Hodgkin Reed–Sternberg-Like Cells in Non-Hodgkin Lymphoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

IRF4/DUSP22 Gene Rearrangement by FISH
IRF4/DUSP22 Gene Rearrangement by FISH The IRF4/DUSP22 locus is rearranged in a newly recognized subtype of non-Hodgkin lymphoma, large B-cell lymphoma with IRF4 rearrangement. These lymphomas are uncommon, but are clinically distinct from morphologically similar lymphomas, Tests to Consider including diffuse large B-cell lymphoma, high-grade follicular lymphoma, and pediatric- type follicular lymphoma. The IRF4/DUSP22 locus is also rearranged in a subset of ALK- IRF4/DUSP22 (6p25) Gene Rearrangement negative anaplastic large cell lymphomas (ALCL), where this rearrangement is associated by FISH 3001568 with a signicantly better prognosis. Method: Fluorescence in situ Hybridization (FISH) Test is useful in identifying ALK-negative anaplastic large cell lymphomas and large B- Disease Overview cell lymphoma with IRF4 rearrangement The rearrangement is associated with an improved prognosis Incidence See Related Tests Large B-cell lymphoma with IRF4 rearrangement accounts for <1% of all non-Hodgkin B-cell lymphomas overall More common in younger patients, with an incidence of 5-6% under age 18 IRF4/DUSP22 rearrangement is found in 30% of ALK-negative ALCLs Symptoms/Findings Large B-cell lymphoma with IRF4 rearrangement typically presents with limited stage disease in the head and neck, while the presentation of ALK-negative ALCLs is variable. Disease-Oriented Information Patients with large B-cell lymphoma with IRF4 rearrangement typically have a favorable outcome after treatment. Rearrangement of the IRF4/DUSP22 locus in ALK-negative ALCL is associated with a better prognosis than ALK-negative ALCL without this rearrangement. Test Interpretation Analytical Sensitivity The limit of detection (LOD) for the IRF4/DUSP22 probe was established by calculating the upper limit of the abnormal signal pattern in normal cells using the Microsoft Excel BETAINV function. -

Follicular Lymphoma
Follicular Lymphoma What is follicular lymphoma? Let us explain it to you. www.anticancerfund.org www.esmo.org ESMO/ACF Patient Guide Series based on the ESMO Clinical Practice Guidelines FOLLICULAR LYMPHOMA: A GUIDE FOR PATIENTS PATIENT INFORMATION BASED ON ESMO CLINICAL PRACTICE GUIDELINES This guide for patients has been prepared by the Anticancer Fund as a service to patients, to help patients and their relatives better understand the nature of follicular lymphoma and appreciate the best treatment choices available according to the subtype of follicular lymphoma. We recommend that patients ask their doctors about what tests or types of treatments are needed for their type and stage of disease. The medical information described in this document is based on the clinical practice guidelines of the European Society for Medical Oncology (ESMO) for the management of newly diagnosed and relapsed follicular lymphoma. This guide for patients has been produced in collaboration with ESMO and is disseminated with the permission of ESMO. It has been written by a medical doctor and reviewed by two oncologists from ESMO including the lead author of the clinical practice guidelines for professionals, as well as two oncology nurses from the European Oncology Nursing Society (EONS). It has also been reviewed by patient representatives from ESMO’s Cancer Patient Working Group. More information about the Anticancer Fund: www.anticancerfund.org More information about the European Society for Medical Oncology: www.esmo.org For words marked with an asterisk, a definition is provided at the end of the document. Follicular Lymphoma: a guide for patients - Information based on ESMO Clinical Practice Guidelines – v.2014.1 Page 1 This document is provided by the Anticancer Fund with the permission of ESMO. -

