Cutaneous Amebiasis: 50 Years of Experience
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Index Vol. 12-15
353 INDEX VOL. 12-15 Die Stichworte des Sachregisters sind in der jeweiligen Sprache der einzelnen Beitrage aufgefiihrt. Les termes repris dans la Table des matieres sont donnes selon la langue dans laquelle l'ouvrage est ecrit. The references of the Subject Index are given in the language of the respective contribution. 14 AAG (Alpha-acid glycoprotein) 120 14 Adenosine 108 12 Abortion 151 12 Adenosine-phosphate 311 13 Abscisin 12, 46, 66 13 Adenosine-5'-phosphosulfate 148 14 Absorbierbarkeit 317 13 Adenosine triphosphate 358 14 Absorption 309, 350 15 S-Adenosylmethionine 261 13 Absorption of drugs 139 13 Adipaenin (Spasmolytin) 318 14 - 15 12 Adrenal atrophy 96 14 Absorptionsgeschwindigkeit 300, 306 14 - 163, 164 14 Absorptionsquote 324 13 Adrenal gland 362 14 ACAI (Anticorticocatabolic activity in 12 Adrenalin(e) 319 dex) 145 14 - 209, 210 12 Acalo 197 15 - 161 13 Aceclidine (3-Acetoxyquinuclidine) 307, 13 {i-Adrenergic blockers 119 308, 310, 311, 330, 332 13 Adrenergic-blocking activity 56 13 Acedapsone 193,195,197 14 O(-Adrenergic blocking drugs 36, 37, 43 13 Aceperone (Acetabutone) 121 14 {i-Adrenergic blocking drugs 38 12 Acepromazin (Plegizil) 200 14 Adrenergic drugs 90 15 Acetanilid 156 12 Adrenocorticosteroids 14, 30 15 Acetazolamide 219 12 Adrenocorticotropic hormone (ACTH) 13 Acetoacetyl-coenzyme A 258 16,30,155 12 Acetohexamide 16 14 - 149,153,163,165,167,171 15 1-Acetoxy-8-aminooctahydroindolizin 15 Adrenocorticotropin (ACTH) 216 (Slaframin) 168 14 Adrenosterone 153 13 4-Acetoxy-1-azabicyclo(3, 2, 2)-nonane 12 Adreson 252 -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -
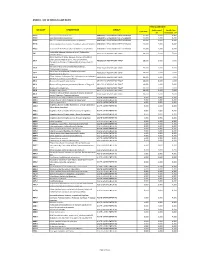
Annex 1: List of Medical Case Rates
ANNEX 1. LIST OF MEDICAL CASE RATES FIRST CASE RATE ICD CODE DESCRIPTION GROUP Professional Health Care Case Rate Fee Institution Fee P91.3 Neonatal cerebral irritability ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 P91.4 Neonatal cerebral depression ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 P91.6 Hypoxic ischemic encephalopathy of newborn ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 P91.8 Other specified disturbances of cerebral status of newborn ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 P91.9 Disturbance of cerebral status of newborn, unspecified ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 Peritonsillar abscess; Abscess of tonsil; Peritonsillar J36 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 cellulitis; Quinsy Other diseases of larynx; Abscess of larynx; Cellulitis of larynx; Disease NOS of larynx; Necrosis of larynx; J38.7 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 Pachyderma of larynx; Perichondritis of larynx; Ulcer of larynx Retropharyngeal and parapharyngeal abscess; J39.0 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 Peripharyngeal abscess Other abscess of pharynx; Cellulitis of pharynx; J39.1 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 Nasopharyngeal abscess Other diseases of pharynx; Cyst of pharynx or nasopharynx; J39.2 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 Oedema of pharynx or nasopharynx J85.1 Abscess of lung with pneumonia ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 J85.2 Abscess of lung without pneumonia; Abscess of lung NOS ABSCESS OF RESPIRATORY -

Natural Remedies of Common Human Parasites and Pathogens
