Frequent Mutation of Hypoxia-Related Genes in Persistent Pulmonary
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Advancing a Clinically Relevant Perspective of the Clonal Nature of Cancer
Advancing a clinically relevant perspective of the clonal nature of cancer Christian Ruiza,b, Elizabeth Lenkiewicza, Lisa Eversa, Tara Holleya, Alex Robesona, Jeffrey Kieferc, Michael J. Demeurea,d, Michael A. Hollingsworthe, Michael Shenf, Donna Prunkardf, Peter S. Rabinovitchf, Tobias Zellwegerg, Spyro Moussesc, Jeffrey M. Trenta,h, John D. Carpteni, Lukas Bubendorfb, Daniel Von Hoffa,d, and Michael T. Barretta,1 aClinical Translational Research Division, Translational Genomics Research Institute, Scottsdale, AZ 85259; bInstitute for Pathology, University Hospital Basel, University of Basel, 4031 Basel, Switzerland; cGenetic Basis of Human Disease, Translational Genomics Research Institute, Phoenix, AZ 85004; dVirginia G. Piper Cancer Center, Scottsdale Healthcare, Scottsdale, AZ 85258; eEppley Institute for Research in Cancer and Allied Diseases, Nebraska Medical Center, Omaha, NE 68198; fDepartment of Pathology, University of Washington, Seattle, WA 98105; gDivision of Urology, St. Claraspital and University of Basel, 4058 Basel, Switzerland; hVan Andel Research Institute, Grand Rapids, MI 49503; and iIntegrated Cancer Genomics Division, Translational Genomics Research Institute, Phoenix, AZ 85004 Edited* by George F. Vande Woude, Van Andel Research Institute, Grand Rapids, MI, and approved June 10, 2011 (received for review March 11, 2011) Cancers frequently arise as a result of an acquired genomic insta- on the basis of morphology alone (8). Thus, the application of bility and the subsequent clonal evolution of neoplastic cells with purification methods such as laser capture microdissection does variable patterns of genetic aberrations. Thus, the presence and not resolve the complexities of many samples. A second approach behaviors of distinct clonal populations in each patient’s tumor is to passage tumor biopsies in tissue culture or in xenografts (4, 9– may underlie multiple clinical phenotypes in cancers. -

(P -Value<0.05, Fold Change≥1.4), 4 Vs. 0 Gy Irradiation
Table S1: Significant differentially expressed genes (P -Value<0.05, Fold Change≥1.4), 4 vs. 0 Gy irradiation Genbank Fold Change P -Value Gene Symbol Description Accession Q9F8M7_CARHY (Q9F8M7) DTDP-glucose 4,6-dehydratase (Fragment), partial (9%) 6.70 0.017399678 THC2699065 [THC2719287] 5.53 0.003379195 BC013657 BC013657 Homo sapiens cDNA clone IMAGE:4152983, partial cds. [BC013657] 5.10 0.024641735 THC2750781 Ciliary dynein heavy chain 5 (Axonemal beta dynein heavy chain 5) (HL1). 4.07 0.04353262 DNAH5 [Source:Uniprot/SWISSPROT;Acc:Q8TE73] [ENST00000382416] 3.81 0.002855909 NM_145263 SPATA18 Homo sapiens spermatogenesis associated 18 homolog (rat) (SPATA18), mRNA [NM_145263] AA418814 zw01a02.s1 Soares_NhHMPu_S1 Homo sapiens cDNA clone IMAGE:767978 3', 3.69 0.03203913 AA418814 AA418814 mRNA sequence [AA418814] AL356953 leucine-rich repeat-containing G protein-coupled receptor 6 {Homo sapiens} (exp=0; 3.63 0.0277936 THC2705989 wgp=1; cg=0), partial (4%) [THC2752981] AA484677 ne64a07.s1 NCI_CGAP_Alv1 Homo sapiens cDNA clone IMAGE:909012, mRNA 3.63 0.027098073 AA484677 AA484677 sequence [AA484677] oe06h09.s1 NCI_CGAP_Ov2 Homo sapiens cDNA clone IMAGE:1385153, mRNA sequence 3.48 0.04468495 AA837799 AA837799 [AA837799] Homo sapiens hypothetical protein LOC340109, mRNA (cDNA clone IMAGE:5578073), partial 3.27 0.031178378 BC039509 LOC643401 cds. [BC039509] Homo sapiens Fas (TNF receptor superfamily, member 