Stats KID 2003 Severity File
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Recent Advances in Surgery the Blind-Loop Syndrome After Gastric
Recent advances in surgery Conducted by ALFRED BLALOCK, M.D. The blind-loop syndrome after gastric operations ince the earliest reports by Whitees time, several examples of the blind-loop ANATOMIC CONFIGURATION OF BLIND LOOPS Various examples of gastrointestinal blind and Wangensteen;O a side-arm loop has been employed as in Fig. 1, A, in which the loop is arranged so as to be self-filling. The side loop arrangement is the one which most 849 850 Recent advances in surgery Surgery ;.$ Nouernbcr 1961 & ad cumulated from observations on lesions at differing sites in the gastrointestinal tract. The principles involved apply, with varia- tions, to blind loops at all levels. The best- known feature of the blind-loop syndrome is megaloblastic anemia, which is due to dis- ruption of vitamin BI2 absorption. Normally, dietary vitamin B12 (Castle's extrinsic fac- tor) is absorbed after an incompletely under- stood interaction with intrinsic factor (Fig. 3, A), a mucoprotein secreted by the gastric rnu~osa.*~In man, the principal site of B,, absorption is the ileum.7* Vitamin B,, deficiency can develop by a number of alternative mechanisms. Rarely loops which have caGsed the blind-loop- syndrome.- is there dietary deficiency of this nutritional A, Anastomosis with formation of a self-filled stagnant loop, B, with jejunal diverticulosis, C, factor. Commonly, as in pernicious anemia with intestinal strictures, D, after enteroenteros- (Fig. 3, B) or after total gastrectomy,Sgthere tomies or fistulas, and E, after gastric operation. is absent intrinsic factor due to gastric atrophy or the absence. of the stomach, re- resembles a blind loop which develops after spectively. -

Hodgkin Lymphoma
Hodgkin Lymphoma • Lymphoid neoplasm derived from germinal center B cells. • Neoplastic cells (i.e. Hodgkin/Reed-Sternberg/LP cells) comprise the minority of the infiltrate. • Non-neoplastic background inflammatory cells comprise the majority of infiltrate. • Two biologically distinct types: 1. Classical Hodgkin Lymphoma (CHL) 2. Nodular Lymphocyte Predominant Hodgkin Lymphoma (NLPHL) Classical Hodgkin Lymphoma • Neoplastic B (Hodgkin) cells are often take the form of Reed-Sternberg cells or variants – Classic RS, mummified and lacunar cells. • The majority of background, non-neoplastic small lymphocytes are T cells. • Unique immunophenotype that differs from most B cell lymphomas. • Divided into 4 histologic subtypes according to the background milieu: – Nodular Sclerosis – Mixed Cellularity – Lymphocyte Rich – Lymphocyte Deplete CHL - RS Cell Variants Classic RS Cell Lacunar Cells Mummified Cell Hsi ED and Golblum JR. Foundations in Diagnostic Pathology: Hematopathology. 2nd Ed. 2012 CHL - Immunophenotype CD45 CD3 CD20 Pax-5 CD30 CD15 CHL - Histologic Subtypes Nodular Sclerosis • Architecture is effaced by prominent nodules separated by dense bands of collagen. • Mixed inflammatory infiltrate composed of T cells, granulocytes, and histiocytes. • Lacunar variants are the predominant form of RS cells. Mixed Cellularity • Architecture is effaced by a more diffuse infiltrate without bands of fibrosis. • Background of lymphocytes, plasma cells, histiocytes and eosinophils. • Approximately 75% of cases are positive for EBV-encoded RNA or protein (LMP1) Lymphocyte Rich • Architecture is effaced by a nodular to vaguely nodular infiltrate of lymphocytes. • Nodules may contain regressed germinal centers. • The majority of background, non- neoplastic lymphocytes are B cells; T cells form rosettes around neoplastic cells. • Granulocytes and histiocytes are rare. Regressed germinal center Lymphocyte Deplete • Architecture is effaced by disordered fibrosis and necrosis. -

