Anaplastic Large Cell Lymphoma (ALCL)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Follicular Lymphoma
Follicular Lymphoma What is follicular lymphoma? Let us explain it to you. www.anticancerfund.org www.esmo.org ESMO/ACF Patient Guide Series based on the ESMO Clinical Practice Guidelines FOLLICULAR LYMPHOMA: A GUIDE FOR PATIENTS PATIENT INFORMATION BASED ON ESMO CLINICAL PRACTICE GUIDELINES This guide for patients has been prepared by the Anticancer Fund as a service to patients, to help patients and their relatives better understand the nature of follicular lymphoma and appreciate the best treatment choices available according to the subtype of follicular lymphoma. We recommend that patients ask their doctors about what tests or types of treatments are needed for their type and stage of disease. The medical information described in this document is based on the clinical practice guidelines of the European Society for Medical Oncology (ESMO) for the management of newly diagnosed and relapsed follicular lymphoma. This guide for patients has been produced in collaboration with ESMO and is disseminated with the permission of ESMO. It has been written by a medical doctor and reviewed by two oncologists from ESMO including the lead author of the clinical practice guidelines for professionals, as well as two oncology nurses from the European Oncology Nursing Society (EONS). It has also been reviewed by patient representatives from ESMO’s Cancer Patient Working Group. More information about the Anticancer Fund: www.anticancerfund.org More information about the European Society for Medical Oncology: www.esmo.org For words marked with an asterisk, a definition is provided at the end of the document. Follicular Lymphoma: a guide for patients - Information based on ESMO Clinical Practice Guidelines – v.2014.1 Page 1 This document is provided by the Anticancer Fund with the permission of ESMO. -

Circle) None Fever Night Sweats Wt Loss Laboratory Studies Hgb WBC Plate
LYMPHOMA STAGING DIAGRAM Instructions: boxed items must be completed History B Sx (Circle) none fever night sweats wt loss Laboratory studies Hgb WBC Plate ECOG performance status g/L x109/L x109/L LDH (patient/upper normal) / CERVICAL PRE-AURICULAR HIV antibody pos neg WALDEYER'S RING UPPER CERVICAL MEDIAN OR LOWER CERVICAL HBsAg pos neg POSTERIOR CERVICAL SUPRACLAVICULAR INFRACLAVICULAR MEDIASTINAL HBcoreAb pos neg PARATRACHEAL MEDIASTINAL AXILLARY Hep C Ab pos neg AXILLARY HILAR RETROCRURAL SPE monoclonal protein pos neg type____________ SPLEEN PARA AORTIC PARA AORTIC MESENTERIC For Hodgkin lymphoma only CELIAC COMMON ILIAC SPLENIC (HEPATIC) HILAR EXTERNAL ILIAC PORTAL Albumin g/L INGUINAL MESENTERIC Lymphs x 109/L INGUINAL FEMORAL OTHER EPITROCHLEAR POPLITEAL Treatment Largest tumor diameter (nearest whole cm) Treatment plan Initial biopsy site Date (d/m/y) / / Histologic diagnosis Doctor in Charge 1 _________________________________________ 2 Reason for referral Bone marrow pos neg not done New Recurrent Follow-up Completed by _______________ Date____________ List all other extranodal sites here 1 2 Complete if diagnosis or stage subsequently changed 3 4 Diagnosis/Stage amended to _________________________ 5 Reason__________________________________________ 6 By_______________________ Date______________ Stage (circle) 0 1 2 3 4 A B E This staging diagram can be found on NOTIFY PATIENT INFORMATION IF STAGE OR H:lym_docs\staging\lymphoma.doc DIAGNOSIS IS AMENDED Form #TH-41 Revised 26 March 2007 LYMPHOMA AND CHRONIC LYMPHOCYTIC LEUKEMIA STAGING SYSTEMS BCCA LYMPHOMA, HODGKIN AND CHRONIC LYMPHOCYTIC LEUKEMIA NON-HODGKIN 1982 STAGE FINDINGS STAGE INVOLVEMENT 0 Lymphocyte count > 5.0 x 109 /L 1 Single lymph node region (1) or one Bone marrow contains 40% extralymphatic site (1E). -