6) (FAS), transcript variant 1, mRNA 3.24 0.022156298 NM_000043 FAS [NM_000043] 3.20 0.021043295 A_32_P125056 BF803942 CM2-CI0135-021100-477-g08 CI0135 Homo sapiens cDNA, mRNA sequence 3.04 0.043389246 BF803942 BF803942 [BF803942] 3.03 0.002430239 NM_015920 RPS27L Homo sapiens ribosomal protein S27-like (RPS27L), mRNA [NM_015920] Homo sapiens tumor necrosis factor receptor superfamily, member 10c, decoy without an 2.98 0.021202829 NM_003841 TNFRSF10C intracellular domain (TNFRSF10C), mRNA [NM_003841] 2.97 0.03243901 AB002384 C6orf32 Homo sapiens mRNA for KIAA0386 gene, partial cds. -

Title Human Genetic Diversity Possibly Determines Human's Compliance to COVID-19
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 16 April 2020 Title Human genetic diversity possibly determines human's compliance to COVID-19 1* 2 1 1 1 1 2 2 Yiqiang Zhao , Yongji Liu , Sa Li , Yuzhan Wang , Lina Bu , Qi Liu , Hongyi Lv , Fang Wan , Lida Wu2, Zeming Ning3, Yuchun Gu2,4* 1. Beijing Advanced Innovation Center for Food Nutrition and Human Health, China Agricultural University, Beijing, China 2. Allife Medicine Ltd., Beijing, China 3. The Wellcome Sanger Institute, Wellcome Genome Campus, Cambridge, UK 4. Regenerative Medicine Center, Aston University, Birmingham, UK Corresponding Author Prof. Yiqiang Zhao Beijing Advanced Innovation Center for Food Nutrition and Human Health China Agricultural University Beijing, China Email: [email protected] And Prof. Yuchun Gu The regenerative Medicine Center Aston University Birmingham, UK & Allife Medicine Co.Ltd Beijing, China Email: [email protected] © 2020 by the author(s). Distributed under a Creative Commons CC BY license. Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 16 April 2020 Abstract The rapid spread of the coronavirus disease 2019 (COVID-19) is a serious threat to public health systems globally and is subsequently, a cause of anxiety and panic within human society. Understanding the mechanisms and reducing the chances of having severe symptoms from COVID-19 will play an essential role in treating the disease, and become an urgent task to calm the panic. However, the COVID-19 test developed to identify virus carriers is unable to predict symptom development in individuals upon infection. Experiences from other plagues in human history and COVID-19 statistics suggest that genetic factors may determine the compliance with the virus, i.e., severe, mild, and asymptomatic. -

Egfr Activates a Taz-Driven Oncogenic Program in Glioblastoma
EGFR ACTIVATES A TAZ-DRIVEN ONCOGENIC PROGRAM IN GLIOBLASTOMA by Minling Gao A thesis submitted to Johns Hopkins University in conformity with the requirements for the degree of Doctor of Philosophy Baltimore, Maryland March 2020 ©2020 Minling Gao All rights reserved Abstract Hyperactivated EGFR signaling is associated with about 45% of Glioblastoma (GBM), the most aggressive and lethal primary brain tumor in humans. However, the oncogenic transcriptional events driven by EGFR are still incompletely understood. We studied the role of the transcription factor TAZ to better understand master transcriptional regulators in mediating the EGFR signaling pathway in GBM. The transcriptional coactivator with PDZ- binding motif (TAZ) and its paralog gene, the Yes-associated protein (YAP) are two transcriptional co-activators that play important roles in multiple cancer types and are regulated in a context-dependent manner by various upstream signaling pathways, e.g. the Hippo, WNT and GPCR signaling. In GBM cells, TAZ functions as an oncogene that drives mesenchymal transition and radioresistance. This