Circle) None Fever Night Sweats Wt Loss Laboratory Studies Hgb WBC Plate
LYMPHOMA STAGING DIAGRAM Instructions: boxed items must be completed History B Sx (Circle) none fever night sweats wt loss Laboratory studies Hgb WBC Plate ECOG performance status g/L x109/L x109/L LDH (patient/upper normal) / CERVICAL PRE-AURICULAR HIV antibody pos neg WALDEYER'S RING UPPER CERVICAL MEDIAN OR LOWER CERVICAL HBsAg pos neg POSTERIOR CERVICAL SUPRACLAVICULAR INFRACLAVICULAR MEDIASTINAL HBcoreAb pos neg PARATRACHEAL MEDIASTINAL AXILLARY Hep C Ab pos neg AXILLARY HILAR RETROCRURAL SPE monoclonal protein pos neg type____________ SPLEEN PARA AORTIC PARA AORTIC MESENTERIC For Hodgkin lymphoma only CELIAC COMMON ILIAC SPLENIC (HEPATIC) HILAR EXTERNAL ILIAC PORTAL Albumin g/L INGUINAL MESENTERIC Lymphs x 109/L INGUINAL FEMORAL OTHER EPITROCHLEAR POPLITEAL Treatment Largest tumor diameter (nearest whole cm) Treatment plan Initial biopsy site Date (d/m/y) / / Histologic diagnosis Doctor in Charge 1 _________________________________________ 2 Reason for referral Bone marrow pos neg not done New Recurrent Follow-up Completed by _______________ Date____________ List all other extranodal sites here 1 2 Complete if diagnosis or stage subsequently changed 3 4 Diagnosis/Stage amended to _________________________ 5 Reason__________________________________________ 6 By_______________________ Date______________ Stage (circle) 0 1 2 3 4 A B E This staging diagram can be found on NOTIFY PATIENT INFORMATION IF STAGE OR H:lym_docs\staging\lymphoma.doc DIAGNOSIS IS AMENDED Form #TH-41 Revised 26 March 2007 LYMPHOMA AND CHRONIC LYMPHOCYTIC LEUKEMIA STAGING SYSTEMS BCCA LYMPHOMA, HODGKIN AND CHRONIC LYMPHOCYTIC LEUKEMIA NON-HODGKIN 1982 STAGE FINDINGS STAGE INVOLVEMENT 0 Lymphocyte count > 5.0 x 109 /L 1 Single lymph node region (1) or one Bone marrow contains 40% extralymphatic site (1E). -

The Lymphoma and Multiple Myeloma Center
The Lymphoma and Multiple Myeloma Center What Sets Us Apart We provide multidisciplinary • Experienced, nationally and internationally recognized physicians dedicated exclusively to treating patients with lymphoid treatment for optimal survival or plasma cell malignancies and quality of life for patients • Cellular therapies such as Chimeric Antigen T-Cell (CAR T) therapy for relapsed/refractory disease with all types and stages of • Specialized diagnostic laboratories—flow cytometry, cytogenetics, and molecular diagnostic facilities—focusing on the latest testing lymphoma, chronic lymphocytic that identifies patients with high-risk lymphoid malignancies or plasma cell dyscrasias, which require more aggresive treatment leukemia, multiple myeloma and • Novel targeted therapies or intensified regimens based on the other plasma cell disorders. cancer’s genetic and molecular profile • Transplant & Cellular Therapy program ranked among the top 10% nationally in patient outcomes for allogeneic transplant • Clinical trials that offer tomorrow’s treatments today www.roswellpark.org/partners-in-practice Partners In Practice medical information for physicians by physicians We want to give every patient their very best chance for cure, and that means choosing Roswell Park Pathology—Taking the best and Diagnosis to a New Level “ optimal front-line Lymphoma and myeloma are a diverse and heterogeneous group of treatment.” malignancies. Lymphoid malignancy classification currently includes nearly 60 different variants, each with distinct pathophysiology, clinical behavior, response to treatment and prognosis. Our diagnostic approach in hematopathology includes the comprehensive examination of lymph node, bone marrow, blood and other extranodal and extramedullary tissue samples, and integrates clinical and diagnostic information, using a complex array of diagnostics from the following support laboratories: • Bone marrow laboratory — Francisco J. -

Low-Grade Non-Hodgkin Lymphoma Book
Low-grade non-Hodgkin lymphoma Low-grade non-Hodgkin lymphoma Follicular lymphoma Mantle cell lymphoma Marginal zone lymphomas Lymphoplasmacytic lymphoma Waldenström’s macroglobulinaemia This book has been researched and written for you by Lymphoma Action, the only UK charity dedicated to people affected by lymphoma. We could not continue to support you, your clinical team and the wider lymphoma community, without the generous donations of our incredible supporters. As an organisation we do not receive any government or NHS funding and so every penny received is truly valued. To make a donation towards our work, please visit lymphoma-action.org.uk/Donate 2 Your lymphoma type and stage Your treatment Key contact Name: Role: Contact details: Job title/role Name and contact details GP Consultant haematologist/ oncologist Clinical nurse specialist or key worker Treatment centre 3 About this book Low-grade (or indolent) non-Hodgkin lymphoma is a type of blood cancer that develops from white blood cells called lymphocytes. It is a broad term that includes lots of different types of lymphoma. This book explains what low-grade non-Hodgkin lymphoma is and how it is diagnosed and treated. It includes tips on coping with treatment and dealing with day-to-day life. The book is split into chapters. You can dip in and out of it and read the sections that are relevant to you at any given time. Important and summary points are written in the chapter colour. Lists practical tips and chapter summaries. Gives space for questions and notes. Lists other resources you might find useful, some of which are online. -

