HODGKIN LYMPHOMA TREATMENT REGIMENS (Part 1 of 2)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hodgkin Lymphoma Treatment Regimens
HODGKIN LYMPHOMA TREATMENT REGIMENS (Part 1 of 5) Clinical Trials: The National Comprehensive Cancer Network recommends cancer patient participation in clinical trials as the gold standard for treatment. Cancer therapy selection, dosing, administration, and the management of related adverse events can be a complex process that should be handled by an experienced health care team. Clinicians must choose and verify treatment options based on the individual patient; drug dose modifications and supportive care interventions should be administered accordingly. The cancer treatment regimens below may include both U.S. Food and Drug Administration-approved and unapproved indications/regimens. These regimens are provided only to supplement the latest treatment strategies. These Guidelines are a work in progress that may be refined as often as new significant data become available. The NCCN Guidelines® are a consensus statement of its authors regarding their views of currently accepted approaches to treatment. Any clinician seeking to apply or consult any NCCN Guidelines® is expected to use independent medical judgment in the context of individual clinical circumstances to determine any patient’s care or treatment. The NCCN makes no warranties of any kind whatsoever regarding their content, use, or application and disclaims any responsibility for their application or use in any way. Classical Hodgkin Lymphoma1 Note: All recommendations are Category 2A unless otherwise indicated. Primary Treatment Stage IA, IIA Favorable (No Bulky Disease, <3 Sites of Disease, ESR <50, and No E-lesions) REGIMEN DOSING Doxorubicin + Bleomycin + Days 1 and 15: Doxorubicin 25mg/m2 IV push + bleomycin 10units/m2 IV push + Vinblastine + Dacarbazine vinblastine 6mg/m2 IV over 5–10 minutes + dacarbazine 375mg/m2 IV over (ABVD) (Category 1)2-5 60 minutes. -

Vincristine (Conventional): Drug Information
Official reprint from UpToDate® www.uptodate.com ©2017 UpToDate® Vincristine (conventional): Drug information Copyright 1978-2017 Lexicomp, Inc. All rights reserved. (For additional information see "Vincristine (conventional): Patient drug information" and see "Vincristine (conventional): Pediatric drug information") For abbreviations and symbols that may be used in Lexicomp (show table) Special Alerts Vincristine Sulfate Safety Alert October 2015 Health Canada is notifying health care providers that certain lots of Hospira’s vincristine sulfate 1 mg/mL injection (DIN 02183013: 2 mL vial, list #7077A001; 5 mL vial, list #7082A001) have incorrect or outdated safety information on the inner/outer labels and package insert, which may increase the risk to patients and may result in significant patient harm requiring medical intervention. These warnings include: - Vincristine should only be administered by the intravenous (IV) route. Administration of vincristine by any other route can be fatal. - Syringes containing this product should be labeled “Warning - for IV use only.” - Extemporaneously prepared syringes containing this product must be packaged in an overwrap which is labeled “Do not remove covering until moment of injection. For IV use only - fatal if given by other routes.” - Contraindication of vincristine in patients with demyelinating Charcot-Marie-Tooth syndrome. - Potential risk of acute shortness of breath when vincristine is coadministered with mitomycin-C and GI toxicities including necrosis with administration of vincristine. Health care providers are requested to consult with the approved Canadian product monograph for vincristine sulfate 1 mg/mL for the most updated information. Consumers with questions should contact their health care provider for more information. ALERT: US Boxed Warning Experienced physician: Vincristine should be administered by individuals experienced in the administration of the drug. -

Hodgkin Lymphoma
