Histiocytic and Dendritic Cell Lesions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Best Diagnosis Is: A
DErmatopathology Diagnosis The best diagnosis is: a. eruptive xanthomacopy H&E, original magnification ×200. b. juvenile xanthogranuloma c. Langerhans cell histiocytosis d. reticulohistiocytomanot e. Rosai-Dorfman disease Do CUTIS H&E, original magnification ×600. PLEASE TURN TO PAGE 39 FOR DERMATOPATHOLOGY DIAGNOSIS DISCUSSION Alyssa Miceli, DO; Nathan Cleaver, DO; Amy Spizuoco, DO Dr. Miceli is from the College of Osteopathic Medicine, New York Institute of Technology, Old Westbury. Drs. Cleaver and Spizuoco are from Ackerman Academy of Dermatopathology, New York, New York. The authors report no conflict of interest. Correspondence: Amy Spizuoco, DO, Ackerman Academy of Dermatopathology, 145 E 32nd Street, 10th Floor, New York, NY 10016 ([email protected]). 16 CUTIS® WWW.CUTIS.COM Copyright Cutis 2015. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher. Dermatopathology Diagnosis Discussion rosai-Dorfman Disease osai-Dorfman disease (RDD), also known as negative staining for CD1a on immunohistochemis- sinus histiocytosis with massive lymphade- try. Lymphocytes and plasma cells often are admixed nopathy, is a rare benign histioproliferative with the Rosai-Dorfman cells, and neutrophils and R 1 4 disorder of unknown etiology. Clinically, it is most eosinophils also may be present in the infiltrate. frequently characterized by massive painless cervical The histologic hallmark of RDD is emperipolesis, lymphadenopathy with other systemic manifesta- a phenomenon whereby inflammatory cells such as tions, including fever, night sweats, and weight loss. lymphocytes and plasma cells reside intact within Accompanying laboratory findings include leukocyto- the cytoplasm of histiocytes (Figure 2).5 sis with neutrophilia, elevated erythrocyte sedimenta- The histologic differential diagnosis of cutaneous tion rate, and polyclonal hypergammaglobulinemia. -

WSC 10-11 Conf 7 Layout Master
The Armed Forces Institute of Pathology Department of Veterinary Pathology Conference Coordinator Matthew Wegner, DVM WEDNESDAY SLIDE CONFERENCE 2010-2011 Conference 7 29 September 2010 Conference Moderator: Thomas Lipscomb, DVM, Diplomate ACVP CASE I: 598-10 (AFIP 3165072). sometimes contain many PAS-positive granules which are thought to be phagocytic debris and possibly Signalment: 14-month-old , female, intact, Boxer dog phagocytized organisms that perhaps Boxers and (Canis familiaris). French bulldogs are not able to process due to a genetic lysosomal defect.1 In recent years, the condition has History: Intestine and colon biopsies were submitted been successfully treated with enrofloxacin2 and a new from a patient with chronic diarrhea. report indicates that this treatment correlates with eradication of intramucosal Escherichia coli, and the Gross Pathology: Not reported. few cases that don’t respond have an enrofloxacin- resistant strain of E. coli.3 Histopathologic Description: Colon: The small intestine is normal but the colonic submucosa is greatly The histiocytic influx is reportedly centered in the expanded by swollen, foamy/granular histiocytes that submucosa and into the deep mucosa and may expand occasionally contain a large clear vacuole. A few of through the muscular wall to the serosa and adjacent these histiocytes are in the deep mucosal lamina lymph nodes.1 Mucosal biopsies only may miss the propria as well, between the muscularis mucosa and lesions. Mucosal ulceration progresses with chronicity the crypts. Many scattered small lymphocytes with from superficial erosions to patchy ulcers that stop at plasma cells and neutrophils are also in the submucosa, the submucosa to only patchy intact islands of mucosa. -

