Mimics of Lymphoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hodgkin Lymphoma
Hodgkin Lymphoma • Lymphoid neoplasm derived from germinal center B cells. • Neoplastic cells (i.e. Hodgkin/Reed-Sternberg/LP cells) comprise the minority of the infiltrate. • Non-neoplastic background inflammatory cells comprise the majority of infiltrate. • Two biologically distinct types: 1. Classical Hodgkin Lymphoma (CHL) 2. Nodular Lymphocyte Predominant Hodgkin Lymphoma (NLPHL) Classical Hodgkin Lymphoma • Neoplastic B (Hodgkin) cells are often take the form of Reed-Sternberg cells or variants – Classic RS, mummified and lacunar cells. • The majority of background, non-neoplastic small lymphocytes are T cells. • Unique immunophenotype that differs from most B cell lymphomas. • Divided into 4 histologic subtypes according to the background milieu: – Nodular Sclerosis – Mixed Cellularity – Lymphocyte Rich – Lymphocyte Deplete CHL - RS Cell Variants Classic RS Cell Lacunar Cells Mummified Cell Hsi ED and Golblum JR. Foundations in Diagnostic Pathology: Hematopathology. 2nd Ed. 2012 CHL - Immunophenotype CD45 CD3 CD20 Pax-5 CD30 CD15 CHL - Histologic Subtypes Nodular Sclerosis • Architecture is effaced by prominent nodules separated by dense bands of collagen. • Mixed inflammatory infiltrate composed of T cells, granulocytes, and histiocytes. • Lacunar variants are the predominant form of RS cells. Mixed Cellularity • Architecture is effaced by a more diffuse infiltrate without bands of fibrosis. • Background of lymphocytes, plasma cells, histiocytes and eosinophils. • Approximately 75% of cases are positive for EBV-encoded RNA or protein (LMP1) Lymphocyte Rich • Architecture is effaced by a nodular to vaguely nodular infiltrate of lymphocytes. • Nodules may contain regressed germinal centers. • The majority of background, non- neoplastic lymphocytes are B cells; T cells form rosettes around neoplastic cells. • Granulocytes and histiocytes are rare. Regressed germinal center Lymphocyte Deplete • Architecture is effaced by disordered fibrosis and necrosis. -

Kaposi Sarcoma-Associated Herpesvirus Uals Were 2 to 16 Times More Likely to Develop Kaposi Sarcoma Than Were Uninfected Individuals
Report on Carcinogens, Fourteenth Edition For Table of Contents, see home page: http://ntp.niehs.nih.gov/go/roc Kaposi Sarcoma-Associated Herpesvirus uals were 2 to 16 times more likely to develop Kaposi sarcoma than were uninfected individuals. In some studies, the risk of Kaposi sar- CAS No.: none assigned coma increased with increasing viral load of KSHV (Sitas et al. 1999, Known to be a human carcinogen Newton et al. 2003a,b, 2006, Albrecht et al. 2004). Most KSHV-infected patients who develop Kaposi sarcoma have Also known as KSHV or human herpesvirus 8 (HHV-8) immune systems compromised either by HIV-1 infection or as a re- Carcinogenicity sult of drug treatments after organ or tissue transplants. The timing of infection with HIV-1 may also play a role in development of Ka- Kaposi sarcoma-associated herpesvirus (KSHV) is known to be a posi sarcoma. Acquiring HIV-1 infection prior to KSHV infection human carcinogen based on sufficient evidence from studies in hu- may increase the risk of epidemic Kaposi sarcoma by 50% to 100%, mans. This conclusion is based on evidence from epidemiological compared with acquiring HIV-1 infection at the same time as or after and molecular studies, which show that KSHV causes Kaposi sar- KSHV infection. Nevertheless, patients with the classic or endemic coma, primary effusion lymphoma, and a plasmablastic variant of forms of Kaposi sarcoma are not suspected of having suppressed im- multicentric Castleman disease, and on supporting mechanistic data. mune systems, suggesting that immunosuppression is not required KSHV causes cancer, primarily but not exclusively in people with for development of Kaposi sarcoma. -