Allogeneic Stem Cell Transplantation in Mantle Cell Lymphoma in the Era of New Drugs and CAR-T Cell Therapy
cancers Review Allogeneic Stem Cell Transplantation in Mantle Cell Lymphoma in the Era of New Drugs and CAR-T Cell Therapy Miriam Marangon 1, Carlo Visco 2 , Anna Maria Barbui 3, Annalisa Chiappella 4, Alberto Fabbri 5, Simone Ferrero 6,7 , Sara Galimberti 8 , Stefano Luminari 9,10 , Gerardo Musuraca 11, Alessandro Re 12 , Vittorio Ruggero Zilioli 13 and Marco Ladetto 14,15,* 1 Department of Hematology, Azienda Sanitaria Universitaria Giuliano Isontina, 34129 Trieste, Italy; [email protected] 2 Section of Hematology, Department of Medicine, University of Verona, 37134 Verona, Italy; [email protected] 3 Hematology Unit, ASST Papa Giovanni XXIII, 24127 Bergamo, Italy; [email protected] 4 Division of Hematology, Fondazione IRCCS, Istituto Nazionale dei Tumori, 20133 Milan, Italy; [email protected] 5 Hematology Division, Department of Oncology, Azienda Ospedaliero-Universitaria Senese, 53100 Siena, Italy; [email protected] 6 Hematology Division, Department of Molecular Biotechnologies and Health Sciences, Università di Torino, 10126 Torino, Italy; [email protected] 7 Hematology 1, AOU Città della Salute e della Scienza di Torino, 10126 Torino, Italy 8 Hematology Unit, Department of Clinical and Experimental Medicine, University of Pisa, 56126 Pisa, Italy; [email protected] 9 Hematology Unit, Azienda Unità Sanitaria Locale IRCCS di Reggio Emilia, 42123 Modena, Italy; [email protected] 10 Surgical, Medical and Dental Department of Morphological Sciences Related -

Hodgkin Lymphoma
Hodgkin Lymphoma • Lymphoid neoplasm derived from germinal center B cells. • Neoplastic cells (i.e. Hodgkin/Reed-Sternberg/LP cells) comprise the minority of the infiltrate. • Non-neoplastic background inflammatory cells comprise the majority of infiltrate. • Two biologically distinct types: 1. Classical Hodgkin Lymphoma (CHL) 2. Nodular Lymphocyte Predominant Hodgkin Lymphoma (NLPHL) Classical Hodgkin Lymphoma • Neoplastic B (Hodgkin) cells are often take the form of Reed-Sternberg cells or variants – Classic RS, mummified and lacunar cells. • The majority of background, non-neoplastic small lymphocytes are T cells. • Unique immunophenotype that differs from most B cell lymphomas. • Divided into 4 histologic subtypes according to the background milieu: – Nodular Sclerosis – Mixed Cellularity – Lymphocyte Rich – Lymphocyte Deplete CHL - RS Cell Variants Classic RS Cell Lacunar Cells Mummified Cell Hsi ED and Golblum JR. Foundations in Diagnostic Pathology: Hematopathology. 2nd Ed. 2012 CHL - Immunophenotype CD45 CD3 CD20 Pax-5 CD30 CD15 CHL - Histologic Subtypes Nodular Sclerosis • Architecture is effaced by prominent nodules separated by dense bands of collagen. • Mixed inflammatory infiltrate composed of T cells, granulocytes, and histiocytes. • Lacunar variants are the predominant form of RS cells. Mixed Cellularity • Architecture is effaced by a more diffuse infiltrate without bands of fibrosis. • Background of lymphocytes, plasma cells, histiocytes and eosinophils. • Approximately 75% of cases are positive for EBV-encoded RNA or protein (LMP1) Lymphocyte Rich • Architecture is effaced by a nodular to vaguely nodular infiltrate of lymphocytes. • Nodules may contain regressed germinal centers. • The majority of background, non- neoplastic lymphocytes are B cells; T cells form rosettes around neoplastic cells. • Granulocytes and histiocytes are rare. Regressed germinal center Lymphocyte Deplete • Architecture is effaced by disordered fibrosis and necrosis. -