thesis intends to broaden our understanding of EGFR signaling and TAZ regulation in GBM. In patient-derived GBM cell models, EGF induced TAZ and its known gene targets through EGFR and downstream tyrosine kinases (ERK1/2 and STAT3). In GBM cells with EGFRvIII, an EGF-independent and constitutively active mutation, TAZ showed EGF- independent hyperactivation when compared to EGFRvIII-negative cells. These results revealed a novel EGFR-TAZ signaling axis in GBM cells. The second contribution of this thesis is that we performed next-generation sequencing to establish the first genome-wide map of EGF-induced TAZ target genes. -

RFX Transcription Factors Are Essential for Hearing in Mice
ARTICLE Received 2 Mar 2015 | Accepted 4 Sep 2015 | Published 15 Oct 2015 DOI: 10.1038/ncomms9549 OPEN RFX transcription factors are essential for hearing in mice Ran Elkon1,*, Beatrice Milon2,*, Laura Morrison2, Manan Shah2, Sarath Vijayakumar3, Manoj Racherla2, Carmen C. Leitch4, Lorna Silipino2, Shadan Hadi5, Miche`le Weiss-Gayet6, Emmanue`le Barras7, Christoph D. Schmid8, Aouatef Ait-Lounis7,w, Ashley Barnes2, Yang Song9, David J. Eisenman2, Efrat Eliyahu10, Gregory I. Frolenkov5, Scott E. Strome2,Be´ne´dicte Durand6, Norann A. Zaghloul4, Sherri M. Jones3, Walter Reith7 & Ronna Hertzano2,9,11 Sensorineural hearing loss is a common and currently irreversible disorder, because mammalian hair cells (HCs) do not regenerate and current stem cell and gene delivery protocols result only in immature HC-like cells. Importantly, although the transcriptional regulators of embryonic HC development have been described, little is known about the postnatal regulators of maturating HCs. Here we apply a cell type-specific functional genomic analysis to the transcriptomes of auditory and vestibular sensory epithelia from early post- natal mice. We identify RFX transcription factors as essential and evolutionarily conserved regulators of the HC-specific transcriptomes, and detect Rfx1,2,3,5 and 7 in the developing HCs. To understand the role of RFX in hearing, we generate Rfx1/3 conditional knockout mice. We show that these mice are deaf secondary to rapid loss of initially well-formed outer HCs. These data identify an essential role for RFX in hearing and survival of the terminally differentiating outer HCs. 1 Department of Human Molecular Genetics and Biochemistry, Sackler School of Medicine, Tel Aviv University, Tel Aviv 69978, Israel. -

Whole Genome Sequence Analysis of the TALLYHO/Jng Mouse James Denvir Marshall University, [email protected]
Marshall University Marshall Digital Scholar Biochemistry and Microbiology Faculty Research 2016 Whole genome sequence analysis of the TALLYHO/Jng mouse James Denvir Marshall University, [email protected] Goran Boskovic Marshall University Jun Fan Marshall University, [email protected] Donald A. Primerano Marshall University, [email protected] Jacaline K. Parkman Marshall University, [email protected] See next page for additional authors Follow this and additional works at: http://mds.marshall.edu/sm_bm Part of the Medical Pharmacology Commons, and the Medicinal and Pharmaceutical Chemistry Commons Recommended Citation Denvir J, Boskovic G, Fan J, Primerano DA, Parkman JK, Kim JH. Whole genome sequence analysis of the TALLYHO/Jng mouse. BMC Genomics. 