HODGKIN LYMPHOMA TREATMENT REGIMENS (Part 1 of 2)
HODGKIN LYMPHOMA TREATMENT REGIMENS (Part 1 of 2) The selection, dosing, and administration of anticancer agents and the management of associated toxicities are complex. Drug dose modifications and schedule and initiation of supportive care interventions are often necessary because of expected toxicities and because of individual patient variability, prior treatment, and comorbidities. Thus, the optimal delivery of anticancer agents requires a healthcare delivery team experienced in the use of such agents and the management of associated toxicities in patients with cancer. The cancer treatment regimens below may include both FDA-approved and unapproved uses/regimens and are provided as references only to the latest treatment strategies. Clinicians must choose and verify treatment options based on the individual patient. NOTE: GREY SHADED BOXES CONTAIN UPDATED REGIMENS. REGIMEN DOSING Classical Hodgkin Lymphoma—First-Line Treatment General treatment note: Routine use of growth factors is not recommended. Leukopenia is not a factor for treatment delay or dose reduction (except for escalated BEACOPP).1 CR=complete response IPS=International Prognostic Score PD=progressive disease PFTs=pulmonary function tests PR=partial response RT=radiation therapy SD=stable disease Stage IA, IIA Favorable ABVD (doxorubicin [Adriamycin] Days 1 and 15: Doxorubicin 25mg/m2 IV + bleomycin 10mg/m2 IV + vinblastine + bleomycin + vinblastine + 6mg/m2 IV + dacarbazine 375mg/m2 IV. dacarbazine [DTIC-Dome]) + Repeat cycle every 4 weeks for 2–4 cycles. involved-field radiotherapy (IFRT)1–4 Follow with IFRT after completion of chemotherapy. Abbreviated Stanford V Weeks 1, 3, 5 and 7: Vinblastine 6mg/m2 IV + doxorubicin 25mg/m2 IV. (doxorubicin + vinblastine + Weeks 1 and 5: Mechlorethamine 6mg/m2. -

(Rituxan®), Rituximab-Abbs (Truxima®), Rituximab-Pvvr (Ruxience®) Prior Authorization Drug Coverage Policy
1 Rituximab Products: Rituximab (Rituxan®), Rituximab-abbs (Truxima®), Rituximab-pvvr (Ruxience®) Prior Authorization Drug Coverage Policy Effective Date: 2/1/2021 Revision Date: n/a Review Date: 7/2/20 Lines of Business: Commercial Policy type: Prior Authorization This Drug Coverage Policy provides parameters for the coverage of rituximab (Rituxan®), rituximab-abbs (Truxima®), and rituximab-pvvr (Ruxience®). Consideration of medically necessary indications are based upon U.S. Food and Drug Administration (FDA) indications, recommended uses within the Centers of Medicare & Medicaid Services (CMS) five recognized compendia, including the National Comprehensive Cancer Network (NCCN) Drugs & Biologics Compendium (Category 1 or 2A recommendations), and peer-reviewed scientific literature eligible for coverage according to the CMS, Medicare Benefit Policy Manual, Chapter 15, section 50.4.5 titled, “Off- Label Use of Anti-Cancer Drugs and Biologics.” This policy evaluates whether the drug therapy is proven to be effective based on published evidence-based medicine. Drug Description1-3 Rituximab (Rituxan®), rituximab-abbs (Truxima®), and rituximab-pvvr (Ruxience®) are monoclonal antibodies that target the CD20 antigen expressed on the surface of pre-B and mature B- lymphocytes. Upon binding to cluster of differentiation (CD) 20, rituximab mediates B-cell lysis. Possible mechanisms of cell lysis include complement dependent cytotoxicity (CDC) and antibody dependent cell mediated cytotoxicity (ADCC). B cells are believed to play a role in the pathogenesis of rheumatoid arthritis (RA) and associated chronic synovitis. In this setting, B cells may be acting at multiple sites in the autoimmune/inflammatory process, including through production of rheumatoid factor (RF) and other autoantibodies, antigen presentation, T-cell activation, and/or proinflammatory cytokine production. -