Mimics of Lymphoma
Mimics of Lymphoma L. Jeffrey Medeiros MD Anderson Cancer Center Mimics of Lymphoma Outline Progressive transformation of GCs Infectious mononucleosis Kikuchi-Fujimoto disease Castleman disease Metastatic seminoma Metastatic nasopharyngeal carcinoma Thymoma Myeloid sarcoma Progressive Transformation of Germinal Centers (GC) Clinical Features Occurs in 3-5% of lymph nodes Any age: 15-30 years old most common Usually localized Cervical LNs # 1 Uncommonly patients can present with generalized lymphadenopathy involved by PTGC Fever and other signs suggest viral etiology Progressive Transformation of GCs Different Stages Early Mid-stage Progressive Transformation of GCs Later Stage Progressive Transformation of GCs IHC Findings CD20 CD21 CD10 BCL2 Progressive Transformation of GCs Histologic Features Often involves small area of LN Large nodules (3-5 times normal) Early stage: Irregular shape Blurring between GC and MZ Later stages: GCs break apart Usually associated with follicular hyperplasia Architecture is not replaced Differential Diagnosis of PTGC NLPHL Nodules replace architecture LP (L&H) cells are present Lymphocyte- Nodules replace architecture rich classical Small residual germinal centers HL, nodular RS+H cells (CD15+ CD30+ LCA-) variant Follicular Numerous follicles lymphoma Back-to-back Into perinodal adipose tissue Uniform population of neoplastic cells PTGC –differential dx Nodular Lymphocyte Predominant HL CD20 NLPHL CD3 Lymphocyte-rich Classical HL Nodular variant CD20 CD15 LRCHL Progressive Transformation of GCs BCL2+ is -

The Lymphoma Guide Information for Patients and Caregivers
The Lymphoma Guide Information for Patients and Caregivers Ashton, lymphoma survivor This publication was supported by Revised 2016 Publication Update The Lymphoma Guide: Information for Patients and Caregivers The Leukemia & Lymphoma Society wants you to have the most up-to-date information about blood cancer treatment. See below for important new information that was not available at the time this publication was printed. In November 2017, the Food and Drug Administration (FDA) approved obinutuzumab (Gazyva®) in combination with chemotherapy, followed by Gazyva alone in those who responded, for people with previously untreated advanced follicular lymphoma (stage II bulky, III or IV). In November 2017, the Food and Drug Administration (FDA) approved brentuximab vedotin (Adcetris®) for treatment of adult patients with primary cutaneous anaplastic large cell lymphoma (pcALCL) or CD30- expressing mycosis fungoides (MF) who have received prior systemic therapy. In October 2017, the Food and Drug Administration (FDA) approved acalabrutinib (CalquenceTM) for the treatment of adults with mantle cell lymphoma who have received at least one prior therapy. In October 2017, the Food and Drug Administration (FDA) approved axicabtagene ciloleucel (Yescarta™) for the treatment of adult patients with relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy, including diffuse large B-cell lymphoma (DLBCL) not otherwise specified, primary mediastinal large B-cell lymphoma, high-grade B-cell lymphoma, and DLBCL arising from follicular lymphoma. Yescarta is a CD19-directed genetically modified autologous T cell immunotherapy FDA approved. Yescarta is not indicated for the treatment of patients with primary central nervous system lymphoma. In September 2017, the Food and Drug Administration (FDA) approved copanlisib (AliqopaTM) for the treatment of adult patients with relapsed follicular lymphoma (FL) who have received at least two prior systemic therapies. -

