Diagnostic Codes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diagnosis and Treatment of Perianal Crohn Disease: NASPGHAN Clinical Report and Consensus Statement
CLINICAL REPORT Diagnosis and Treatment of Perianal Crohn Disease: NASPGHAN Clinical Report and Consensus Statement ÃEdwin F. de Zoeten, zBrad A. Pasternak, §Peter Mattei, ÃRobert E. Kramer, and yHoward A. Kader ABSTRACT disease. The first description connecting regional enteritis with Inflammatory bowel disease is a chronic inflammatory disorder of the perianal disease was by Bissell et al in 1934 (2), and since that time gastrointestinal tract that includes both Crohn disease (CD) and ulcerative perianal disease has become a recognized entity and an important colitis. Abdominal pain, rectal bleeding, diarrhea, and weight loss consideration in the diagnosis and treatment of CD. Perianal characterize both CD and ulcerative colitis. The incidence of IBD in the Crohn disease (PCD) is defined as inflammation at or near the United States is 70 to 150 cases per 100,000 individuals and, as with other anus, including tags, fissures, fistulae, abscesses, or stenosis. autoimmune diseases, is on the rise. CD can affect any part of the The symptoms of PCD include pain, itching, bleeding, purulent gastrointestinal tract from the mouth to the anus and frequently will include discharge, and incontinence of stool. perianal disease. The first description connecting regional enteritis with perianal disease was by Bissell et al in 1934, and since that time perianal INCIDENCE AND NATURAL HISTORY disease has become a recognized entity and an important consideration in the Limited pediatric data describe the incidence and prevalence diagnosis and treatment of CD. Perianal Crohn disease (PCD) is defined as of PCD. The incidence of PCD in the pediatric age group has been inflammation at or near the anus, including tags, fissures, fistulae, abscesses, estimated to be between 13.6% and 62% (3). -

Recent Advances in Surgery the Blind-Loop Syndrome After Gastric
Recent advances in surgery Conducted by ALFRED BLALOCK, M.D. The blind-loop syndrome after gastric operations ince the earliest reports by Whitees time, several examples of the blind-loop ANATOMIC CONFIGURATION OF BLIND LOOPS Various examples of gastrointestinal blind and Wangensteen;O a side-arm loop has been employed as in Fig. 1, A, in which the loop is arranged so as to be self-filling. The side loop arrangement is the one which most 849 850 Recent advances in surgery Surgery ;.$ Nouernbcr 1961 & ad cumulated from observations on lesions at differing sites in the gastrointestinal tract. The principles involved apply, with varia- tions, to blind loops at all levels. The best- known feature of the blind-loop syndrome is megaloblastic anemia, which is due to dis- ruption of vitamin BI2 absorption. Normally, dietary vitamin B12 (Castle's extrinsic fac- tor) is absorbed after an incompletely under- stood interaction with intrinsic factor (Fig. 3, A), a mucoprotein secreted by the gastric rnu~osa.*~In man, the principal site of B,, absorption is the ileum.7* Vitamin B,, deficiency can develop by a number of alternative mechanisms. Rarely loops which have caGsed the blind-loop- syndrome.- is there dietary deficiency of this nutritional A, Anastomosis with formation of a self-filled stagnant loop, B, with jejunal diverticulosis, C, factor. Commonly, as in pernicious anemia with intestinal strictures, D, after enteroenteros- (Fig. 3, B) or after total gastrectomy,Sgthere tomies or fistulas, and E, after gastric operation. is absent intrinsic factor due to gastric atrophy or the absence. of the stomach, re- resembles a blind loop which develops after spectively. -