Mimics of Lymphoma
Mimics of Lymphoma L. Jeffrey Medeiros MD Anderson Cancer Center Mimics of Lymphoma Outline Progressive transformation of GCs Infectious mononucleosis Kikuchi-Fujimoto disease Castleman disease Metastatic seminoma Metastatic nasopharyngeal carcinoma Thymoma Myeloid sarcoma Progressive Transformation of Germinal Centers (GC) Clinical Features Occurs in 3-5% of lymph nodes Any age: 15-30 years old most common Usually localized Cervical LNs # 1 Uncommonly patients can present with generalized lymphadenopathy involved by PTGC Fever and other signs suggest viral etiology Progressive Transformation of GCs Different Stages Early Mid-stage Progressive Transformation of GCs Later Stage Progressive Transformation of GCs IHC Findings CD20 CD21 CD10 BCL2 Progressive Transformation of GCs Histologic Features Often involves small area of LN Large nodules (3-5 times normal) Early stage: Irregular shape Blurring between GC and MZ Later stages: GCs break apart Usually associated with follicular hyperplasia Architecture is not replaced Differential Diagnosis of PTGC NLPHL Nodules replace architecture LP (L&H) cells are present Lymphocyte- Nodules replace architecture rich classical Small residual germinal centers HL, nodular RS+H cells (CD15+ CD30+ LCA-) variant Follicular Numerous follicles lymphoma Back-to-back Into perinodal adipose tissue Uniform population of neoplastic cells PTGC –differential dx Nodular Lymphocyte Predominant HL CD20 NLPHL CD3 Lymphocyte-rich Classical HL Nodular variant CD20 CD15 LRCHL Progressive Transformation of GCs BCL2+ is -

Hodgkin's Disease Variant of Richter's Syndrome in Chronic Lymphocytic Leukaemia Patients Previously Treated with Fludarabin
research paper Hodgkin’s disease variant of Richter’s syndrome in chronic lymphocytic leukaemia patients previously treated with fludarabine Dominic Fong,1 Alexandra Kaiser,2 Summary Gilbert Spizzo,1 Guenther Gastl,1 Alexandar Tzankov2 The transformation of chronic lymphocytic leukaemia (CLL) into large-cell 1Division of Haematology and Oncology and lymphoma (Richter’s syndrome, RS) is a well-documented phenomenon. 2Department of Pathology, Innsbruck Medical Only rarely does CLL transform into Hodgkin’s lymphoma (HL). To further University, Innsbruck, Austria analyse the clinico-pathological and genetic findings in the HL variant of RS, we performed a single-institution study in four patients, who developed HL within a mean of 107 months after diagnosis of CLL. All were treated with fludarabine. Three cases were Epstein–Barr virus (EBV)-associated mixed cellularity (MC) HL, the fourth was nodular sclerosis (NS) HL without EBV association. The sites involved by HL included supra- and infradiaphragmal lymph nodes and the tonsils; stage IV disease was also documented. All patients presented with CLL treatment-resistant lymphadenopathies and B- symptoms. In two of the MC cases, molecular analysis performed on CLL samples and microdissected Hodgkin and Reed–Sternberg cells (HRSC) suggested a clonal relationship, while in NS no indication of a clonal relationship was detected. In summary, HL can occur in CLL patients at any Received 15 December 2004; accepted for site, up to 17 years after initial diagnosis, especially after treatment with publication 1 February 2005 fludarabine. The majority present with B-symptoms and CLL treatment- Correspondence: A. Tzankov MD, Department resistant lymphadenopathy, are of the MC type, clonally related to CLL and of Pathology, Innsbruck Medical University, might be triggered by an EBV infection. -