FT117 Langerhans Cell Histiocytosis with Histopathological Features
FT117 Langerhans cell histiocytosis with histopathological features, single center experience Histopatolojik özellikleriyle langerhans hücreli histiyositoz, tek merkez deneyimi Fahriye KILINÇ Necmettin Erbakan Üniversitesi, Meram Tıp Fakültesi, Tıbbi Patoloji Anabilim Dalı, Konya Aim: Langerhans cell histiocytosis (LCH) is a rare histiocytic disease, occurring in 2-10 children per million and 1-2 adults per million, and may have a wide variety of clinical manifestations. Infiltration can develop in almost any organ (the most commonly reported organs are bone, skin, lymph nodes, lungs, thymus, liver, spleen, bone marrow and central nervous system). We aimed to evaluate the histopathological features of the lesions and review the literature in pediatric patients referred to our department for pathological examination and diagnosed as LCH. Materials and Methods: Retrospectively, childhood cases diagnosed with LCH in 2012-2019 were screened by hospital automation system. Age, gender, lesion localizations of the cases were recorded and histopathological features were reviewed. Results: 5 male and 5 female total of 10 cases were detected. The youngest 3 were under the age of 1, the oldest was 16 years old. Localization; 6 of the cases were bone (2 femur, 3 skull bone, 1 scapula), 2 skin, 1 bone and lymph node, 1 lung and lymph node. Histopathology revealed histiocytic cells with grooved nuclei, eosinophilic cytoplasm with eosinophils, and neutrophils in some cases. Immunohistochemical CD1a staining was positive in all cases and positivities were present with S100 in applied 9 cases, CD68 in 4. Ki67 proliferation index was studied in 2 patients with bone localization, 15% and 20%. Conclusion: The term LCH is due to the morphological and immunophenotypic similarity of the infiltrating cells of this disease to Langerhans cells specialized as dendritic cells in the skin and mucous membranes. -

Skin Biopsy Diagnosis of Langerhans Cell Neoplasms
Chapter 3 Skin Biopsy Diagnosis of Langerhans Cell Neoplasms Olga L. Bohn, Julie Teruya-Feldstein and Sergio Sanchez-Sosa Additional information is available at the end of the chapter http://dx.doi.org/10.5772/55893 1. Introduction This chapter reviews the clinical presentation, histopathology, immunoprofile and molecular features of Langerhans cell neoplasms of the skin including Langerhans cell histiocytosis (LCH) and its malignant counterpart, Langerhans cell sarcoma (LCS). Biopsy of the skin is a useful method to confirm LCH/LCS diagnosis, as cutaneous involvement is seen in more than 50% cases. Skin can be the only presenting site of LCH, but it is usually seen as an integral part of multisystemic disease involvement. Langerhans cells (LC) are bone marrow-derived antigen presenting cells [1]. Although LC, dendritic cells and monocytic/histiocytic cells share a common multipotential progenitor cells that reside in the bone marrow, to the date, myeloid derived macrophages and dendritic cells constitute divergent lines of differentiation from bone marrow precursors [2]. However, recent evidence demonstrates that LC can be generated from lymphoid-committed CD4low precur‐ sors, suggesting the role of lineage plasticity/ trans-differentiation and clonal infidelity [3-4]. LC can be found in the epidermis and mucosal lining of multiple organs including cervix, vagina, stomach and esophagus. The specific immunophenotypic profile is helpful distin‐ guishing LCs, as they can express CD1a and langerin (CD207); in addition the detection of Birbeck granules, seen in both pathological and resting LC is a prominent feature [5]. LCH encompasses a spectrum of disease characterized by an uncontrolled proliferation of LC [5]. -

An Electron Microscope Study of Histiocyte Response to Ascites Tumor Homografts*
An Electron Microscope Study of Histiocyte Response to Ascites Tumor Homografts* L. J. JOURNEYANDD. B. Aiviosf (Experimental Biology Department, Roswell Park Memorial Institute, fÃujfaln.New York) SUMMARY When the ascites forms of the DBA/2 lymphoma L1210 or the C57BL E.L. 4 lymphoma are injected into C3H mice, host histiocytes (macrophages) accumulate and are responsible for the destruction of a large number of tumor cells. Many of the tumor cells, often apparently intact, are ingested. The ingestion process is rapid and depends upon invagination of an area of the histiocyte with simultaneous projection of cytoplasmic fimbriae which complete the encirclement. The earliest change seen in the enclosed cell is shrinkage; digestion of the cell wall and cytoplasmic elements fol lows. Phagocytosis accounts for only a proportion of the cells destroyed by histiocytes. Other cells are probably destroyed when their cell membrane is broken down in an area in contact with a histiocyte, apparently permitting fusion of the two cytoplasms. Weaver and his colleagues (13) observed that cytes and details some of the concomitant changes host cells were frequently found in close associa occurring in the histiocytes themselves. tion with tumor cells and described death of both host and incompatible tumor cell after a period of MATERIALS AND METHODS contact. Gorer (9) found that the predominant In a series of experiments 20 X IO7 cells from host cell in the ascites fluid during tumor rejection rapidly growing ascites populations of the lympho- was the histiocyte. This finding was confirmed, and mas E. L. 4 or L1210 native to C57BL and DBA/ some quantitative measurements were made by 2, respectively, were injected into the peritoneal one of us (1) and later by Weiser and his col cavity of young adult male C3H/He mice. -