ACTA SCIENTIFIC MICROBIOLOGY (ISSN: 2581-3226) Volume 2 Issue 11 November 2019 Investigation Paper Natural Remedies of Common Human Parasites and Pathogens Omar M Amin* Parasitology Center, Scottsdale, Arizona *Corresponding Author: Omar M Amin, Parasitology Center, Scottsdale, Arizona. Received: July 12, 2019; Published: October 16, 2019 DOI: 10.31080/ASMI.2019.02.0401 • Bleeding. • Appetite changes. • Malabsorption. • Mucus. • Rectal itching. • Gut leakage. • Poor digestion. • Systemic/other symptoms • Fatigue. • Skin rash. • Dry cough. • Brain fog/memory loss. • Lymph blockage. Figure 1 • Allergies. • Nausea. Diagnosis and management of: • Muscle or joint pain. • Parasitic organisms and agents of medical and public • Dermatitis. health importance in fecal, blood, skin, urine specimens. • Headaches. • Toxicities related to Neurocutaneous Syndrome (NCS). • Insomnia. Development of anti-parasitic herbal products (F/C/R) Edu- How we get infected cational services: workshops, seminars, training and publications Drinking water or juice: Giardia, Cryptosporidium. provided. 1. 2. Skin contact with contaminated water: Schistosomi- Consultations and protocols for herbal and allopathic treat- asis, swimmers itch. ments. Research: over 220 publications on parasites from all con- Food (fecal-oral infections): most protozoans, ex., tinents. 3. Blastocysts, Entamoeba spp. and worms: Ascaris. Why test? 4. Arthropods: Lyme disease, plague, typhus, etc. You need to be tested if you have one or more of these symp- 5. Air: Upper respiratory tract infections (viruses, bac- toms: teria), ex GI symptoms 6. Pets: Hydatid., flu, Valleycyst disease,fever, Hanta heart virus. worm, larva mi- grans (dogs), Toxoplasma (cats), Taenia (beef, swine. • Diarrhea/constipation. People (contagious diseases): AIDS, herpes. • Irritable bowel 7. Soil: hook worms, thread worms. • Cramps 8. -
![Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set](https://docslib.b-cdn.net/cover/8870/ehealth-dsi-ehdsi-v2-2-2-or-ehealth-dsi-master-value-set-1028870.webp)
Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set
MTC eHealth DSI [eHDSI v2.2.2-OR] eHealth DSI – Master Value Set Catalogue Responsible : eHDSI Solution Provider PublishDate : Wed Nov 08 16:16:10 CET 2017 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 1 of 490 MTC Table of Contents epSOSActiveIngredient 4 epSOSAdministrativeGender 148 epSOSAdverseEventType 149 epSOSAllergenNoDrugs 150 epSOSBloodGroup 155 epSOSBloodPressure 156 epSOSCodeNoMedication 157 epSOSCodeProb 158 epSOSConfidentiality 159 epSOSCountry 160 epSOSDisplayLabel 167 epSOSDocumentCode 170 epSOSDoseForm 171 epSOSHealthcareProfessionalRoles 184 epSOSIllnessesandDisorders 186 epSOSLanguage 448 epSOSMedicalDevices 458 epSOSNullFavor 461 epSOSPackage 462 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 2 of 490 MTC epSOSPersonalRelationship 464 epSOSPregnancyInformation 466 epSOSProcedures 467 epSOSReactionAllergy 470 epSOSResolutionOutcome 472 epSOSRoleClass 473 epSOSRouteofAdministration 474 epSOSSections 477 epSOSSeverity 478 epSOSSocialHistory 479 epSOSStatusCode 480 epSOSSubstitutionCode 481 epSOSTelecomAddress 482 epSOSTimingEvent 483 epSOSUnits 484 epSOSUnknownInformation 487 epSOSVaccine 488 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 3 of 490 MTC epSOSActiveIngredient epSOSActiveIngredient Value Set ID 1.3.6.1.4.1.12559.11.10.1.3.1.42.24 TRANSLATIONS Code System ID Code System Version Concept Code Description (FSN) 2.16.840.1.113883.6.73 2017-01 A ALIMENTARY TRACT AND METABOLISM 2.16.840.1.113883.6.73 2017-01 -

Bacterial Brain Abscess in a Patient with Granulomatous Amebic Encephalitis