Long-Term Outcome After Neonatal Meconium Obstruction
Long-term Outcome After Neonatal Meconium Obstruction Julie R. Fuchs, MD, and Jacob C. Langer, MD ABSTRACT. Objective. It is unclear whether children meconium ileus and those undergoing resection or enter- with cystic fibrosis (CF) who present with neonatal ostomy. Patients with meconium obstruction who do not meconium ileus have a different long-term outcome from have CF have an excellent long-term prognosis. This those presenting later in childhood with pulmonary com- information will be useful in counseling the families of plications or failure to thrive. We examined a cohort of infants presenting with neonatal meconium obstruction. patients with meconium ileus, and compared their long- Pediatrics 1998;101(4). URL: http://www.pediatrics.org/ term outcome with children who had CF without meco- cgi/content/full/101/4/e7; cystic fibrosis, meconium ileus, nium ileus and neonates who had meconium obstruction meconium plug syndrome. without CF (meconium plug syndrome). Study Design. Comparative study using retrospective and follow-up interview data. ABBREVIATION. CF, cystic fibrosis. Patients. Group 1 consisted of 35 surviving CF pa- tients who presented with meconium ileus between 1966 econium obstruction in the neonate is a and 1992. Two control groups were also studied: 35 age- spectrum of disease that includes meco- and sex-matched CF patients without meconium ileus 1 (group 2), and 12 infants presenting with meconium plug Mnium ileus and meconium plug syndrome. syndrome during the same time period (group 3). Meconium ileus is characterized by extremely viscid, Outcome Measures. Pulmonary, gastrointestinal, nu- protein-rich inspissated meconium causing terminal tritional, and functional status were reviewed, and sur- ileal obstruction, and accounts for approximately gical complications were recorded. -
Diagnostic Codes
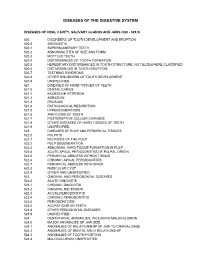
DISEASES OF THE DIGESTIVE SYSTEM DISEASES OF ORAL CAVITY, SALIVARY GLANDS AND JAWS (520 - 529.9) 520 DISORDERS OF TOOTH DEVELOPMENT AND ERUPTION 520.0 ANODONTIA 520.1 SUPERNUMERARY TEETH 520.2 ABNORMALITIES OF SIZE AND FORM 520.3 MOTTLED TEETH 520.4 DISTURBANCES OF TOOTH FORMATION 520.5 HEREDITARY DISTURBANCES IN TOOTH STRUCTURE, NOT ELSEWHERE CLASSIFIED 520.6 DISTURBANCES IN TOOTH ERUPTION 520.7 TEETHING SYNDROME 520.8 OTHER DISORDERS OF TOOTH DEVELOPMENT 520.9 UNSPECIFIED 521 DISEASES OF HARD TISSUES OF TEETH 521.0 DENTAL CARIES 521.1 EXCESSIVE ATTRITION 521.2 ABRASION 521.3 EROSION 521.4 PATHOLOGICAL RESORPTION 521.5 HYPERCEMENTOSIS 521.6 ANKYLOSIS OF TEETH 521.7 POSTERUPTIVE COLOUR CHANGES 521.8 OTHER DISEASES OF HARD TISSUES OF TEETH 521.9 UNSPECIFIED 522 DISEASES OF PULP AND PERIAPICAL TISSUES 522.0 PULPITIS 522.1 NECROSIS OF THE PULP 522.2 PULP DEGENERATION 522.3 ABNORMAL HARD TISSUE FORMATION IN PULP 522.4 ACUTE APICAL PERIODONTITIS OF PULPAL ORIGIN 522.5 PERIAPICAL ABSCESS WITHOUT SINUS 522.6 CHRONIC APICAL PERIODONTITIS 522.7 PERIAPICAL ABSCESS WITH SINUS 522.8 RADICULAR CYST 522.9 OTHER AND UNSPECIFIED 523 GINGIVAL AND PERIODONTAL DISEASES 523.0 ACUTE GINGIVITIS 523.1 CHRONIC GINGIVITIS 523.2 GINGIVAL RECESSION 523.3 ACUTE PERIODONTITIS 523.4 CHRONIC PERIODONTITIS 523.5 PERIODONTOSIS 523.6 ACCRETIONS ON TEETH 523.8 OTHER PERIODONTAL DISEASES 523.9 UNSPECIFIED 524 DENTOFACIAL ANOMALIES, INCLUDING MALOCCLUSION 524.0 MAJOR ANOMALIES OF JAW SIZE 524.1 ANOMALIES OF RELATIONSHIP OF JAW TO CRANIAL BASE 524.2 ANOMALIES OF DENTAL ARCH -