Hodgkin Lymphoma Erica, Hodgkin lymphoma survivor Revised 2016 Publication Update Hodgkin Lymphoma The Leukemia & Lymphoma Society wants you to have the most up-to-date information about blood cancer treatment. See below for important new information that was not available at the time this publication was printed. In May 2017, the Food and Drug Administration (FDA) approved nivolumab (Opdivo®) for the treatment of adult patients with classical Hodgkin lymphoma (HL) that has relapsed or progressed after 3 or more lines of systemic therapy that includes autologous hematopoietic stem cell transplantation (HSCT). It is also approved for the treatment of adult patients with classical HL that has relapsed or progressed after autologous HSCT and brentuximab vedotin. These indications are approved under accelerated approval based on overall response rate. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials. In March 2017, the Food and Drug Administration (FDA) approved pembrolizumab (Keytruda®) for the treatment of adult and pediatric patients with refractory classical Hodgkin lymphoma (cHL), or who have relapsed after 3 or more prior lines of therapy. This indication is approved under accelerated approval based on tumor response rate and durability of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials. For more information, contact an Information Specialist at (800) 955-4572 or [email protected]. Information Specialists: 800.955.4572 I www.LLS.org PS57 A Message from Louis J. DeGennaro, PhD President and CEO of The Leukemia & Lymphoma Society The Leukemia & Lymphoma Society (LLS) is the world’s largest voluntary health organization dedicated to finding cures for blood cancer patients. -

(Rituxan®), Rituximab-Abbs (Truxima®), Rituximab-Pvvr (Ruxience®) Prior Authorization Drug Coverage Policy
1 Rituximab Products: Rituximab (Rituxan®), Rituximab-abbs (Truxima®), Rituximab-pvvr (Ruxience®) Prior Authorization Drug Coverage Policy Effective Date: 2/1/2021 Revision Date: n/a Review Date: 7/2/20 Lines of Business: Commercial Policy type: Prior Authorization This Drug Coverage Policy provides parameters for the coverage of rituximab (Rituxan®), rituximab-abbs (Truxima®), and rituximab-pvvr (Ruxience®). Consideration of medically necessary indications are based upon U.S. Food and Drug Administration (FDA) indications, recommended uses within the Centers of Medicare & Medicaid Services (CMS) five recognized compendia, including the National Comprehensive Cancer Network (NCCN) Drugs & Biologics Compendium (Category 1 or 2A recommendations), and peer-reviewed scientific literature eligible for coverage according to the CMS, Medicare Benefit Policy Manual, Chapter 15, section 50.4.5 titled, “Off- Label Use of Anti-Cancer Drugs and Biologics.” This policy evaluates whether the drug therapy is proven to be effective based on published evidence-based medicine. Drug Description1-3 Rituximab (Rituxan®), rituximab-abbs (Truxima®), and rituximab-pvvr (Ruxience®) are monoclonal antibodies that target the CD20 antigen expressed on the surface of pre-B and mature B- lymphocytes. Upon binding to cluster of differentiation (CD) 20, rituximab mediates B-cell lysis. Possible mechanisms of cell lysis include complement dependent cytotoxicity (CDC) and antibody dependent cell mediated cytotoxicity (ADCC). B cells are believed to play a role in the pathogenesis of rheumatoid arthritis (RA) and associated chronic synovitis. In this setting, B cells may be acting at multiple sites in the autoimmune/inflammatory process, including through production of rheumatoid factor (RF) and other autoantibodies, antigen presentation, T-cell activation, and/or proinflammatory cytokine production. -
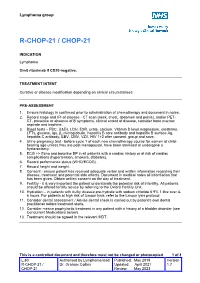
R-Chop-21 / Chop-21
Lymphoma group R-CHOP-21 / CHOP-21 INDICATION Lymphoma Omit rituximab if CD20-negative. TREATMENT INTENT Curative or disease modification depending on clinical circumstances PRE-ASSESSMENT 1. Ensure histology is confirmed prior to administration of chemotherapy and document in notes. 2. Record stage and IPI of disease - CT scan (neck, chest, abdomen and pelvis), and/or PET- CT, presence or absence of B symptoms, clinical extent of disease, consider bone marrow aspirate and trephine. 3. Blood tests – FBC, U&Es, LDH, ESR, urate, calcium, Vitamin D level,magnesium, creatinine, LFTs, glucose, Igs, β2 microglobulin, hepatitis B core antibody and hepatitis B surface Ag, hepatitis C antibody, EBV, CMV, VZV, HIV 1+2 after consent, group and save. 4. Urine pregnancy test • before cycle 1 of each new chemotherapy course for women of child- bearing age unless they are post-menopausal, have been sterilised or undergone a hysterectomy. 5. ECG +/- Echo and baseline BP in all patients with a cardiac history or at risk of cardiac complications (hypertension, smokers, diabetes). 6. Record performance status (WHO/ECOG). 7. Record height and weight. 8. Consent - ensure patient has received adequate verbal and written information regarding their disease, treatment and potential side effects. Document in medical notes all information that has been given. Obtain written consent on the day of treatment. 9. Fertility - it is very important the patient understands the potential risk of infertility. All patients should be offered fertility advice by referring to the Oxford Fertility Unit. 10. Hydration – in patients with bulky disease pre-hydrate with sodium chloride 0.9% 1 litre over 4- 6 hours. -