2016;17:907. doi:10.1186/s12864-016-3245-6. This Article is brought to you for free and open access by the Faculty Research at Marshall Digital Scholar. It has been accepted for inclusion in Biochemistry and Microbiology by an authorized administrator of Marshall Digital Scholar. For more information, please contact [email protected], [email protected]. Authors James Denvir, Goran Boskovic, Jun Fan, Donald A. Primerano, Jacaline K. Parkman, and Jung Han Kim This article is available at Marshall Digital Scholar: http://mds.marshall.edu/sm_bm/204 Denvir et al. BMC Genomics (2016) 17:907 DOI 10.1186/s12864-016-3245-6 RESEARCHARTICLE Open Access Whole genome sequence analysis of the TALLYHO/Jng mouse James Denvir, Goran Boskovicˆ, Jun Fan, Donald A. Primerano, Jacaline K. Parkman and Jung Han Kim* Abstract Background: The TALLYHO/Jng (TH) mouse is a polygenic model for obesity and type 2 diabetes first described in the literature in 2001. -

Disruption of SF3B1 Results in Deregulated Expression And
Disruption of SF3B1 results in deregulated expression and splicing of key genes and pathways in myelodysplastic syndrome hematopoietic stem and progenitor cells Dolatshad, H., Pellagatti, A., Fernandez-Mercado, M., Yip, BH., Malcovati, L., Attwood, M., Przychodzen, B., Sahgal, N., Kanapin, AA., Lockstone, H., Scifo, L., Vandenberghe, P., Papaemmanuil, E., Smith, CWJ., Campbell, PJ., Ogawa, S., Maciejewski, JP., Cazzola, M., Savage, KI., & Boultwood, J. (2015). Disruption of SF3B1 results in deregulated expression and splicing of key genes and pathways in myelodysplastic syndrome hematopoietic stem and progenitor cells. Leukemia, 29(5), 1092-1103. https://doi.org/10.1038/leu.2014.331 Published in: Leukemia Document Version: Publisher's PDF, also known as Version of record Queen's University Belfast - Research Portal: Link to publication record in Queen's University Belfast Research Portal Publisher rights © 2014 The authors This is an open access article published under a Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution and reproduction in any medium, provided the author and source are cited. General rights Copyright for the publications made accessible via the Queen's University Belfast Research Portal is retained by the author(s) and / or other copyright owners and it is a condition of accessing these publications that users recognise and abide by the legal requirements associated with these rights. Take down policy The Research Portal is Queen's institutional repository that provides access to Queen's research output. Every effort has been made to ensure that content in the Research Portal does not infringe any person's rights, or applicable UK laws. -

Mouse Models of Inherited Retinal Degeneration with Photoreceptor Cell Loss
cells Review Mouse Models of Inherited Retinal Degeneration with Photoreceptor Cell Loss 1, 1, 1 1,2,3 1 Gayle B. Collin y, Navdeep Gogna y, Bo Chang , Nattaya Damkham , Jai Pinkney , Lillian F. Hyde 1, Lisa Stone 1 , Jürgen K. Naggert 1 , Patsy M. Nishina 1,* and Mark P. Krebs 1,* 1 The Jackson Laboratory, Bar Harbor, Maine, ME 04609, USA; [email protected] (G.B.C.); [email protected] (N.G.); [email protected] (B.C.); [email protected] (N.D.); [email protected] (J.P.); [email protected] (L.F.H.); [email protected] (L.S.); [email protected] (J.K.N.) 2 Department of Immunology, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok 10700, Thailand 3 Siriraj Center of Excellence for Stem Cell Research, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok 10700, Thailand * Correspondence: [email protected] (P.M.N.); [email protected] (M.P.K.); Tel.: +1-207-2886-383 (P.M.N.); +1-207-2886-000 (M.P.K.) These authors contributed equally to this work. y Received: 29 February 2020; Accepted: 7 April 2020; Published: 10 April 2020 Abstract: Inherited retinal degeneration (RD) leads to the impairment or loss of vision in millions of individuals worldwide, most frequently due to the loss of photoreceptor (PR) cells. Animal models, particularly the laboratory mouse, have been used to understand the pathogenic mechanisms that underlie PR cell loss and to explore therapies that may prevent, delay, or reverse RD. Here, we reviewed entries in the Mouse Genome Informatics and PubMed databases to compile a comprehensive list of monogenic mouse models in which PR cell loss is demonstrated. -