CD20-Positive Peripheral T-Cell Lymphoma: Report of a Case After Nodular Sclerosis Hodgkin’S Disease and Review of the Literature Renee L
CD20-Positive Peripheral T-Cell Lymphoma: Report of a Case after Nodular Sclerosis Hodgkin’s Disease and Review of the Literature Renee L. Mohrmann, M.D., Daniel A. Arber, M.D. Division of Pathology, City of Hope National Medical Center, Duarte, California CASE REPORT We present a case of peripheral T-cell lymphoma co-expressing CD3 and CD20, as well as demon- A 47-year-old man presented in 1993 with a brief strating T-cell receptor gene rearrangement, in a history of right axillary lymph node enlargement patient who had been diagnosed with nodular scle- and mild fatigue. Biopsy showed nodular sclerosis rosis Hodgkin’s disease 5 years previously. Although Hodgkin’s disease. He was treated with six courses 15 cases of CD20-positive T-cell neoplasms have of mechlorethamine, vincristine, procarbazine, been previously reported in the literature, this is the prednisone/doxorubicin, bleomycin, vinblastine first report of CD20-positive T-cell lymphoma oc- chemotherapy over a period of 6 months. Clinical curring subsequent to treatment of Hodgkin’s dis- remission was achieved for 5 years. In early 1998, the patient noticed enlargement of lymph nodes in ease. The current case affords an opportunity to the posterior cervical region, which were followed review the rarely reported expression of CD20 in clinically for several months. Weight loss of 15 lbs., T-cell neoplasms as well as the relationship between fatigue, and flu-like symptoms ensued. The lymph Hodgkin’s disease and subsequently occurring non- nodes became firmer to palpation and were biop- Hodgkin’s lymphomas. In addition, the identifica- sied, showing peripheral T-cell lymphoma, diffuse tion of this case supports the suggestion that the use large-cell type. -

Dysfunction of the Continent Ileostomy: Clinical Features and Bacteriology*
Gut: first published as 10.1136/gut.24.3.193 on 1 March 1983. Downloaded from Gut, 1983, 24, 193-201 Dysfunction of the continent ileostomy: clinical features and bacteriology* DARLENE G KELLY, S F PHILLIPS. K A KELLY, W M WEINSTEIN, AND MARY J R GILCHRIST From the Gastroenterology Unit and Department of Laboratorv Medicine, Mayo Clinic and Mayo Foundation, Rochester, Minnesota, and the Departmlent of Medicine, University of California, Los Angeles, California, USA SUMMARY The pathogenesis and treatment of dysfunction of the continent ileostomy was investigated in 12 patients, five of whom had asymptomatic malabsorption and seven of whom had acute complaints. The number of anaerobic bacteria in jejunal aspirates was increased in patients with pouch malfunction (range 103 to 108/g aspirate), but the microbiology of ileal effluent and the morphology of the ileal mucosa could not be correlated with dysfunction. Bile acid breath tests and lactose tolerance tests were not, however, reliable indicators of jejunal bacterial overgrowth. The symptoms, the malabsorption, and the number of jejunal and ileal anaerobic bacteria decreased in patients during treatment with metronidazole, implicating overgrowth of anaerobic bacterial flora in the pathogenesis of the syndrome. The continent ileostomy (ileal pouch), devised by vitamin B12,9 12 proliferation of anaerobic bacteria http://gut.bmj.com/ Kock,' has been used as an alternative to con- in the pouch,9 inflammation in the pouch,7 ventional ileostomy for selected patients with incontinence,"' difficulty with intubation,1' and ulcerative colitis and familial polyposis.2-5 The bloody discharge.5 We previously reported reservoir functions satisfactorily in most patients, diarrhoea with some features of malabsorption in but malfunction of the 'nipple valve' may occur in up approximately one-third of asymptomatic patients to a third of patients and lead to incontinence. -