SVOA Neurology ISSN: 2753-9180 Case Report Bacterial Brain Abscess in a Patient with Granulomatous Amebic Encephalitis. A Misdiagnosis or Free-Living Amoeba Acting as Trojan Horse? Rolando Lovaton1* and Wesley Alaba1 1 Hospital Nacional Cayetano Heredia (Lima-Peru) *Corresponding Author: Dr. Rolando Lovaton, Neurosurgery Service-Hospital Nacional Cayetano Heredia, Avenida Honorio Delgado 262 San Martin de Porres, Lima-Peru Received: July 13, 2021 Published: July 24, 2021 Abstract Amebic encephalitis is a rare and devastating disease. Mortality rate is almost 90% of cases. Here is described a very rare case of bacterial brain abscess in a patient with recent diagnosis of granulomatous amebic encephalitis. Case De- scription: A 29-year-old woman presented with headache, right hemiparesis and tonic-clonic seizure. Patient was diag- nosed with granulomatous amebic encephalitis due to Acanthamoeba spp.; although, there was no improvement of symptoms in spite of stablished treatment. Three months after initial diagnosis, a brain MRI showed a ring-enhancing lesion in the left frontal lobe compatible with brain abscess. Patient was scheduled for surgical evacuation and brain abscess was confirmed intraoperatively. However, Gram staining of the purulent content showed gram-positive cocci. Patient improved headache and focal deficit after surgery. Conclusion: It is the first reported case of a patient with cen- tral nervous system infection secondary to Acanthamoeba spp. who presented a bacterial brain abscess in a short time. Keywords: amebic encephalitis; Acanthamoeba spp; bacterial brain abscess Introduction Free–living amoebae cause potentially fatal infection of central nervous system. Two clinical entities have been de- scribed for amebic encephalitis: primary amebic meningoencephalitis (PAM), and granulomatous amebic encephalitis (GAE). -

Developing Novel Therapeutic Agents for Acanthamoeba Infection and Investigating the Process of Encystment
Developing novel therapeutic agents for Acanthamoeba infection and investigating the process of encystment Anas Abdullah Hamad (BSc, MSc) A thesis submitted in partial fulfilment of the requirements of the University of Wolverhampton for the degree of Doctor of Philosophy June 2020 Declaration This work or any part thereof has not previously been presented in any form to the University or to any other body whether for the purposes of assessment, publication or for any other purpose (unless otherwise indicated in page 3). Save for any express acknowledgements, references and/or bibliographies cited in the work, I confirm that the intellectual content of the work is the result of my own efforts and of no other person. The right of Anas Abdullah Hamad to be identified as author of this work is asserted in accordance with ss.77 and 78 of the Copyright, Designs and Patents Act 1988. At this date copyright is owned by the author. Signature………………………………………. Date……………………………………………. 15/10/2020 2 List of posters and publication related to the work presented in this thesis: Heaselgrave, W., Hamad, A., Coles, S. and Hau, S., 2019. In Vitro Evaluation of the Inhibitory Effect of Topical Ophthalmic Agents on Acanthamoeba Viability. Translational vision science & technology, 8(5), pp.17-17. Manuscript published. Hamad, A. and Heaselgrave, W., 2017. Developing novel treatments for the blinding protozoan eye infection Acanthamoeba keratitis. Proceedings of the Internal Annual Research Symposium, Poster no. 23, University of Wolverhampton, UK. Hamad, A. and Heaselgrave, W., 2018. Developing new treatments and optimising existing treatment strategies for the corneal infection Acanthamoeba keratitis. -

This Thesis Has Been Submitted in Fulfilment of the Requirements for a Postgraduate Degree (E.G