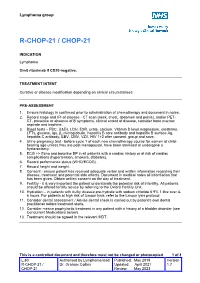
R-Chop-21 / Chop-21
Lymphoma group R-CHOP-21 / CHOP-21 INDICATION Lymphoma Omit rituximab if CD20-negative. TREATMENT INTENT Curative or disease modification depending on clinical circumstances PRE-ASSESSMENT 1. Ensure histology is confirmed prior to administration of chemotherapy and document in notes. 2. Record stage and IPI of disease - CT scan (neck, chest, abdomen and pelvis), and/or PET- CT, presence or absence of B symptoms, clinical extent of disease, consider bone marrow aspirate and trephine. 3. Blood tests – FBC, U&Es, LDH, ESR, urate, calcium, Vitamin D level,magnesium, creatinine, LFTs, glucose, Igs, β2 microglobulin, hepatitis B core antibody and hepatitis B surface Ag, hepatitis C antibody, EBV, CMV, VZV, HIV 1+2 after consent, group and save. 4. Urine pregnancy test • before cycle 1 of each new chemotherapy course for women of child- bearing age unless they are post-menopausal, have been sterilised or undergone a hysterectomy. 5. ECG +/- Echo and baseline BP in all patients with a cardiac history or at risk of cardiac complications (hypertension, smokers, diabetes). 6. Record performance status (WHO/ECOG). 7. Record height and weight. 8. Consent - ensure patient has received adequate verbal and written information regarding their disease, treatment and potential side effects. Document in medical notes all information that has been given. Obtain written consent on the day of treatment. 9. Fertility - it is very important the patient understands the potential risk of infertility. All patients should be offered fertility advice by referring to the Oxford Fertility Unit. 10. Hydration – in patients with bulky disease pre-hydrate with sodium chloride 0.9% 1 litre over 4- 6 hours. -

The Lymphoma Guide Information for Patients and Caregivers
The Lymphoma Guide Information for Patients and Caregivers Ashton, lymphoma survivor This publication was supported by Revised 2016 Publication Update The Lymphoma Guide: Information for Patients and Caregivers The Leukemia & Lymphoma Society wants you to have the most up-to-date information about blood cancer treatment. See below for important new information that was not available at the time this publication was printed. In November 2017, the Food and Drug Administration (FDA) approved obinutuzumab (Gazyva®) in combination with chemotherapy, followed by Gazyva alone in those who responded, for people with previously untreated advanced follicular lymphoma (stage II bulky, III or IV). In November 2017, the Food and Drug Administration (FDA) approved brentuximab vedotin (Adcetris®) for treatment of adult patients with primary cutaneous anaplastic large cell lymphoma (pcALCL) or CD30- expressing mycosis fungoides (MF) who have received prior systemic therapy. In October 2017, the Food and Drug Administration (FDA) approved acalabrutinib (CalquenceTM) for the treatment of adults with mantle cell lymphoma who have received at least one prior therapy. In October 2017, the Food and Drug Administration (FDA) approved axicabtagene ciloleucel (Yescarta™) for the treatment of adult patients with relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy, including diffuse large B-cell lymphoma (DLBCL) not otherwise specified, primary mediastinal large B-cell lymphoma, high-grade B-cell lymphoma, and DLBCL arising from follicular lymphoma. Yescarta is a CD19-directed genetically modified autologous T cell immunotherapy FDA approved. Yescarta is not indicated for the treatment of patients with primary central nervous system lymphoma. In September 2017, the Food and Drug Administration (FDA) approved copanlisib (AliqopaTM) for the treatment of adult patients with relapsed follicular lymphoma (FL) who have received at least two prior systemic therapies. -