Human Anatomy As Related to Tumor Formation Book Four
SEER Program Self Instructional Manual for Cancer Registrars Human Anatomy as Related to Tumor Formation Book Four Second Edition U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service National Institutesof Health SEER PROGRAM SELF-INSTRUCTIONAL MANUAL FOR CANCER REGISTRARS Book 4 - Human Anatomy as Related to Tumor Formation Second Edition Prepared by: SEER Program Cancer Statistics Branch National Cancer Institute Editor in Chief: Evelyn M. Shambaugh, M.A., CTR Cancer Statistics Branch National Cancer Institute Assisted by Self-Instructional Manual Committee: Dr. Robert F. Ryan, Emeritus Professor of Surgery Tulane University School of Medicine New Orleans, Louisiana Mildred A. Weiss Los Angeles, California Mary A. Kruse Bethesda, Maryland Jean Cicero, ART, CTR Health Data Systems Professional Services Riverdale, Maryland Pat Kenny Medical Illustrator for Division of Research Services National Institutes of Health CONTENTS BOOK 4: HUMAN ANATOMY AS RELATED TO TUMOR FORMATION Page Section A--Objectives and Content of Book 4 ............................... 1 Section B--Terms Used to Indicate Body Location and Position .................. 5 Section C--The Integumentary System ..................................... 19 Section D--The Lymphatic System ....................................... 51 Section E--The Cardiovascular System ..................................... 97 Section F--The Respiratory System ....................................... 129 Section G--The Digestive System ......................................... 163 Section -

Mimics of Lymphoma
Mimics of Lymphoma L. Jeffrey Medeiros MD Anderson Cancer Center Mimics of Lymphoma Outline Progressive transformation of GCs Infectious mononucleosis Kikuchi-Fujimoto disease Castleman disease Metastatic seminoma Metastatic nasopharyngeal carcinoma Thymoma Myeloid sarcoma Progressive Transformation of Germinal Centers (GC) Clinical Features Occurs in 3-5% of lymph nodes Any age: 15-30 years old most common Usually localized Cervical LNs # 1 Uncommonly patients can present with generalized lymphadenopathy involved by PTGC Fever and other signs suggest viral etiology Progressive Transformation of GCs Different Stages Early Mid-stage Progressive Transformation of GCs Later Stage Progressive Transformation of GCs IHC Findings CD20 CD21 CD10 BCL2 Progressive Transformation of GCs Histologic Features Often involves small area of LN Large nodules (3-5 times normal) Early stage: Irregular shape Blurring between GC and MZ Later stages: GCs break apart Usually associated with follicular hyperplasia Architecture is not replaced Differential Diagnosis of PTGC NLPHL Nodules replace architecture LP (L&H) cells are present Lymphocyte- Nodules replace architecture rich classical Small residual germinal centers HL, nodular RS+H cells (CD15+ CD30+ LCA-) variant Follicular Numerous follicles lymphoma Back-to-back Into perinodal adipose tissue Uniform population of neoplastic cells PTGC –differential dx Nodular Lymphocyte Predominant HL CD20 NLPHL CD3 Lymphocyte-rich Classical HL Nodular variant CD20 CD15 LRCHL Progressive Transformation of GCs BCL2+ is -

Kaposi Sarcoma-Associated Herpesvirus Uals Were 2 to 16 Times More Likely to Develop Kaposi Sarcoma Than Were Uninfected Individuals
Report on Carcinogens, Fourteenth Edition For Table of Contents, see home page: http://ntp.niehs.nih.gov/go/roc Kaposi Sarcoma-Associated Herpesvirus uals were 2 to 16 times more likely to develop Kaposi sarcoma than were uninfected individuals. In some studies, the risk of Kaposi sar- CAS No.: none assigned coma increased with increasing viral load of KSHV (Sitas et al. 1999, Known to be a human carcinogen Newton et al. 2003a,b, 2006, Albrecht et al. 2004). Most KSHV-infected patients who develop Kaposi sarcoma have Also known as KSHV or human herpesvirus 8 (HHV-8) immune systems compromised either by HIV-1 infection or as a re- Carcinogenicity sult of drug treatments after organ or tissue transplants. The timing of infection with HIV-1 may also play a role in development of Ka- Kaposi sarcoma-associated herpesvirus (KSHV) is known to be a posi sarcoma. Acquiring HIV-1 infection prior to KSHV infection human carcinogen based on sufficient evidence from studies in hu- may increase the risk of epidemic Kaposi sarcoma by 50% to 100%, mans. This conclusion is based on evidence from epidemiological compared with acquiring HIV-1 infection at the same time as or after and molecular studies, which show that KSHV causes Kaposi sar- KSHV infection. Nevertheless, patients with the classic or endemic coma, primary effusion lymphoma, and a plasmablastic variant of forms of Kaposi sarcoma are not suspected of having suppressed im- multicentric Castleman disease, and on supporting mechanistic data. mune systems, suggesting that immunosuppression is not required KSHV causes cancer, primarily but not exclusively in people with for development of Kaposi sarcoma. -