This thesis has been submitted in fulfilment of the requirements for a postgraduate degree (e.g. PhD, MPhil, DClinPsychol) at the University of Edinburgh. Please note the following terms and conditions of use: This work is protected by copyright and other intellectual property rights, which are retained by the thesis author, unless otherwise stated. A copy can be downloaded for personal non-commercial research or study, without prior permission or charge. This thesis cannot be reproduced or quoted extensively from without first obtaining permission in writing from the author. The content must not be changed in any way or sold commercially in any format or medium without the formal permission of the author. When referring to this work, full bibliographic details including the author, title, awarding institution and date of the thesis must be given. Protein secretion and encystation in Acanthamoeba Alvaro de Obeso Fernández del Valle Doctor of Philosophy The University of Edinburgh 2018 Abstract Free-living amoebae (FLA) are protists of ubiquitous distribution characterised by their changing morphology and their crawling movements. They have no common phylogenetic origin but can be found in most protist evolutionary branches. Acanthamoeba is a common FLA that can be found worldwide and is capable of infecting humans. The main disease is a life altering infection of the cornea named Acanthamoeba keratitis. Additionally, Acanthamoeba has a close relationship to bacteria. Acanthamoeba feeds on bacteria. At the same time, some bacteria have adapted to survive inside Acanthamoeba and use it as transport or protection to increase survival. When conditions are adverse, Acanthamoeba is capable of differentiating into a protective cyst. -

Cutaneous Balamuthia Mandrillaris Infection As a Precursor To
Volume 23 Number 7 | July 2017 Dermatology Online Journal || Case Report DOJ 23 (7): 4 Cutaneous Balamuthia mandrillaris infection as a precursor to Balamuthia amoebic encephalitis (BAE) in a healthy 84-year-old Californian Larisa M Lehmer, Gabriel E Ulibarri, Bruce D Ragsdale, James Kunkle Affiliations: University of California Irvine Health, Department of Dermatology, Irvine, California, Central Coast Pathology Laboratory, San Luis Obispo, California, Western Diagnostic Services Laboratory, San Luis Obispo, California, Central Coast Dermatology, Arroyo Grande, California Corresponding Author: Larisa M Lehmer, Department of Dermatology, UC Irvine Health, 118 Med Surg 1, Irvine, CA 92697-2400, Email: [email protected] Abstract Keywords: Balamuthia mandrillaris; cutaneous balamuthiasis; granulomatous amoebic encephalitis; Soil and freshwater-dwelling amoebae may GAE; balamuthia amoebic encephalitis; BAE; opportunistically infect the skin and evoke a immunocompromise; granulomatous dermatitis; granulomatous dermatitis that camouflages their immune senescence. underlying morphology. Amoebic infestations are incredibly rare in the U.S., predominantly occurring in the young, elderly, and immunocompromised. Introduction Sadly, because diagnosis is difficult and unsuspected, Balamuthia mandrillaris (B. mandrillaris), along most cases are diagnosed at autopsy. The following with Naegleria, Sappinia and several species of case is of a healthy 84-year-old man with a non- Acanthomeba, are free-living amoebae found in fresh healing nodulo-ulcerative cutaneous lesion on his water and soil worldwide that may opportunistically left forearm that appeared following a gardening infect the skin and/or central nervous system (CNS) injury. Lesional punch biopsies repeatedly showed of humans. The first sign of infection ranges from non-specific granulomatous inflammation with a stubborn indurated plaque or ulceration on the no pathogens evident histologically or by culture. -

Cutaneous Amebiasis in Pediatrics