Anaplastic Large Cell Lymphoma (ALCL)
Helpline (freephone) 0808 808 5555 [email protected] www.lymphoma-action.org.uk Anaplastic large cell lymphoma (ALCL) This page is about anaplastic large-cell lymphoma (ALCL), a type of T-cell lymphoma. On this page What is ALCL? Who gets it? Symptoms Treatment Relapsed and refractory ALCL Research and targeted treatments We have separate information about the topics in bold font. Please get in touch if you’d like to request copies or if you would like further information about any aspect of lymphoma. Phone 0808 808 5555 or email [email protected]. What is ALCL? Anaplastic large cell lymphoma (ALCL) is a type of T-cell lymphoma – a non-Hodgkin lymphoma that develops from white blood cells called T cells. Under a microscope, the cancerous cells in ALCL look large, undeveloped and very abnormal (‘anaplastic’). There are four main types of ALCL. They have complicated names based on their features and the types of proteins they make: • ALK-positive ALCL (also known as ALK+ ALCL) is the most common type. In ALK-positive ALCL, the abnormal T cells have a genetic change (mutation) that means they make a protein called ‘anaplastic lymphoma kinase’ (ALK). In other words, they test positive for ALK. ALK-positive ALCL is a fast-growing (high-grade) lymphoma. Page 1 of 6 © Lymphoma Action • ALK-negative ALCL (also known as ALK- ALCL) is a high-grade lymphoma that accounts for around 3 in every 10 cases of ALCL. The abnormal T cells do not make the ALK protein – they test negative for ALK. -
Mantle Cell Lymphoma (MCL)
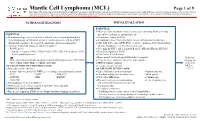
Mantle Cell Lymphoma (MCL) Page 1 of 9 Disclaimer: This algorithm has been developed for MD Anderson using a multidisciplinary approach considering circumstances particular to MD Anderson’s specific patient population, services and structure, and clinical information. This is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient's care. This algorithm should not be used to treat pregnant women. PATHOLOGIC DIAGNOSIS INITIAL EVALUATION ESSENTIAL: ● Physical exam: attention to node-bearing areas, including Waldeyer's ring, ESSENTIAL: size of liver and spleen, and patient’s age ● Hematopathology review of all slides with at least one tumor paraffin block. ● Performance status (ECOG) Hematopathology confirmation of classic versus aggressive variant of MCL ● B symptoms (fever, drenching night sweats, unintentional weight loss) (blastoid/pleomorphic). Re-biopsy if consult material is non-diagnostic. ● CBC with differential, LDH, BUN, creatinine, albumin, AST, total bilirubin, 1 ● Adequate immunophenotype to confirm diagnosis alkaline phosphatase, serum calcium, uric acid ○ Paraffin panel: ● Screening for HIV 1 and 2, hepatitis B and C (HBcAb, HBaAg, HCVAb) - Pan B-cell marker (CD19, CD20, PAX5), CD3, CD5, CD10, and cyclin D1 ● Beta-2 microglobulin (B2M) - Ki-67 (proliferation rate) ● Chest x-ray, PA and lateral or ● Bone marrow bilateral biopsy with unilateral aspirate Induction ○ Flow cytometry immunophenotyping: -

CD20-Negative Diffuse Large B-Cell Lymphomas: Biology and Emerging Therapeutic Options
Expert Review of Hematology ISSN: 1747-4086 (Print) 1747-4094 (Online) Journal homepage: http://www.tandfonline.com/loi/ierr20 CD20-negative diffuse large B-cell lymphomas: biology and emerging therapeutic options Jorge J Castillo, Julio C Chavez, Francisco J Hernandez-Ilizaliturri & Santiago Montes-Moreno To cite this article: Jorge J Castillo, Julio C Chavez, Francisco J Hernandez-Ilizaliturri & Santiago Montes-Moreno (2015) CD20-negative diffuse large B-cell lymphomas: biology and emerging therapeutic options, Expert Review of Hematology, 8:3, 343-354, DOI: 10.1586/17474086.2015.1007862 To link to this article: http://dx.doi.org/10.1586/17474086.2015.1007862 Published online: 01 Feb 2015. Submit your article to this journal Article views: 165 View related articles View Crossmark data Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=ierr20 Download by: [North Shore Med Ctr], [Jorge Castillo] Date: 16 March 2016, At: 07:44 Review CD20-negative diffuse large B-cell lymphomas: biology and emerging therapeutic options Expert Rev. Hematol. 8(3), 343–354 (2015) Jorge J Castillo*1, CD20-negative diffuse large B-cell lymphoma (DLBCL) is a rare and heterogeneous group of Julio C Chavez2, lymphoproliferative disorders. Known variants of CD20-negative DLBCL include plasmablastic Francisco J lymphoma, primary effusion lymphoma, large B-cell lymphoma arising in human herpesvirus 8-associated multicentric Castleman disease and anaplastic lymphoma kinase-positive DLBCL. Hernandez-Ilizaliturri3 Given the lack of CD20 expression, atypical cellular morphology and aggressive clinical and Santiago 4 behavior characterized by chemotherapy resistance and inferior survival rates, CD20-negative Montes-Moreno DLBCL represents a challenge from the diagnostic and therapeutic perspectives.