Anaplastic Large Cell Lymphoma (ALCL)
Helpline (freephone) 0808 808 5555 [email protected] www.lymphoma-action.org.uk Anaplastic large cell lymphoma (ALCL) This page is about anaplastic large-cell lymphoma (ALCL), a type of T-cell lymphoma. On this page What is ALCL? Who gets it? Symptoms Treatment Relapsed and refractory ALCL Research and targeted treatments We have separate information about the topics in bold font. Please get in touch if you’d like to request copies or if you would like further information about any aspect of lymphoma. Phone 0808 808 5555 or email [email protected]. What is ALCL? Anaplastic large cell lymphoma (ALCL) is a type of T-cell lymphoma – a non-Hodgkin lymphoma that develops from white blood cells called T cells. Under a microscope, the cancerous cells in ALCL look large, undeveloped and very abnormal (‘anaplastic’). There are four main types of ALCL. They have complicated names based on their features and the types of proteins they make: • ALK-positive ALCL (also known as ALK+ ALCL) is the most common type. In ALK-positive ALCL, the abnormal T cells have a genetic change (mutation) that means they make a protein called ‘anaplastic lymphoma kinase’ (ALK). In other words, they test positive for ALK. ALK-positive ALCL is a fast-growing (high-grade) lymphoma. Page 1 of 6 © Lymphoma Action • ALK-negative ALCL (also known as ALK- ALCL) is a high-grade lymphoma that accounts for around 3 in every 10 cases of ALCL. The abnormal T cells do not make the ALK protein – they test negative for ALK. -
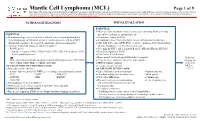
Mantle Cell Lymphoma (MCL)
Mantle Cell Lymphoma (MCL) Page 1 of 9 Disclaimer: This algorithm has been developed for MD Anderson using a multidisciplinary approach considering circumstances particular to MD Anderson’s specific patient population, services and structure, and clinical information. This is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient's care. This algorithm should not be used to treat pregnant women. PATHOLOGIC DIAGNOSIS INITIAL EVALUATION ESSENTIAL: ● Physical exam: attention to node-bearing areas, including Waldeyer's ring, ESSENTIAL: size of liver and spleen, and patient’s age ● Hematopathology review of all slides with at least one tumor paraffin block. ● Performance status (ECOG) Hematopathology confirmation of classic versus aggressive variant of MCL ● B symptoms (fever, drenching night sweats, unintentional weight loss) (blastoid/pleomorphic). Re-biopsy if consult material is non-diagnostic. ● CBC with differential, LDH, BUN, creatinine, albumin, AST, total bilirubin, 1 ● Adequate immunophenotype to confirm diagnosis alkaline phosphatase, serum calcium, uric acid ○ Paraffin panel: ● Screening for HIV 1 and 2, hepatitis B and C (HBcAb, HBaAg, HCVAb) - Pan B-cell marker (CD19, CD20, PAX5), CD3, CD5, CD10, and cyclin D1 ● Beta-2 microglobulin (B2M) - Ki-67 (proliferation rate) ● Chest x-ray, PA and lateral or ● Bone marrow bilateral biopsy with unilateral aspirate Induction ○ Flow cytometry immunophenotyping: -
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines® ) Non-Hodgkin’S Lymphomas Version 2.2015