Plugs for Anal Fistula Repair Original Policy Date: November 26, 2014 Effective Date: January 1, 2021 Section: 7.0 Surgery Page: Page 1 of 12
Medical Policy 7.01.123 Plugs for Anal Fistula Repair Original Policy Date: November 26, 2014 Effective Date: January 1, 2021 Section: 7.0 Surgery Page: Page 1 of 12 Policy Statement Biosynthetic fistula plugs, including plugs made of porcine small intestine submucosa or of synthetic material, are considered investigational for the repair of anal fistulas. NOTE: Refer to Appendix A to see the policy statement changes (if any) from the previous version. Policy Guidelines There is a specific CPT code for the use of these plugs in the repair of an anorectal fistula: • 46707: Repair of anorectal fistula with plug (e.g., porcine small intestine submucosa [SIS]) Description Anal fistula plugs (AFPs) are biosynthetic devices used to promote healing and prevent the recurrence of anal fistulas. They are proposed as an alternative to procedures including fistulotomy, endorectal advancement flaps, seton drain placement, and use of fibrin glue in the treatment of anal fistulas. Related Policies • N/A Benefit Application Benefit determinations should be based in all cases on the applicable contract language. To the extent there are any conflicts between these guidelines and the contract language, the contract language will control. Please refer to the member's contract benefits in effect at the time of service to determine coverage or non-coverage of these services as it applies to an individual member. Some state or federal mandates (e.g., Federal Employee Program [FEP]) prohibits plans from denying Food and Drug Administration (FDA)-approved technologies as investigational. In these instances, plans may have to consider the coverage eligibility of FDA-approved technologies on the basis of medical necessity alone. -

Surgery for Colon and Rectal Cancer
Colon and Rectal Surgery Mohammed Bayasi, MD Department of Surgery Colon and Rectal Surgery What is a Colon and Rectal Surgeon? • Fully trained General Surgeon. • Has done additional training in the diseases of colon and rectum. Why Colon and Rectal Surgery? • Surgical and non surgical therapy for multiple diseases. • Chance to help cancer patients by removing tumor, potentially curing them. • Variety of cases, ages and patient populations. • Specialized area. Colorectal Diseases • Colon • Rectum/Anus – Cancer – Hemorrhoids – Diverticulitis – Anal fistula and – Inflammatory Bowel abscess Disease (Crohn, UC) – Anal fissure – Polyps – Prolapse Symptoms/Signs • Pain • Itching • Discharge • Bleeding • Lump Anatomy Lesson Colon • Extracts water and nutrients. • Helps to form and excrete waste. • Stores important bacteria flora. • Length: 1.5 meters long = 4.9 feet = 59 inches Colon Rectum/Anus • The final portion of the colon. • Area contains muscles important in controlling defecation and flatulence. Rectum/Anus When to see a Colon and Rectal Surgeon • Referral from another physician (Gastroenterology, PCP). • Treatment of anorectal diseases. • Blood with stool, abdominal pain, rectal pain. Hemorrhoids • Internal and external. • Cushions of blood vessels. • When enlarged, they cause bleeding and pain. Treatment • Treatment of symptomatic hemorrhoids is directed by the symptoms themselves. It can broadly be categorized into four groups: − Medical therapy − Office-based procedure − Operative therapies − Emergent interventions Anorectal Abscess • It is a collection of pus in the perianal area. Normal • Causes pain and rectal gland drainage, and if it progresses, fever and systemic Abscess infection. • Treated with incision and drainage. Anorectal Fistula • A tunnel between the inside of the anus and the skin. • Causes discharge, pain, and formation of abscess. -

Common Anorectal Conditions
TurkJMedSci 34(2004)285-293 ©TÜB‹TAK PERSPECTIVESINMEDICALSCIENCES CommonAnorectalConditions PravinJ.GUPTA ConsultingProctologistGuptaNursingHome,D/9,Laxminagar,NAGPUR-440022INDIA Received:July12,2004 Anorectaldisordersincludeadiversegroupof dentateorpectinatelinedividesthesquamousepithelium pathologicdisordersthatgeneratesignificantpatient fromthemucosalorcolumnarepithelium.Fourtoeight discomfortanddisability.Althoughthesearefrequently analglandsdrainintothecryptsofMorgagniatthelevel encounteredingeneralmedicalpractice,theyoften ofthedentateline.Mostrectalabscessesandfistulae receiveonlycasualattentionandtemporaryrelief . originateintheseglands.Thedentatelinealsodelineates Diseasesoftherectumandanusarecommon theareawheresensoryfibersend.Abovethedentate phenomena.Theirprevalenceinthegeneralpopulationis line,therectumissuppliedbystretchnervefibers,and probablymuchhigherthanthatseeninclinicalpractice, notpainnervefibers.Thisallowsmanysurgical sincemostpatientswithsymptomsreferabletothe procedurestobeperformedwithoutanesthesiaabovethe anorectumdonotseekmedicalattention. dentateline.Conversely,belowthedentateline,thereis extremesensitivity,andtheperianalareaisoneofthe Asdoctorsoffirstcontact,general(family) mostsensitiveareasofthebody.Theevacuationofbowel practitioners(GPs)frequentlyfacedifficultquestions contentsdependsonactionbythemusclesofboththe concerningtheoptimummanagementofanorectal involuntaryinternalsphincterandthevoluntaryexternal symptoms.Whiletheexaminationanddiagnosisof sphincter. certainanorectaldisorderscanbechallenging,itisa -