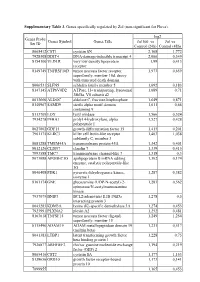
Supplementary Table 3. Genes Specifically Regulated by Zol (Non-Significant for Fluva)
Supplementary Table 3. Genes specifically regulated by Zol (non-significant for Fluva). log2 Genes Probe Genes Symbol Genes Title Zol100 vs Zol vs Set ID Control (24h) Control (48h) 8065412 CST1 cystatin SN 2,168 1,772 7928308 DDIT4 DNA-damage-inducible transcript 4 2,066 0,349 8154100 VLDLR very low density lipoprotein 1,99 0,413 receptor 8149749 TNFRSF10D tumor necrosis factor receptor 1,973 0,659 superfamily, member 10d, decoy with truncated death domain 8006531 SLFN5 schlafen family member 5 1,692 0,183 8147145 ATP6V0D2 ATPase, H+ transporting, lysosomal 1,689 0,71 38kDa, V0 subunit d2 8013660 ALDOC aldolase C, fructose-bisphosphate 1,649 0,871 8140967 SAMD9 sterile alpha motif domain 1,611 0,66 containing 9 8113709 LOX lysyl oxidase 1,566 0,524 7934278 P4HA1 prolyl 4-hydroxylase, alpha 1,527 0,428 polypeptide I 8027002 GDF15 growth differentiation factor 15 1,415 0,201 7961175 KLRC3 killer cell lectin-like receptor 1,403 1,038 subfamily C, member 3 8081288 TMEM45A transmembrane protein 45A 1,342 0,401 8012126 CLDN7 claudin 7 1,339 0,415 7993588 TMC7 transmembrane channel-like 7 1,318 0,3 8073088 APOBEC3G apolipoprotein B mRNA editing 1,302 0,174 enzyme, catalytic polypeptide-like 3G 8046408 PDK1 pyruvate dehydrogenase kinase, 1,287 0,382 isozyme 1 8161174 GNE glucosamine (UDP-N-acetyl)-2- 1,283 0,562 epimerase/N-acetylmannosamine kinase 7937079 BNIP3 BCL2/adenovirus E1B 19kDa 1,278 0,5 interacting protein 3 8043283 KDM3A lysine (K)-specific demethylase 3A 1,274 0,453 7923991 PLXNA2 plexin A2 1,252 0,481 8163618 TNFSF15 tumor necrosis -

(12) United States Patent (10) Patent No.: US 8,361,780 B2 Gaertig Et Al
USOO836.1780B2 (12) United States Patent (10) Patent No.: US 8,361,780 B2 Gaertig et al. (45) Date of Patent: Jan. 29, 2013 (54) BIOLOGICAL SYSTEMAND ASSAY FOR Adoutte et al., “Microtubule diversity in ciliated cells: evidence for its IDENTIFYING MODULATORS OF TUBULIN generation by post-translational modification in the axonemes of LGASES Paramecium and quail oviduct cells.” 1991 Biol. Cell 71:227-245. Alexander et al., "Characterization of posttranslational modifications in neuron-specific class III beta-tubulin by mass spectrometry.” Jun. (75) Inventors: Jacek Gaertig, Athens, GA (US); 1, 1991 Proc. Natl. Acad. Sci. USA 88:4685-4689. Dorota Wloga, Legionowo (PL); Swati Artymiuket al., “Biotin carboxylase comes into the fold.” Feb. 1996 M. Suryavanshi, Pittsburgh, PA (US) Nat. Struct. Biol. 3:128-132. Attwell et al., “A temperature-sensitive mutation affecting synthesis (73) Assignee: University of Georgia Research of outer arm dyneins in Tetrahymena thermophila.” Mar.-Apr. 1992.J. Foundation, Inc., Athens, GA (US) Protozool. 39,261-266. Audebert et al., “Reversible Polyglutamylation of O- and B-Tubulin (*) Notice: Subject to any disclaimer, the term of this and Microtubule Dynamics in Mouse Brain Neurons.” Jun. 1993 patent is extended or adjusted under 35 Mol. Biol. Cell 4:615-626. U.S.C. 154(b) by 241 days. Audebert et al., “Developmental regulation of polyglutamylated alpha- and beta-tubulin in mouse brain neurons.” Aug. 1994.J. Cell (21) Appl. No.: 12/6S8,487 Sci. 107(Pt. 8): 2313-2322. Backofen et al., “Cloning and characterization of the mammalian (22) Filed: Feb. 5, 2010 specific nicolin 1 gene (NICNI) encoding a nuclear 24 kDa protein.” Nov. -