NCCN Guidelines Index NHL Table of Contents Discussion NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines® ) Non-Hodgkin’s Lymphomas Version 2.2015 NCCN.org Continue Version 2.2015, 03/03/15 © National Comprehensive Cancer Network, Inc. 2015, All rights reserved. The NCCN Guidelines® and this illustration may not be reproduced in any form without the express written permission of NCCN® . Peripheral T-Cell Lymphomas NCCN Guidelines Version 2.2015 NCCN Guidelines Index NHL Table of Contents Peripheral T-Cell Lymphomas Discussion DIAGNOSIS SUBTYPES ESSENTIAL: · Review of all slides with at least one paraffin block representative of the tumor should be done by a hematopathologist with expertise in the diagnosis of PTCL. Rebiopsy if consult material is nondiagnostic. · An FNA alone is not sufficient for the initial diagnosis of peripheral T-cell lymphoma. Subtypes included: · Adequate immunophenotyping to establish diagnosisa,b · Peripheral T-cell lymphoma (PTCL), NOS > IHC panel: CD20, CD3, CD10, BCL6, Ki-67, CD5, CD30, CD2, · Angioimmunoblastic T-cell lymphoma (AITL)d See Workup CD4, CD8, CD7, CD56, CD57 CD21, CD23, EBER-ISH, ALK · Anaplastic large cell lymphoma (ALCL), ALK positive (TCEL-2) or · ALCL, ALK negative > Cell surface marker analysis by flow cytometry: · Enteropathy-associated T-cell lymphoma (EATL) kappa/lambda, CD45, CD3, CD5, CD19, CD10, CD20, CD30, CD4, CD8, CD7, CD2; TCRαβ; TCRγ Subtypesnot included: · Primary cutaneous ALCL USEFUL UNDER CERTAIN CIRCUMSTANCES: · All other T-cell lymphomas · Molecular analysis to detect: antigen receptor gene rearrangements; t(2;5) and variants · Additional immunohistochemical studies to establish Extranodal NK/T-cell lymphoma, nasal type (See NKTL-1) lymphoma subtype:βγ F1, TCR-C M1, CD279/PD1, CXCL-13 · Cytogenetics to establish clonality · Assessment of HTLV-1c serology in at-risk populations. -

Highlights from the Pan Pacific Lymphoma Conference
October 2011 A SPECIAL MEETING REVIEW EDITION Volume 9, Issue 10, Supplement 24 Highlights From the Pan Pacific Lymphoma Conference August 15–19, 2011 Kauai, Hawaii Special Reporting on: • Aggressive T-Cell Lymphomas • Novel Agents With Activity in CLL/SLL • PTCL—Update on Novel Therapies • Agents Targeting the Stromal Elements of the Lymph Node • Inducing Apoptosis in Lymphoma Cells Through Novel Agents With Expert Commentary by: Bruce D. Cheson, MD Deputy Chief Division of Hematology-Oncology Head of Hematology Lombardi Comprehensive Cancer Center Georgetown University Hospital Washington, DC Eb: E W Th O N www.clinicaladvances.com ENGINEERING T H E N E X T GENERATION OF ANTIBODY-DRUG CONJUGATES 003203_sgncor_adcadvcaho_fa4.indd 2 8/25/11 11:13 AM An innovative approach to improving outcomes in patients with cancer Antibody-drug conjugates (ADCs) use a conditionally stable linker to combine the targeting specificity of monoclonal antibodies with the tumor-killing power of potent cytotoxic agents.1,2 This could allow potent drugs to be delivered directly to tumor cells with minimal systemic toxicity. Optimizing the parameters for clinical success Scientists at Seattle Genetics are focused on parameters critical to the effective performance of ADCs, including target antigen selection,3,4 linker stability5-7 and potent cytotoxic agents.4,7,8 Elements of an antibody-drug conjugate Linker ADCs link precision and Antibody attaches the cytotoxic agent to specific for a tumor-associated the antibody. Newer linker potency for greater activity -

Analysis Compared with Classical Hodgkin Lymphoma
From bloodjournal.hematologylibrary.org by guest on July 21, 2014. For personal use only. 2014 123: 3567-3573 doi:10.1182/blood-2013-12-541078 originally published online April 8, 2014 Advanced-stage nodular lymphocyte predominant Hodgkin lymphoma compared with classical Hodgkin lymphoma: a matched pair outcome analysis Katharine H. Xing, Joseph M. Connors, Anky Lai, Mubarak Al-Mansour, Laurie H. Sehn, Diego Villa, Richard Klasa, Tamara Shenkier, Randy D. Gascoyne, Brian Skinnider and Kerry J. Savage Updated information and services can be found at: http://bloodjournal.hematologylibrary.org/content/123/23/3567.full.html Articles on similar topics can be found in the following Blood collections Clinical Trials and Observations (3892 articles) Free Research Articles (2531 articles) Lymphoid Neoplasia (1767 articles) Information about reproducing this article in parts or in its entirety may be found online at: http://bloodjournal.hematologylibrary.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://bloodjournal.hematologylibrary.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://bloodjournal.hematologylibrary.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved. From bloodjournal.hematologylibrary.org by guest on July 21, 2014. For personal use only. Regular Article CLINICAL TRIALS AND OBSERVATIONS Advanced-stage nodular lymphocyte predominant Hodgkin lymphoma compared with classical Hodgkin lymphoma: a matched pair outcome analysis Katharine H. -

Bendamustine Plus Rituximab: Is It a BRIGHT Idea?
