19 year old male patient presented to ophthalmology OPD with the complaints of diminution of vision in both eyes since birth. There was history of fever during the first trimester of pregnancy for which the mother had taken some medication from a local doctor. There was no history of consanguineous marriage, other sibling was normal. No other chronic medical or systemic illness was present. Clinically, there was no evidence of systemic associations like facial defects, webbed hands, colobomatous lids, preauricular tags, hydrocephalus/ microcephaly, seizures or cleft lip.