Gastroenterology and the Elderly
3 Gastroenterology and the Elderly Thomas W. Sheehy 3.1. Esophagus 3.1.1. Dysphagia Esophageal disorders, such as esophageal motility disorders, infections, tumors, and other diseases, are common in the elderly. In the elderly, dysphagia usually implies organic disease. There are two types: (1) pre-esophageal and (2) esophageal. Both are further subdivided into motor (neuromuscular) or structural (intrinsic and extrinsic) lesions.! 3.1.2. Pre-esophageal Dysphagia Pre-esophageal dysphagia (PED) usually implies neuromuscular disease and may be caused by pseudobular palsy, multiple sclerosis, amy trophic lateral scle rosis, Parkinson's disease, bulbar poliomyelitis, lesions of the glossopharyngeal nerve, myasthenia gravis, and muscular dystrophies. Since PED is due to inability to initiate the swallowing mechanism, food cannot escape from the oropharynx into the esophagus. Such patients usually have more difficulty swallowing liquid THOMAS W. SHEEHY • The University of Alabama in Birmingham, School of Medicine, Department of Medicine; and Medical Services, Veterans Administration Medical Center, Birming ham, Alabama 35233. 87 S. R. Gambert (ed.), Contemporary Geriatric Medicine © Plenum Publishing Corporation 1983 88 THOMAS W. SHEEHY than solids. They sputter or cough during attempts to swallow and often have nasal regurgitation or aspiration of food. 3.1.3. Dysfunction of the Cricopharyngeus Muscle In the elderly, this is one of the more common forms of PED.2 These patients have the sensation of an obstruction in their throat when they attempt to swallow. This is due to incoordination of the cricopharyngeus muscle. When this muscle fails to relax quickly enough during swallowing, food cannot pass freely into the esophagus. If the muscle relaxes promptly but closes too quickly, food is trapped as it attempts to enter the esophagus. -

Crohn's Disease of the Anal Region
Gut: first published as 10.1136/gut.6.6.515 on 1 December 1965. Downloaded from Gut, 1965, 6, 515 Crohn's disease of the anal region B. K. GRAY, H. E. LOCKHART-MUMMERY, AND B. C. MORSON From the Research Department, St. Mark's Hospital, London EDITORIAL SYNOPSIS This paper records for the first time the clinico-pathological picture of Crohn's disease affecting the anal canal. It has long been recognized that anal lesions may precede intestinal Crohn's disease, often by some years, but the specific characteristics of the lesion have not hitherto been described. The differential diagnosis is discussed in detail. In a previous report from this hospital (Morson and types of anal lesion when the patients were first seen Lockhart-Mummery, 1959) the clinical features and were as follows: pathology of the anal lesions of Crohn's disease were described. In that paper reference was made to Anal fistula, single or multiple .............. 13 several patients with anal fissures or fistulae, biopsy Anal fissures ........... ......... 3 of which showed a sarcoid reaction, but in whom Anal fissure and fistula .................... 3 there was no clinical or radiological evidence of Total 19 intra-abdominal Crohn's disease. The opinion was expressed that some of these patients might later The types of fistula included both low level and prove to have intestinal pathology. This present complex high level varieties. The majority had the contribution is a follow-up of these cases as well as clinical features described previously (Morson and of others seen subsequently. Lockhart-Mummery, 1959; Lockhart-Mummery Involvement of the anus in Crohn's disease has and Morson, 1964) which suggest Crohn's disease, http://gut.bmj.com/ been seen at this hospital in three different ways: that is, the lesions had an indolent appearance with 1 Patients who presented with symptoms of irregular undermined edges and absence of indura- intestinal Crohn's disease who, at the same time, ation. -