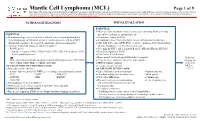
Mantle Cell Lymphoma (MCL)
Mantle Cell Lymphoma (MCL) Page 1 of 9 Disclaimer: This algorithm has been developed for MD Anderson using a multidisciplinary approach considering circumstances particular to MD Anderson’s specific patient population, services and structure, and clinical information. This is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient's care. This algorithm should not be used to treat pregnant women. PATHOLOGIC DIAGNOSIS INITIAL EVALUATION ESSENTIAL: ● Physical exam: attention to node-bearing areas, including Waldeyer's ring, ESSENTIAL: size of liver and spleen, and patient’s age ● Hematopathology review of all slides with at least one tumor paraffin block. ● Performance status (ECOG) Hematopathology confirmation of classic versus aggressive variant of MCL ● B symptoms (fever, drenching night sweats, unintentional weight loss) (blastoid/pleomorphic). Re-biopsy if consult material is non-diagnostic. ● CBC with differential, LDH, BUN, creatinine, albumin, AST, total bilirubin, 1 ● Adequate immunophenotype to confirm diagnosis alkaline phosphatase, serum calcium, uric acid ○ Paraffin panel: ● Screening for HIV 1 and 2, hepatitis B and C (HBcAb, HBaAg, HCVAb) - Pan B-cell marker (CD19, CD20, PAX5), CD3, CD5, CD10, and cyclin D1 ● Beta-2 microglobulin (B2M) - Ki-67 (proliferation rate) ● Chest x-ray, PA and lateral or ● Bone marrow bilateral biopsy with unilateral aspirate Induction ○ Flow cytometry immunophenotyping: -

CD20-Negative Diffuse Large B-Cell Lymphomas: Biology and Emerging Therapeutic Options
Expert Review of Hematology ISSN: 1747-4086 (Print) 1747-4094 (Online) Journal homepage: http://www.tandfonline.com/loi/ierr20 CD20-negative diffuse large B-cell lymphomas: biology and emerging therapeutic options Jorge J Castillo, Julio C Chavez, Francisco J Hernandez-Ilizaliturri & Santiago Montes-Moreno To cite this article: Jorge J Castillo, Julio C Chavez, Francisco J Hernandez-Ilizaliturri & Santiago Montes-Moreno (2015) CD20-negative diffuse large B-cell lymphomas: biology and emerging therapeutic options, Expert Review of Hematology, 8:3, 343-354, DOI: 10.1586/17474086.2015.1007862 To link to this article: http://dx.doi.org/10.1586/17474086.2015.1007862 Published online: 01 Feb 2015. Submit your article to this journal Article views: 165 View related articles View Crossmark data Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=ierr20 Download by: [North Shore Med Ctr], [Jorge Castillo] Date: 16 March 2016, At: 07:44 Review CD20-negative diffuse large B-cell lymphomas: biology and emerging therapeutic options Expert Rev. Hematol. 8(3), 343–354 (2015) Jorge J Castillo*1, CD20-negative diffuse large B-cell lymphoma (DLBCL) is a rare and heterogeneous group of Julio C Chavez2, lymphoproliferative disorders. Known variants of CD20-negative DLBCL include plasmablastic Francisco J lymphoma, primary effusion lymphoma, large B-cell lymphoma arising in human herpesvirus 8-associated multicentric Castleman disease and anaplastic lymphoma kinase-positive DLBCL. Hernandez-Ilizaliturri3 Given the lack of CD20 expression, atypical cellular morphology and aggressive clinical and Santiago 4 behavior characterized by chemotherapy resistance and inferior survival rates, CD20-negative Montes-Moreno DLBCL represents a challenge from the diagnostic and therapeutic perspectives. -