Human Population History and Genetic Adaptation in the Himalayan Region
Human population history and genetic adaptation in the Himalayan region University of Cambridge Corpus Christi College A thesis submitted for the degree of Doctor of Philosophy Elena Arciero The Wellcome Sanger Institute Wellcome Genome Campus Hinxton, Cambridge CB10 1SA, UK September 2018 2 3 To my parents, Cristina and Virgilio 4 5 Declaration I hereby declare that except where specific reference is made to the work of others, the contents of this dissertation are original and have not been submitted in whole or in part for consideration for any other degree or qualification at the University of Cambridge or any other University or similar institution. This dissertation is my own work carried out under the supervision of Prof. Chris Tyler- Smith at the Wellcome Sanger Institute, while a member of Corpus Christi College, University of Cambridge, and contains nothing which is the outcome of work done in collaboration with others, except as specified in the text and Acknowledgements. This dissertation does not exceed the prescribed word limit of 60,000 words excluding bibliography, figures, tables, equations and appendices. Elena Arciero September 2018 6 7 Acknowledgements First and foremost I would like to express my sincere gratitude to my supervisor Dr Chris Tyler-Smith for giving me the opportunity to carry out this project and for his continuous support, advice and mentorship during my PhD. I would like to thank Dr Yali Xue and Dr Qasim Ayub for their guidance and for their critical and constructive assessment of my work. I would also like to thank Dr Marc Haber for his help in the day to day work. -

Table S1. 103 Ferroptosis-Related Genes Retrieved from the Genecards
Table S1. 103 ferroptosis-related genes retrieved from the GeneCards. Gene Symbol Description Category GPX4 Glutathione Peroxidase 4 Protein Coding AIFM2 Apoptosis Inducing Factor Mitochondria Associated 2 Protein Coding TP53 Tumor Protein P53 Protein Coding ACSL4 Acyl-CoA Synthetase Long Chain Family Member 4 Protein Coding SLC7A11 Solute Carrier Family 7 Member 11 Protein Coding VDAC2 Voltage Dependent Anion Channel 2 Protein Coding VDAC3 Voltage Dependent Anion Channel 3 Protein Coding ATG5 Autophagy Related 5 Protein Coding ATG7 Autophagy Related 7 Protein Coding NCOA4 Nuclear Receptor Coactivator 4 Protein Coding HMOX1 Heme Oxygenase 1 Protein Coding SLC3A2 Solute Carrier Family 3 Member 2 Protein Coding ALOX15 Arachidonate 15-Lipoxygenase Protein Coding BECN1 Beclin 1 Protein Coding PRKAA1 Protein Kinase AMP-Activated Catalytic Subunit Alpha 1 Protein Coding SAT1 Spermidine/Spermine N1-Acetyltransferase 1 Protein Coding NF2 Neurofibromin 2 Protein Coding YAP1 Yes1 Associated Transcriptional Regulator Protein Coding FTH1 Ferritin Heavy Chain 1 Protein Coding TF Transferrin Protein Coding TFRC Transferrin Receptor Protein Coding FTL Ferritin Light Chain Protein Coding CYBB Cytochrome B-245 Beta Chain Protein Coding GSS Glutathione Synthetase Protein Coding CP Ceruloplasmin Protein Coding PRNP Prion Protein Protein Coding SLC11A2 Solute Carrier Family 11 Member 2 Protein Coding SLC40A1 Solute Carrier Family 40 Member 1 Protein Coding STEAP3 STEAP3 Metalloreductase Protein Coding ACSL1 Acyl-CoA Synthetase Long Chain Family Member 1 Protein