Progress in Understanding the Pathogenesis of Langerhans Cell Histiocytosis: Back to Histiocytosis X?
review Progress in understanding the pathogenesis of Langerhans cell histiocytosis: back to Histiocytosis X? Marie-Luise Berres,1,2,3,4 Miriam Merad1,2,3 and Carl E. Allen5,6 1Department of Oncological Sciences, Mount Sinai School of Medicine, 2Tisch Cancer Institute, Mount Sinai School of Medicine, 3Immunology Institute, Mount Sinai School of Medicine, New York, NY, USA, 4Department of Internal Medicine III, University Hospital, RWTH Aachen, Aachen, Germany, 5Texas Children’s Cancer Center, and 6Baylor College of Medicine, Houston, TX, USA Summary Langerhans cell histiocytosis (LCH) is the most common his- tiocytic disorder, arising in approximately five children per Langerhans cell histiocytosis (LCH), the most common million, similar in frequency to paediatric Hodgkin lym- histiocytic disorder, is characterized by the accumulation of phoma and acute myeloid leukaemia (AML) (Guyot-Goubin CD1A+/CD207+ mononuclear phagocytes within granuloma- et al, 2008; Stalemark et al, 2008; Salotti et al, 2009). The tous lesions that can affect nearly all organ systems. Histori- median age of presentation is 30 months, though LCH is cally, LCH has been presumed to arise from transformed or reported in adults in approximately one adult per million, pathologically activated epidermal dendritic cells called Lan- both as unrecognized chronic paediatric disease and de novo gerhans cells. However, new evidence supports a model in disease (Baumgartner et al, 1997). There are occasional which LCH occurs as a consequence of a misguided differen- reports of affected non-twin siblings and multiple cases in tiation programme of myeloid dendritic cell precursors. one family, though it is not clear if this is significantly more Genetic, molecular and functional data implicate activation frequent than one would expect by chance (Arico et al, of the ERK signalling pathway at critical stages in myeloid 2005). -

Cutaneous Neonatal Langerhans Cell Histiocytosis
F1000Research 2019, 8:13 Last updated: 18 SEP 2019 SYSTEMATIC REVIEW Cutaneous neonatal Langerhans cell histiocytosis: a systematic review of case reports [version 1; peer review: 1 approved with reservations, 1 not approved] Victoria Venning 1, Evelyn Yhao2,3, Elizabeth Huynh2,3, John W. Frew 2,4 1Prince of Wales Hospital, Randwick, Sydney, NSW, 2033, Australia 2University of New South Wales, Sydney, NSW, 2033, Australia 3Sydney Children's Hospital, Randwick, NSW, 2033, Australia 4Department of Dermatology, Liverpool Hospital, Sydney, Sydney, NSW, 2170, Australia First published: 03 Jan 2019, 8:13 ( Open Peer Review v1 https://doi.org/10.12688/f1000research.17664.1) Latest published: 03 Jan 2019, 8:13 ( https://doi.org/10.12688/f1000research.17664.1) Reviewer Status Abstract Invited Reviewers Background: Cutaneous langerhans cell histiocytosis (LCH) is a rare 1 2 disorder characterized by proliferation of cells with phenotypical characteristics of Langerhans cells. Although some cases spontaneously version 1 resolve, no consistent variables have been identified that predict which published report report cases will manifest with systemic disease later in childhood. 03 Jan 2019 Methods: A systematic review (Pubmed, Embase, Cochrane database and all published abstracts from 1946-2018) was undertaken to collate all reported cases of cutaneous LCH in the international literature. This study 1 Jolie Krooks , Florida Atlantic University, was registered with PROSPERO (CRD42016051952). Descriptive statistics Boca Raton, USA and correlation analyses were undertaken. Bias was analyzed according to Milen Minkov , Teaching Hospital of the GRADE criteria. Medical University of Vienna, Vienna, Austria Results: A total of 83 articles encompassing 128 cases of cutaneous LCH were identified. -