Histiocytic and Dendritic Cell Lesions
1/18/2019 Histiocytic and Dendritic Cell Lesions L. Jeffrey Medeiros, MD MD Anderson Cancer Center Outline 2016 classification of Histiocyte Society Langerhans cell histiocytosis / sarcoma Erdheim-Chester disease Juvenile xanthogranuloma Malignant histiocytosis Histiocytic sarcoma Interdigitating dendritic cell sarcoma Follicular dendritic cell sarcoma Rosai-Dorfman disease Hemophagocytic lymphohistiocytosis Writing Group of the Histiocyte Society 1 1/18/2019 Major Groups of Histiocytic Lesions Group Name L Langerhans-related C Cutaneous and mucocutaneous M Malignant histiocytosis R Rosai-Dorfman disease H Hemophagocytic lymphohistiocytosis Blood 127: 2672, 2016 L Group Langerhans cell histiocytosis Indeterminate cell tumor Erdheim-Chester disease S100 Normal Langerhans cells Langerhans Cell Histiocytosis “Old” Terminology Eosinophilic granuloma Single lesion of bone, LN, or skin Hand-Schuller-Christian disease Lytic lesions of skull, exopthalmos, and diabetes insipidus Sidney Farber Letterer-Siwe disease 1903-1973 Widespread visceral disease involving liver, spleen, bone marrow, and other sites Histiocytosis X Umbrella term proposed by Sidney Farber and then Lichtenstein in 1953 Louis Lichtenstein 1906-1977 2 1/18/2019 Langerhans Cell Histiocytosis Incidence and Disease Distribution Incidence Children: 5-9 x 106 Adults: 1 x 106 Sites of Disease Poor Prognosis Bones 80% Skin 30% Liver Pituitary gland 25% Spleen Liver 15% Bone marrow Spleen 15% Bone Marrow 15% High-risk organs Lymph nodes 10% CNS <5% Blood 127: 2672, 2016 N Engl J Med -

Hodgkin's Disease Variant of Richter's Syndrome in Chronic Lymphocytic Leukaemia Patients Previously Treated with Fludarabin
research paper Hodgkin’s disease variant of Richter’s syndrome in chronic lymphocytic leukaemia patients previously treated with fludarabine Dominic Fong,1 Alexandra Kaiser,2 Summary Gilbert Spizzo,1 Guenther Gastl,1 Alexandar Tzankov2 The transformation of chronic lymphocytic leukaemia (CLL) into large-cell 1Division of Haematology and Oncology and lymphoma (Richter’s syndrome, RS) is a well-documented phenomenon. 2Department of Pathology, Innsbruck Medical Only rarely does CLL transform into Hodgkin’s lymphoma (HL). To further University, Innsbruck, Austria analyse the clinico-pathological and genetic findings in the HL variant of RS, we performed a single-institution study in four patients, who developed HL within a mean of 107 months after diagnosis of CLL. All were treated with fludarabine. Three cases were Epstein–Barr virus (EBV)-associated mixed cellularity (MC) HL, the fourth was nodular sclerosis (NS) HL without EBV association. The sites involved by HL included supra- and infradiaphragmal lymph nodes and the tonsils; stage IV disease was also documented. All patients presented with CLL treatment-resistant lymphadenopathies and B- symptoms. In two of the MC cases, molecular analysis performed on CLL samples and microdissected Hodgkin and Reed–Sternberg cells (HRSC) suggested a clonal relationship, while in NS no indication of a clonal relationship was detected. In summary, HL can occur in CLL patients at any Received 15 December 2004; accepted for site, up to 17 years after initial diagnosis, especially after treatment with publication 1 February 2005 fludarabine. The majority present with B-symptoms and CLL treatment- Correspondence: A. Tzankov MD, Department resistant lymphadenopathy, are of the MC type, clonally related to CLL and of Pathology, Innsbruck Medical University, might be triggered by an EBV infection. -
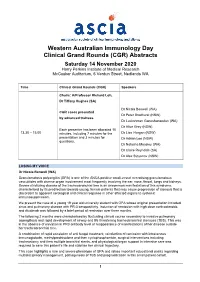
ASCIA WAID Program
Western Australian Immunology Day Clinical Grand Rounds (CGR) Abstracts Saturday 14 November 2020 Harry Perkins Institute of Medical Research McCusker Auditorium, 6 Verdun Street, Nedlands WA Time Clinical Grand Rounds (CGR) Speakers Chairs: A/Professor Richard Loh, Dr Tiffany Hughes (SA) Dr Nicola Benwell (WA) CGR cases presented Dr Peter Bradhurst (NSW) by advanced trainees Dr Luckshman Ganeshanandan (WA) Dr Alice Grey (NSW) Each presenter has been allocated 10 13.30 – 15.00 minutes, including 7 minutes for the Dr Lisa Horgan (NSW) presentation and 3 minutes for Dr Adrian Lee (NSW) questions. Dr Natasha Moseley (WA) Dr Claire Reynolds (SA) Dr Alex Stoyanov (NSW) LOSING MY VOICE Dr Nicola Benwell (WA) Granulomatosis polyangiitis (GPA) is one of the ANCA positive small-vessel necrotising granulomatous vasculitides with diverse organ involvement most frequently involving the ear, nose, throat, lungs and kidneys. Severe stricturing disease of the tracheobronchial tree is an uncommon manifestation of this syndrome, characterised by its predilection towards young, female patients that may cause progression of stenosis that is discordant to apparent serological and clinical response in other affected organs to systemic immunosuppression. We present the case of a young 19 year old university student with GPA whose original presentation included sinus and pulmonary disease with PR-3 seropositivity. Induction of remission with high dose corticosteroids and rituximab was followed by a brief period of remission over three months. The following 2 months were characterised by fluctuating clinical course secondary to invasive pulmonary aspergillosis and rapid development of airway and life threatening tracheobronchial stenoses (TBS). This was in the absence of elevation in PR3 antibody level or reappearance of manifestations of her disease outside her tracheobronchial tree. -