CDHO Factsheet Ulcerative Colitis
Disease/Medical Condition ULCERATIVE COLITIS Date of Publication: June 14, 2013 (also referred to as “UC”, “idiopathic proctocolitis”, “pancolitis”, and “inflammatory bowel disease” [IBD]; IBD is an umbrella term that also includes Crohn’s disease and indeterminate/undifferentiated IBD) Is the initiation of non-invasive dental hygiene procedures* contra-indicated? No Is medical consult advised? ...................................... No (assuming patient/client is already under medical care for ulcerative colitis). Is the initiation of invasive dental hygiene procedures contra-indicated?** Possibly, but not typically Is medical consult advised? ....................................... Possibly (depends on severity and level of control of the disease, including the presence/absence of oral lesions). Is medical clearance required? .................................. Possibly (e.g., if the disease is unstable — flare-up — and/or there are active oral lesions). Also, medical clearance may be required if patient/client is being treated with medications associated with immunosuppression +/- increased risk of infection (e.g., corticosteroids [e.g., prednisone], azathioprine, 6-mercaptopurine, methotrexate, cyclosporine, sulfasalazine, biologic response modifier drugs [e.g., anti-tumour necrosis factor drugs — anti-TNFs — such as infliximab, adalimumab, certoluzimab, and golimumab, as well as monoclonal antibody drugs such as vedoluzimab], JAK1 inhibitors [e.g., tofacitinib], etc.). Is antibiotic prophylaxis required? ............................. -

Clinical Practice Guideline for the Management of Anorectal Abscess, Fistula-In-Ano, and Rectovaginal Fistula Jon D
PRACTICE GUIDELINES Clinical Practice Guideline for the Management of Anorectal Abscess, Fistula-in-Ano, and Rectovaginal Fistula Jon D. Vogel, M.D. • Eric K. Johnson, M.D. • Arden M. Morris, M.D. • Ian M. Paquette, M.D. Theodore J. Saclarides, M.D. • Daniel L. Feingold, M.D. • Scott R. Steele, M.D. Prepared on behalf of The Clinical Practice Guidelines Committee of the American Society of Colon and Rectal Surgeons he American Society of Colon and Rectal Sur- and submucosal locations.7–11 Anorectal abscess occurs geons is dedicated to ensuring high-quality pa- more often in males than females, and may occur at any Ttient care by advancing the science, prevention, age, with peak incidence among 20 to 40 year olds.4,8–12 and management of disorders and diseases of the co- In general, the abscess is treated with prompt incision lon, rectum, and anus. The Clinical Practice Guide- and drainage.4,6,10,13 lines Committee is charged with leading international Fistula-in-ano is a tract that connects the perine- efforts in defining quality care for conditions related al skin to the anal canal. In patients with an anorec- to the colon, rectum, and anus by developing clinical tal abscess, 30% to 70% present with a concomitant practice guidelines based on the best available evidence. fistula-in-ano, and, in those who do not, one-third will These guidelines are inclusive, not prescriptive, and are be diagnosed with a fistula in the months to years after intended for the use of all practitioners, health care abscess drainage.2,5,8–10,13–16 Although a perianal abscess workers, and patients who desire information about the is defined by the anatomic space in which it forms, a management of the conditions addressed by the topics fistula-in-ano is classified in terms of its relationship to covered in these guidelines. -
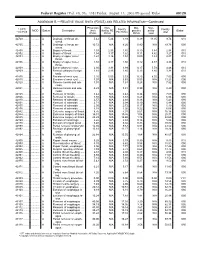
RELATIVE VALUE UNITS (RVUS) and RELATED INFORMATION—Continued
Federal Register / Vol. 68, No. 158 / Friday, August 15, 2003 / Proposed Rules 49129 ADDENDUM B.—RELATIVE VALUE UNITS (RVUS) AND RELATED INFORMATION—Continued Physician Non- Mal- Non- 1 CPT/ Facility Facility 2 MOD Status Description work facility PE practice acility Global HCPCS RVUs RVUs PE RVUs RVUs total total 42720 ....... ........... A Drainage of throat ab- 5.42 5.24 3.93 0.39 11.05 9.74 010 scess. 42725 ....... ........... A Drainage of throat ab- 10.72 N/A 8.26 0.80 N/A 19.78 090 scess. 42800 ....... ........... A Biopsy of throat ................ 1.39 2.35 1.45 0.10 3.84 2.94 010 42802 ....... ........... A Biopsy of throat ................ 1.54 3.17 1.62 0.11 4.82 3.27 010 42804 ....... ........... A Biopsy of upper nose/ 1.24 3.16 1.54 0.09 4.49 2.87 010 throat. 42806 ....... ........... A Biopsy of upper nose/ 1.58 3.17 1.66 0.12 4.87 3.36 010 throat. 42808 ....... ........... A Excise pharynx lesion ...... 2.30 3.31 1.99 0.17 5.78 4.46 010 42809 ....... ........... A Remove pharynx foreign 1.81 2.46 1.40 0.13 4.40 3.34 010 body. 42810 ....... ........... A Excision of neck cyst ........ 3.25 5.05 3.53 0.25 8.55 7.03 090 42815 ....... ........... A Excision of neck cyst ........ 7.07 N/A 5.63 0.53 N/A 13.23 090 42820 ....... ........... A Remove tonsils and ade- 3.91 N/A 3.63 0.28 N/A 7.82 090 noids. -