Case Report Congenital Self-Healing Reticulohistiocytosis
Case Report Congenital Self-Healing Reticulohistiocytosis Presented with Multiple Hypopigmented Flat-Topped Papules: A Case Report and Review of Literatures Rawipan Uaratanawong MD*, Tanawatt Kootiratrakarn MD, PhD*, Poonnawis Sudtikoonaseth MD*, Atjima Issara MD**, Pinnaree Kattipathanapong MD* * Institute of Dermatology, Department of Medical Services Ministry of Public Health, Bangkok, Thailand ** Department of Pediatrics, Saraburi Hospital, Sabaruri, Thailand Congenital self-healing reticulohistiocytosis, also known as Hashimoto-Pritzker disease, is a single system Langerhans cell histiocytosis that typically presents in healthy newborns and spontaneously regresses. In the present report, we described a 2-month-old Thai female newborn with multiple hypopigmented flat-topped papules without any internal organ involvement including normal blood cell count, urinary examination, liver and renal functions, bone scan, chest X-ray, abdominal ultrasound, and bone marrow biopsy. The histopathology revealed typical findings of Langerhans cell histiocytosis, which was confirmed by the immunohistochemical staining CD1a and S100. Our patient’s lesions had spontaneously regressed within a few months, and no new lesion recurred after four months follow-up. Keywords: Congenital self-healing reticulohistiocytosis, Congenital self-healing Langerhans cell histiocytosis, Langerhans cell histiocytosis, Hashimoto-Pritzker disease, Birbeck granules J Med Assoc Thai 2014; 97 (9): 993-7 Full text. e-Journal: http://www.jmatonline.com Langerhans cell histiocytosis (LCH) is a multiple hypopigmented flat-topped papules, which clonal proliferative disease of Langerhans cell is a rare manifestation. involving multiple organs, including skin, which is the second most commonly involved organ by following Case Report the skeletal system(1). LCH has heterogeneous clinical A 2-month-old Thai female infant presented manifestations, ranging from benign single system with multiple hypopigmented flat-topped papules since disease to fatal multisystem disease(1-3). -
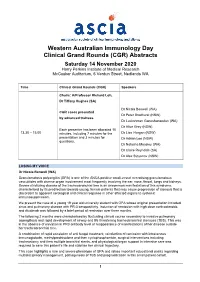
ASCIA WAID Program
Western Australian Immunology Day Clinical Grand Rounds (CGR) Abstracts Saturday 14 November 2020 Harry Perkins Institute of Medical Research McCusker Auditorium, 6 Verdun Street, Nedlands WA Time Clinical Grand Rounds (CGR) Speakers Chairs: A/Professor Richard Loh, Dr Tiffany Hughes (SA) Dr Nicola Benwell (WA) CGR cases presented Dr Peter Bradhurst (NSW) by advanced trainees Dr Luckshman Ganeshanandan (WA) Dr Alice Grey (NSW) Each presenter has been allocated 10 13.30 – 15.00 minutes, including 7 minutes for the Dr Lisa Horgan (NSW) presentation and 3 minutes for Dr Adrian Lee (NSW) questions. Dr Natasha Moseley (WA) Dr Claire Reynolds (SA) Dr Alex Stoyanov (NSW) LOSING MY VOICE Dr Nicola Benwell (WA) Granulomatosis polyangiitis (GPA) is one of the ANCA positive small-vessel necrotising granulomatous vasculitides with diverse organ involvement most frequently involving the ear, nose, throat, lungs and kidneys. Severe stricturing disease of the tracheobronchial tree is an uncommon manifestation of this syndrome, characterised by its predilection towards young, female patients that may cause progression of stenosis that is discordant to apparent serological and clinical response in other affected organs to systemic immunosuppression. We present the case of a young 19 year old university student with GPA whose original presentation included sinus and pulmonary disease with PR-3 seropositivity. Induction of remission with high dose corticosteroids and rituximab was followed by a brief period of remission over three months. The following 2 months were characterised by fluctuating clinical course secondary to invasive pulmonary aspergillosis and rapid development of airway and life threatening tracheobronchial stenoses (TBS). This was in the absence of elevation in PR3 antibody level or reappearance of manifestations of her disease outside her tracheobronchial tree.