Editorial Commentary Page 1 of 4 Bendamustine plus rituximab: is it a BRIGHT idea? Carlo Visco1, Francesca Maria Quaglia1, Chiara Bovo2, Maria Chiara Tisi3, Mauro Krampera1 1Department of Medicine, Section of Hematology, University of Verona, Verona, Italy; 2Medical Direction, University Hospital of Verona, Verona, Italy; 3Cell Therapy and Hematology, San Bortolo Hospital, Vicenza, Italy Correspondence to: Carlo Visco, MD. Associate Professor of Hematology, Department of Medicine, Section of Hematology, University of Verona, P.le L.A. Scuro 10, 37134 Verona, Italy. Email: [email protected]. Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Xinyi Du (Department of Hematology, Northern Jiangsu People’s Hospital, Yangzhou, China). Comment on: Flinn IW, van der Jagt R, Kahl B, et al. First-Line Treatment of Patients With Indolent Non-Hodgkin Lymphoma or Mantle-Cell Lymphoma With Bendamustine Plus Rituximab Versus R-CHOP or R-CVP: Results of the BRIGHT 5-Year Follow-Up Study. J Clin Oncol 2019;37:984-91. Submitted Sep 20, 2019. Accepted for publication Oct 14, 2019. doi: 10.21037/cco.2019.10.03 View this article at: http://dx.doi.org/10.21037/cco.2019.10.03 Flinn et al. have reported the results of the long-term in the BRIGHT study were eagerly awaited. As the Stil- follow-up for the BRIGHT trial, an international study 1 trial, the BRIGHT study (3) included patients with which compared the efficacy and the safety of bendamustine follicular lymphoma (grade 1 or 2, excluding grade 3A), plus rituximab (BR) with either rituximab plus lymphoplasmacytic lymphoma, splenic marginal zone B-cell cyclophosphamide, doxorubicin, vincristine, and prednisone lymphoma, extranodal marginal zone lymphoma (MZL) (R-CHOP) or rituximab plus cyclophosphamide, vincristine, of mucosa-associated lymphoid tissue type, nodal marginal and prednisone (R-CVP) for treatment-naive patients with zone B-cell lymphoma (371 patients with iNHL), or MCL indolent non-Hodgkin lymphoma (iNHL) or mantle-cell (74 patients). -

Older Patients
Older patients (aged ≥60 years) with previously untreated advanced-stage classical Hodgkin lymphoma: a detailed analysis from the phase III ECHELON-1 study by Andrew M. Evens, Joseph M. Connors, Anas Younes, Stephen M. Ansell, Won Seog Kim, John Radford, Tatyana Feldman, Joseph Tuscano, Kerry J. Savage, Yasuhiro Oki, Andrew Grigg, Christopher Pocock, Monika Dlugosz-Danecka, Keenan Fenton, Andres Forero-Torres, Rachael Liu, Hina Jolin, Ashish Gautam, and Andrea Gallamini Haematologica 2021 [Epub ahead of print] Citation: Andrew M. Evens, Joseph M. Connors, Anas Younes, Stephen M. Ansell, Won Seog Kim, John Radford, Tatyana Feldman, Joseph Tuscano, Kerry J. Savage, Yasuhiro Oki, Andrew Grigg, Christopher Pocock, Monika Dlugosz-Danecka, Keenan Fenton, Andres Forero-Torres, Rachael Liu, Hina Jolin, Ashish Gautam, and Andrea Gallamini. Older patients (aged ≥60 years) with previously untreated advanced-stage classical Hodgkin lymphoma: a detailed analysis from the phase III ECHELON-1 study. Haematologica. 2021; 106:xxx doi:10.3324/haematol.2021.278438 Publisher's Disclaimer. E-publishing ahead of print is increasingly important for the rapid dissemination of science. Haematologica is, therefore, E-publishing PDF files of an early version of manuscripts that have completed a regular peer review and have been accepted for publication. E-publishing of this PDF file has been approved by the authors. After having E-published Ahead of Print, manuscripts will then undergo technical and English editing, typesetting, proof correction and be presented for the authors' final approval; the final version of the manuscript will then appear in print on a regular issue of the journal. All legal disclaimers that apply to the journal also pertain to this production process.