Solitary Plasmacytoma: a Review of Diagnosis and Management
Current Hematologic Malignancy Reports (2019) 14:63–69 https://doi.org/10.1007/s11899-019-00499-8 MULTIPLE MYELOMA (P KAPOOR, SECTION EDITOR) Solitary Plasmacytoma: a Review of Diagnosis and Management Andrew Pham1 & Anuj Mahindra1 Published online: 20 February 2019 # Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Purpose of Review Solitary plasmacytoma is a rare plasma cell dyscrasia, classified as solitary bone plasmacytoma or solitary extramedullary plasmacytoma. These entities are diagnosed by demonstrating infiltration of a monoclonal plasma cell population in a single bone lesion or presence of plasma cells involving a soft tissue mass, respectively. Both diseases represent a single localized process without significant plasma cell infiltration into the bone marrow or evidence of end organ damage. Clinically, it is important to classify plasmacytoma as having completely undetectable bone marrow involvement versus minimal marrow involvement. Here, we discuss the diagnosis, management, and prognosis of solitary plasmacytoma. Recent Findings There have been numerous therapeutic advances in the treatment of multiple myeloma over the last few years. While the treatment paradigm for solitary plasmacytoma has not changed significantly over the years, progress has been made with regard to diagnostic tools available that can risk stratify disease, offer prognostic value, and discern solitary plasmacytoma from quiescent or asymptomatic myeloma at the time of diagnosis. Summary Despite various studies investigating the use of systemic therapy or combined modality therapy for the treatment of plasmacytoma, radiation therapy remains the mainstay of therapy. Much of the recent advancement in the management of solitary plasmacytoma has been through the development of improved diagnostic techniques. -

Japanese Variant of Multicentric Castleman's Disease
J Clin Exp Hematop Vol. 53, No. 1, June 2013 Case Study Japanese Variant of Multicentric Castleman’s Disease Associated With Serositis and Thrombocytopenia ― A Report of Two Cases: Is TAFRO Syndrome (Castleman- Kojima Disease) a Distinct Clinicopathological Entity? Yasufumi Masaki,1) Akio Nakajima,1) Haruka Iwao,1) Nozomu Kurose,2) Tomomi Sato,1) Takuji Nakamura,1) Miyuki Miki,1) Tomoyuki Sakai,1) Takafumi Kawanami,1) Toshioki Sawaki,1) Yoshimasa Fujita,1) Masao Tanaka,1) Toshihiro Fukushima,1) Toshiro Okazaki,1) and Hisanori Umehara1) Multicentric Castleman’s disease (MCD) is a polyclonal lymphoproliferative disorder that manifests as marked hyper-g- globulinemia, severe inflammation, anemia, and thrombocytosis. Recently, Takai et al. reported a new disease concept, TAFRO syndrome, named from thrombocytopenia, anasarca, fever, reticulin fibrosis, and organomegaly. Furthermore, Kojima et al. reported Japanese MCD cases with effusion and thrombocytopenia (Castleman-Kojima disease). Here, we report two cases of MCD associated with marked pleural effusion, ascites, and thrombocytopenia, and discuss the independence of the TAFRO syndrome (Castleman-Kojima disease). Case 1: A 57-year-old woman had fever, anemia, anasarca, and some small cervical lymphadenopathy. Although she had been administered steroid therapy, and full-coverage antibiotics, her general condition, including fever, systemic inflammation, and anasarca, deteriorated steadily. We administered chemotherapy [CHOEP (cyclo- phosphamide, doxorubicin, vincristine, etoposide, and prednisolone) regimen], but despite a transient improvement, she died due to septic shock. Case 2: A 73-year-old man with a history of aplastic anemia and remission presented with fever, severe inflammation, and anasarca. Prednisolone was administered (15 mg daily), and his hyperinflammation once improved. -