CD20 Over-Expression in Hodgkin-Reed-Sternberg Cells of Classical Hodgkin Lymphoma: the Neglected Quest Daniel Benharroch1, Karen Nalbandyan1, Irina Lazarev2
Journal of Cancer 2015, Vol. 6 1155 Ivyspring International Publisher Journal of Cancer 2015; 6(11): 1155-1159. doi: 10.7150/jca.13107 Research Paper CD20 Over-Expression in Hodgkin-Reed-Sternberg Cells of Classical Hodgkin Lymphoma: the Neglected Quest Daniel Benharroch1, Karen Nalbandyan1, Irina Lazarev2 1. Department of Pathology, Soroka University Medical Center, Beer-Sheva and Faculty of Health Sciences, Ben Gurion University of the Negev, Beer-Sheva, Israel 2. Department of Oncology, Soroka University Medical Center, Beer-Sheva and Faculty of Health Sciences, Ben Gurion University of the Negev, Beer-Sheva, Israel Corresponding author: Prof. Daniel Benharroch, Dept. of Pathology, Soroka University Medical Center, P.O.Box 151, Beer-Sheva, 84101, Israel. Tel: 97286400920. Fax:86232770. e-mail: [email protected] © 2015 Ivyspring International Publisher. Reproduction is permitted for personal, noncommercial use, provided that the article is in whole, unmodified, and properly cited. See http://ivyspring.com/terms for terms and conditions. Received: 2015.07.01; Accepted: 2015.08.08; Published: 2015.09.15 Abstract We have scrutinized a previously analyzed cohort of classical Hodgkin lymphoma patients for evidence of a CD20 over-expression. This was pursued in order to determine whether all the 24 (12.6%) CD20+++ patients had clinical and/or biological profiles which would warrant a separate consideration and treatment or would carry a different outcome from our 166 CD20 (-) classical Hodgkin lymphoma patients. Except for an older age and a significantly lower expression of non-sialyl-CD15 antigen, both previously described in classical Hodgkin lymphoma, no justification to exclude these CD20+++ patients from the cohort at large is apparent. -

A Rare Case of Multiple Perforated Jejunal Diverticulae - Case Report
International Journal of Recent Trends in Science And Technology, ISSN 2277-2812 E-ISSN 2249-8109, Volume 10, Issue 3, 2014 pp 458-460 A Rare Case of Multiple Perforated Jejunal Diverticulae - Case Report B. Easwaran 1, G. P. Sekar 2, K. Senthil Kumaran 3, B. Selvaraj 4 1Professor and HOD, 2,4 Associate Professor, 3Assisstant Professor, Department of Surgery, SVMCH, Pondicherry, INDIA. *Corresponding Address: [email protected] Case report Abstract: Jejunal diverticula are very rare with an incidence of less rate 70/Min and BP was 100/60 mm HG. Systemic 1 than 0.5% and are usually asymptomatic. The etiology remains examination was normal. The abdomen was soft, unclear. Since they arise from herniation of the mucosa and distended and tenderness was present in all quadrants. A submucosa through a weak portion of the bowel they are classified as false diverticula of the pulsion type. Complications occur in 10 3 hours later guarding and rigidity also developed to 30% of patients (Ref. 22 ). They are chronic abdominal pain, Blind .clinically free fluid was also present. The bowel sounds loop syndrome, malabsorption, steatorrhoea, megaloblastic anemia, were sluggish. There was tenderness on per rectal hemorrhage, diverticulitis, obstruction, abscess formation, examination. Lab tests revealed impaired renal profile intussusception, volvulus 23 , small bowel obstruction due to 24,25,26,27 (urea 130 mg/d L; creatinine 4.5mg/d L) .Other blood enteroliths and rarely perforation. Jejunal diverticula have a tests were normal. Abdominal x-ray showed air under higher rate of complication than other small bowel diverticula 22 . Diagnosing complicated acute jejunal diverticulosis based on right dome of diaphragm, dilated small bowel loops. -