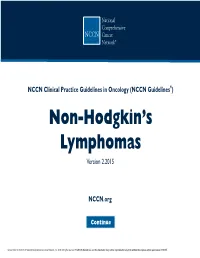
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines® ) Non-Hodgkin’S Lymphomas Version 2.2015
NCCN Guidelines Index NHL Table of Contents Discussion NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines® ) Non-Hodgkin’s Lymphomas Version 2.2015 NCCN.org Continue Version 2.2015, 03/03/15 © National Comprehensive Cancer Network, Inc. 2015, All rights reserved. The NCCN Guidelines® and this illustration may not be reproduced in any form without the express written permission of NCCN® . Peripheral T-Cell Lymphomas NCCN Guidelines Version 2.2015 NCCN Guidelines Index NHL Table of Contents Peripheral T-Cell Lymphomas Discussion DIAGNOSIS SUBTYPES ESSENTIAL: · Review of all slides with at least one paraffin block representative of the tumor should be done by a hematopathologist with expertise in the diagnosis of PTCL. Rebiopsy if consult material is nondiagnostic. · An FNA alone is not sufficient for the initial diagnosis of peripheral T-cell lymphoma. Subtypes included: · Adequate immunophenotyping to establish diagnosisa,b · Peripheral T-cell lymphoma (PTCL), NOS > IHC panel: CD20, CD3, CD10, BCL6, Ki-67, CD5, CD30, CD2, · Angioimmunoblastic T-cell lymphoma (AITL)d See Workup CD4, CD8, CD7, CD56, CD57 CD21, CD23, EBER-ISH, ALK · Anaplastic large cell lymphoma (ALCL), ALK positive (TCEL-2) or · ALCL, ALK negative > Cell surface marker analysis by flow cytometry: · Enteropathy-associated T-cell lymphoma (EATL) kappa/lambda, CD45, CD3, CD5, CD19, CD10, CD20, CD30, CD4, CD8, CD7, CD2; TCRαβ; TCRγ Subtypesnot included: · Primary cutaneous ALCL USEFUL UNDER CERTAIN CIRCUMSTANCES: · All other T-cell lymphomas · Molecular analysis to detect: antigen receptor gene rearrangements; t(2;5) and variants · Additional immunohistochemical studies to establish Extranodal NK/T-cell lymphoma, nasal type (See NKTL-1) lymphoma subtype:βγ F1, TCR-C M1, CD279/PD1, CXCL-13 · Cytogenetics to establish clonality · Assessment of HTLV-1c serology in at-risk populations. -

Analysis Compared with Classical Hodgkin Lymphoma
From bloodjournal.hematologylibrary.org by guest on July 21, 2014. For personal use only. 2014 123: 3567-3573 doi:10.1182/blood-2013-12-541078 originally published online April 8, 2014 Advanced-stage nodular lymphocyte predominant Hodgkin lymphoma compared with classical Hodgkin lymphoma: a matched pair outcome analysis Katharine H. Xing, Joseph M. Connors, Anky Lai, Mubarak Al-Mansour, Laurie H. Sehn, Diego Villa, Richard Klasa, Tamara Shenkier, Randy D. Gascoyne, Brian Skinnider and Kerry J. Savage Updated information and services can be found at: http://bloodjournal.hematologylibrary.org/content/123/23/3567.full.html Articles on similar topics can be found in the following Blood collections Clinical Trials and Observations (3892 articles) Free Research Articles (2531 articles) Lymphoid Neoplasia (1767 articles) Information about reproducing this article in parts or in its entirety may be found online at: http://bloodjournal.hematologylibrary.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://bloodjournal.hematologylibrary.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://bloodjournal.hematologylibrary.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved. From bloodjournal.hematologylibrary.org by guest on July 21, 2014. For personal use only. Regular Article CLINICAL TRIALS AND OBSERVATIONS Advanced-stage nodular lymphocyte predominant Hodgkin lymphoma compared with classical Hodgkin lymphoma: a matched pair outcome analysis Katharine H. -