CD20-Positive Peripheral T-Cell Lymphoma: Report of a Case After Nodular Sclerosis Hodgkin’S Disease and Review of the Literature Renee L
CD20-Positive Peripheral T-Cell Lymphoma: Report of a Case after Nodular Sclerosis Hodgkin’s Disease and Review of the Literature Renee L. Mohrmann, M.D., Daniel A. Arber, M.D. Division of Pathology, City of Hope National Medical Center, Duarte, California CASE REPORT We present a case of peripheral T-cell lymphoma co-expressing CD3 and CD20, as well as demon- A 47-year-old man presented in 1993 with a brief strating T-cell receptor gene rearrangement, in a history of right axillary lymph node enlargement patient who had been diagnosed with nodular scle- and mild fatigue. Biopsy showed nodular sclerosis rosis Hodgkin’s disease 5 years previously. Although Hodgkin’s disease. He was treated with six courses 15 cases of CD20-positive T-cell neoplasms have of mechlorethamine, vincristine, procarbazine, been previously reported in the literature, this is the prednisone/doxorubicin, bleomycin, vinblastine first report of CD20-positive T-cell lymphoma oc- chemotherapy over a period of 6 months. Clinical curring subsequent to treatment of Hodgkin’s dis- remission was achieved for 5 years. In early 1998, the patient noticed enlargement of lymph nodes in ease. The current case affords an opportunity to the posterior cervical region, which were followed review the rarely reported expression of CD20 in clinically for several months. Weight loss of 15 lbs., T-cell neoplasms as well as the relationship between fatigue, and flu-like symptoms ensued. The lymph Hodgkin’s disease and subsequently occurring non- nodes became firmer to palpation and were biop- Hodgkin’s lymphomas. In addition, the identifica- sied, showing peripheral T-cell lymphoma, diffuse tion of this case supports the suggestion that the use large-cell type. -

Diagnosis and Management of Castleman Disease Jacob D
Castleman disease is an uncommon and heterogeneous lymphoproliferative disorder for which management is rapidly evolving. Gum Drop Mushrooms. Photograph courtesy of Sherri Damlo. www.damloedits.com. Diagnosis and Management of Castleman Disease Jacob D. Soumerai, MD, Aliyah R. Sohani, MD, and Jeremy S. Abramson, MD Background: Castleman disease is an uncommon lymphoproliferative disorder characterized as either unicentric or multicentric. Unicentric Castleman disease (UCD) is localized and carries an excellent prognosis, whereas multicentric Castleman disease (MCD) is a systemic disease occurring most commonly in the setting of HIV infection and is associated with human herpesvirus 8. MCD has been associated with considerable morbidity and mortality, and the therapeutic landscape for its management continues to evolve. Methods: The available medical literature on UCD and MCD was reviewed. The clinical presentation and pathological diagnosis of Castleman disease was reviewed, along with associated disorders such as certain malignancies and autoimmune complications. Results: Surgical resection remains the standard therapy for UCD, while systemic therapies are required for the management of MCD. Rituximab monotherapy is the mainstay of therapy; however, novel therapies targeting interleukin 6 may represent a treatment option in the near future. Antiviral strategies as well as single-agent and combination chemotherapy with glucocorticoids are established systemic therapies. The management of Castleman disease also requires careful attention to potential concomitant infections, malignancies, and associated syndromes. Conclusions: UCD and MCD constitute uncommon but well-defined clinicopathologic entities. Although UCD is typically well controlled with local therapy, MCD continues to pose formidable challenges in management. We address historical chemotherapy-based approaches to this disease as well as recently developed targeted therapies, including rituximab and siltuximab, that have improved the outcome for newly diagnosed patients. -