Anal Fistula
ANAL FISTULA This leaflet is produced by the Department of Colorectal Surgery at Beaumont Hospital supported by an unrestricted grant to better Beaumont from the Beaumont Hospital Cancer Research and Development Trust. This information leaflet has been designed to give you general guidelines and advice regarding your surgery. Not all of this information may be relevant to your circumstances. Please discuss any queries with your doctor or nurse. YOUR TREATMENT EXPLAINED What is a fistula? A fistula is a small tract or tunnel between the back passage and the external skin on the buttocks. This is usually the result of a previous abscess which has drained but which has not fully healed. This results in an intermittent or persistent discharge or leaking of pus or blood. Once a tract has been formed it will remain in place as long as there is pus draining through it. There are different types of fistula. Some develop as a single tract from your rectum (back passage) through to the external skin (simple fistula). Others may branch of into different directions creating more than one tract (complex fistula). How can a fistula be treated? Treatment for a fistula varies from person to person depending on the type of fistula and how each individual fistula responds following surgery. Most of these procedures are carried out as a day case procedure. You will come to the Day ward on the morning of your procedure. You will usually be able to go home the same day once you have recovered from your anaesthetic. The aim of treating a fistula is to drain away any pus allowing inflammation to settle and ultimately the tract to heal. -

Advice Note: Infant Proctocolitis – Fresh Blood PR in a Thriving Infant
Advice Note: Infant proctocolitis – Fresh blood PR in a thriving infant Dear GP, Thank you for your referral. The most common cause for small amounts of fresh blood PR in a well, thriving infant is infant proctocolitis. This is a benign condition in vast majority of cases and does not require a secondary care input. This is a food protein related reaction most commonly caused by cow’s milk protein (CMP) but other common causes include soy, egg, corn and cereal grains. Rarely other foods can trigger a reaction. Typically infants can tolerate the previously causative proteins by 1 year of age. It does not increase the risk of IgE mediated food allergy. It is common in both breast and formula fed babies. There are no diagnostic tests and the diagnosis relies on exclusion of other causes and resolution of symptoms with dietary manipulations. Features of a typical presentation include: Mucousy loose stools with spots or streaks of bright red blood in a well thriving infant Age at presentation: 1 week to 5 months (although can present earlier and later) It can be associated with mild to moderate diarrhea, excessive crying / fussiness/ sleep disturbance, apparent pain on defecation. It may also be associated with mild anemia, hypoalbuminaemia, mild peripheral eosinophilia and family history of same. Features indicating other disorders include: No IM vitamin K at birth Severe bleeding Abdominal distension / tenderness on examination Faltering growth Signs / symptoms of malabsorption Severe diarrhea Vomiting Anaphylaxis Rash, including petechiae, purpura or urticarial Significant anaemia Persistent perianal dermatitis Anal fissures Management: Referral to ED if the infant : o is unwell and or febrile o is haemodynamically unstable o has a history of severe bleeding o has significant vomiting o has abdominal distension or tenderness on examination o has features of anaphylaxis o has severe anaemia Management in the community if the child is well and there are no worrying features on history or examination: o Investigations: .