190.18 - Serum Iron Studies
Medicare National Coverage Determinations (NCD) Coding Policy Manual and Change Report (ICD-10-CM) 190.18 - Serum Iron Studies HCPCS Codes (Alphanumeric, CPT AMA) Code Description 82728 Ferritin 83540 Iron 83550 Iron Binding capacity 84466 Transferrin ICD-10-CM Codes Covered by Medicare Program The ICD-10-CM codes in the table below can be viewed on CMS’ website as part of Downloads: Lab Code List, at http://www.cms.gov/Medicare/Coverage/CoverageGenInfo/LabNCDsICD10.html Code Description A01.00 Typhoid fever, unspecified A01.01 Typhoid meningitis A01.02 Typhoid fever with heart involvement A01.03 Typhoid pneumonia A01.04 Typhoid arthritis A01.05 Typhoid osteomyelitis A01.09 Typhoid fever with other complications A01.1 Paratyphoid fever A A01.2 Paratyphoid fever B A01.3 Paratyphoid fever C A01.4 Paratyphoid fever, unspecified A02.0 Salmonella enteritis A02.1 Salmonella sepsis A02.20 Localized salmonella infection, unspecified NCD 190.18 January 2021 Changes ICD-10-CM Version – Red Fu Associates, Ltd. January 2021 1 Medicare National Coverage Determinations (NCD) Coding Policy Manual and Change Report (ICD-10-CM) Code Description A02.21 Salmonella meningitis A02.22 Salmonella pneumonia A02.23 Salmonella arthritis A02.24 Salmonella osteomyelitis A02.25 Salmonella pyelonephritis A02.29 Salmonella with other localized infection A02.8 Other specified salmonella infections A02.9 Salmonella infection, unspecified A04.0 Enteropathogenic Escherichia coli infection A04.1 Enterotoxigenic Escherichia coli infection A04.2 Enteroinvasive Escherichia -

Hodgkin Reed–Sternberg-Like Cells in Non-Hodgkin Lymphoma
diagnostics Review Hodgkin Reed–Sternberg-Like Cells in Non-Hodgkin Lymphoma 1 2 3, 4,5, Paola Parente , Magda Zanelli , Francesca Sanguedolce *, Luca Mastracci y 1, and Paolo Graziano y 1 Pathology Unit, Fondazione IRCCS Ospedale Casa Sollievo della Sofferenza, 71013 San Giovanni Rotondo, Italy; [email protected] (P.P.); [email protected] (P.G.) 2 Pathology Unit, Azienda USL-IRCCS Reggio Emilia, 42123 Reggio Emilia, Italy; [email protected] 3 Pathology Unit, Azienda Ospedaliera-Universitaria OO.RR, 71100 Foggia, Italy 4 Anatomic Pathology, Ospedale Policlinico San Martino IRCCS, 16132 Genova, Italy; [email protected] 5 Anatomic Pathology, Department of Surgical Sciences and Integrated Diagnostics (DISC), University of Genova, 16132 Genova, Italy * Correspondence: [email protected]; Tel.: +39-0881736315 These Authors contributed equally. y Received: 10 September 2020; Accepted: 24 November 2020; Published: 27 November 2020 Abstract: Reed–Sternberg cells (RSCs) are hallmarks of classic Hodgkin lymphoma (cHL). However, cells with a similar morphology and immunophenotype, so-called Reed–Sternberg-like cells (RSLCs), are occasionally seen in both B cell and T cell non-Hodgkin Lymphomas (NHLs). In NHLs, RSLCs are usually present as scattered elements or in small clusters, and the typical background microenviroment of cHL is usually absent. Nevertheless, in NHLs, the phenotype of RSLCs is very similar to typical RSCs, staining positive for CD30 and EBV, and often for B cell lineage markers, and negative for CD45/LCA. Due to different therapeutic approaches and prognostication, it is mandatory to distinguish between cHL and NHLs. Herein, NHL types in which RSLCs can be detected along with clinicopathological correlation are described.