CD20 Over-Expression in Hodgkin-Reed-Sternberg Cells of Classical Hodgkin Lymphoma: the Neglected Quest Daniel Benharroch1, Karen Nalbandyan1, Irina Lazarev2
Journal of Cancer 2015, Vol. 6 1155 Ivyspring International Publisher Journal of Cancer 2015; 6(11): 1155-1159. doi: 10.7150/jca.13107 Research Paper CD20 Over-Expression in Hodgkin-Reed-Sternberg Cells of Classical Hodgkin Lymphoma: the Neglected Quest Daniel Benharroch1, Karen Nalbandyan1, Irina Lazarev2 1. Department of Pathology, Soroka University Medical Center, Beer-Sheva and Faculty of Health Sciences, Ben Gurion University of the Negev, Beer-Sheva, Israel 2. Department of Oncology, Soroka University Medical Center, Beer-Sheva and Faculty of Health Sciences, Ben Gurion University of the Negev, Beer-Sheva, Israel Corresponding author: Prof. Daniel Benharroch, Dept. of Pathology, Soroka University Medical Center, P.O.Box 151, Beer-Sheva, 84101, Israel. Tel: 97286400920. Fax:86232770. e-mail: [email protected] © 2015 Ivyspring International Publisher. Reproduction is permitted for personal, noncommercial use, provided that the article is in whole, unmodified, and properly cited. See http://ivyspring.com/terms for terms and conditions. Received: 2015.07.01; Accepted: 2015.08.08; Published: 2015.09.15 Abstract We have scrutinized a previously analyzed cohort of classical Hodgkin lymphoma patients for evidence of a CD20 over-expression. This was pursued in order to determine whether all the 24 (12.6%) CD20+++ patients had clinical and/or biological profiles which would warrant a separate consideration and treatment or would carry a different outcome from our 166 CD20 (-) classical Hodgkin lymphoma patients. Except for an older age and a significantly lower expression of non-sialyl-CD15 antigen, both previously described in classical Hodgkin lymphoma, no justification to exclude these CD20+++ patients from the cohort at large is apparent. -

Hodgkin Reed–Sternberg-Like Cells in Non-Hodgkin Lymphoma
diagnostics Review Hodgkin Reed–Sternberg-Like Cells in Non-Hodgkin Lymphoma 1 2 3, 4,5, Paola Parente , Magda Zanelli , Francesca Sanguedolce *, Luca Mastracci y 1, and Paolo Graziano y 1 Pathology Unit, Fondazione IRCCS Ospedale Casa Sollievo della Sofferenza, 71013 San Giovanni Rotondo, Italy; [email protected] (P.P.); [email protected] (P.G.) 2 Pathology Unit, Azienda USL-IRCCS Reggio Emilia, 42123 Reggio Emilia, Italy; [email protected] 3 Pathology Unit, Azienda Ospedaliera-Universitaria OO.RR, 71100 Foggia, Italy 4 Anatomic Pathology, Ospedale Policlinico San Martino IRCCS, 16132 Genova, Italy; [email protected] 5 Anatomic Pathology, Department of Surgical Sciences and Integrated Diagnostics (DISC), University of Genova, 16132 Genova, Italy * Correspondence: [email protected]; Tel.: +39-0881736315 These Authors contributed equally. y Received: 10 September 2020; Accepted: 24 November 2020; Published: 27 November 2020 Abstract: Reed–Sternberg cells (RSCs) are hallmarks of classic Hodgkin lymphoma (cHL). However, cells with a similar morphology and immunophenotype, so-called Reed–Sternberg-like cells (RSLCs), are occasionally seen in both B cell and T cell non-Hodgkin Lymphomas (NHLs). In NHLs, RSLCs are usually present as scattered elements or in small clusters, and the typical background microenviroment of cHL is usually absent. Nevertheless, in NHLs, the phenotype of RSLCs is very similar to typical RSCs, staining positive for CD30 and EBV, and often for B cell lineage markers, and negative for CD45/LCA. Due to different therapeutic approaches and prognostication, it is mandatory to distinguish between cHL and NHLs. Herein, NHL types in which RSLCs can be detected along with clinicopathological correlation are described. -

Hodgkin Lymphoma
Hodgkin Lymphoma Zach, Hodgkin lymphoma survivor Revised 2013 A Message From John Walter President and CEO of The Leukemia & Lymphoma Society The Leukemia & Lymphoma Society (LLS) believes we are living at an extraordinary moment. LLS is committed to bringing you the most up-to-date blood cancer information. We know how important it is for you to have an accurate understanding of your diagnosis, treatment and support options. An important part of our mission is bringing you the latest information about advances in treatment for Hodgkin lymphoma, so you can work with your healthcare team to determine the best options for the best outcomes. Our vision is that one day the great majority of people who have been diagnosed with Hodgkin lymphoma will be cured or will be able to manage their disease with a good quality of life. We hope that the information in this publication will help you along your journey. LLS is the world’s largest voluntary health organization dedicated to funding blood cancer research, education and patient services. Since 1954, LLS has been a driving force behind almost every treatment breakthrough for patients with blood cancers, and we have awarded almost $1 billion to fund blood cancer research. Our commitment to pioneering science has contributed to an unprecedented rise in survival rates for people with many different blood cancers. Until there is a cure, LLS will continue to invest in research, patient support programs and services that improve the quality of life for patients and families. We wish you well. John