Non-Hodgkin Lymphoma
Non-Hodgkin Lymphoma Rick, non-Hodgkin lymphoma survivor This publication was supported in part by grants from Revised 2013 A Message From John Walter President and CEO of The Leukemia & Lymphoma Society The Leukemia & Lymphoma Society (LLS) believes we are living at an extraordinary moment. LLS is committed to bringing you the most up-to-date blood cancer information. We know how important it is for you to have an accurate understanding of your diagnosis, treatment and support options. An important part of our mission is bringing you the latest information about advances in treatment for non-Hodgkin lymphoma, so you can work with your healthcare team to determine the best options for the best outcomes. Our vision is that one day the great majority of people who have been diagnosed with non-Hodgkin lymphoma will be cured or will be able to manage their disease with a good quality of life. We hope that the information in this publication will help you along your journey. LLS is the world’s largest voluntary health organization dedicated to funding blood cancer research, education and patient services. Since 1954, LLS has been a driving force behind almost every treatment breakthrough for patients with blood cancers, and we have awarded almost $1 billion to fund blood cancer research. Our commitment to pioneering science has contributed to an unprecedented rise in survival rates for people with many different blood cancers. Until there is a cure, LLS will continue to invest in research, patient support programs and services that improve the quality of life for patients and families. -

Bendamustine Plus Rituximab: Is It a BRIGHT Idea?
Editorial Commentary Page 1 of 4 Bendamustine plus rituximab: is it a BRIGHT idea? Carlo Visco1, Francesca Maria Quaglia1, Chiara Bovo2, Maria Chiara Tisi3, Mauro Krampera1 1Department of Medicine, Section of Hematology, University of Verona, Verona, Italy; 2Medical Direction, University Hospital of Verona, Verona, Italy; 3Cell Therapy and Hematology, San Bortolo Hospital, Vicenza, Italy Correspondence to: Carlo Visco, MD. Associate Professor of Hematology, Department of Medicine, Section of Hematology, University of Verona, P.le L.A. Scuro 10, 37134 Verona, Italy. Email: [email protected]. Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Xinyi Du (Department of Hematology, Northern Jiangsu People’s Hospital, Yangzhou, China). Comment on: Flinn IW, van der Jagt R, Kahl B, et al. First-Line Treatment of Patients With Indolent Non-Hodgkin Lymphoma or Mantle-Cell Lymphoma With Bendamustine Plus Rituximab Versus R-CHOP or R-CVP: Results of the BRIGHT 5-Year Follow-Up Study. J Clin Oncol 2019;37:984-91. Submitted Sep 20, 2019. Accepted for publication Oct 14, 2019. doi: 10.21037/cco.2019.10.03 View this article at: http://dx.doi.org/10.21037/cco.2019.10.03 Flinn et al. have reported the results of the long-term in the BRIGHT study were eagerly awaited. As the Stil- follow-up for the BRIGHT trial, an international study 1 trial, the BRIGHT study (3) included patients with which compared the efficacy and the safety of bendamustine follicular lymphoma (grade 1 or 2, excluding grade 3A), plus rituximab (BR) with either rituximab plus lymphoplasmacytic lymphoma, splenic marginal zone B-cell cyclophosphamide, doxorubicin, vincristine, and prednisone lymphoma, extranodal marginal zone lymphoma (MZL) (R-CHOP) or rituximab plus cyclophosphamide, vincristine, of mucosa-associated lymphoid tissue type, nodal marginal and prednisone (R-CVP) for treatment-naive patients with zone B-cell lymphoma (371 patients with iNHL), or MCL indolent non-Hodgkin lymphoma (iNHL) or mantle-cell (74 patients).