OBSERVATION Cutaneous Amebiasis in Pediatrics Mario L. Magan˜a, MD; Jorge Ferna´ndez-Dı´ez, MD; Mario Magan˜a,MD Background: Cutaneous amebiasis (CA), which is still Conclusions: Cutaneous amebiasis always presents with a health problem in developing countries, is important painful ulcers. The ulcers are laden with amebae, which to diagnose based on its clinical and histopathologic are relatively easy to see microscopically with routine features. stains. Erythrophagocytosis is an unequivocal sign of CA. Amebae reach the skin via 2 mechanisms: direct and in- Observations: Retrospective medical record review of direct. Amebae are able to reach the skin if there is a lac- 26 patients with CA (22 adults and 4 children) treated from eration (port of entry) and if conditions in the patient 1955 to 2005 was performed. In addition to the age and are favorable. Amebae are able to destroy tissues by means sex of the patients, the case presentation, associated ill- of their physical activity, phagocytosis, enzymes, secre- ness or factors, and method of establishing the diagnosis, tagogues, and other molecules. clinical pictures and microscopic slides were also analyzed. Arch Dermatol. 2008;144(10):1369-1372 UTANEOUS AMEBIASIS (CA) ria, are opportunistic organisms that act as can be defined as damage pathogens, usually in the immunocompro- to the skin and underly- mised host, who can develop disease in any ing soft tissues by tropho- organ, such as the skin and central ner- zoites of Entamoeba histo- vous system. This kind of amebiasis has be- lytica, the only pathogenic form for humans. come more common during the last few C 8-18 Cutaneous amebiasis may be the only ex- years. -

Pathogenic Free Living Amoeba
Middle Black Sea Journal of Health Science August 2015; 1(2): 13-20 REVIEW Risks and Threats Comes with Global Warming: Pathogenic Free Living Amoeba Nihal Doğan1 1Osmangazi University Medical Faculty Microbiology Department. Eskişehir, Turkey Received: 28 July 2015 accepted: 12 August 2015/ published online: 30 August 2015 © Ordu University Institute of Health Science, Turkey, 2015 Abstract Free living amoebae like Naegleria, Acanthamoeba, Balamuthia and Sappinia are known appearing opportunistic and also fatal protozoa in humans and other animals. They are widely distributed in soil and water in the world. They cause “Primer Amoebic Meningoencephalitis” the host immune response to these protist pathogens differs from each other to evidence by the postmortem laboratory findings from the affected patients. This review was performed with a search in Medline, PubMed, Science Direct, Ovid, and Scopus literatures by the search terms of “pathogenic free-living amoeba infections”. Analysis of a detailed review and literature shown that Naegleria fowleri, Acanthamoeba and Balamuthia and also Sappinia sp. infections are causing extensive brain damage to the host immune response. In human infection due to related to brain, skin, lung and eyes have increased significantly during the last years. They have different effects on epidemiology, immunology, pathology, and clinical features of the infections produced. This particular review planned to raise awareness about free-living amoeba, which found in a patient who applied to ESOGU Hospital Neurology Clinic because of suddenly unconsciousness and coma and diagnosed with Naegleria fowleri. Clinicians should be aware of PAM infections and include in differential diagnosis of meningoencephalitis. PAM should be suspected in young adults and children with acute neurological symptoms as described below and recent exposure to fresh water. -

Die Prinzipien Der Chirurgischen Therapie Beim Fortgeschrittenen
Aus der Chirurgischen Klinik und Poliklinik - Innenstadt, der Ludwig-Maximilian- Universität-München Direktor: Prof. Dr. med. Wolf Mutschler Die Prinzipien der chirurgischen Therapie beim fortgeschrittenen Pyoderma gangränosum Dissertation zum Erwerb des Doktorgrades der Medizin an der Medizinischen Fakultät der Ludwig-Maximilians-Universität zu München vorgelegt von Christoph Hendrik Volkering aus Groß-Gerau 2008 Mit Genehmigung der Medizinischen Fakultät der Universität München Berichterstatter: Prof. Dr. Sigurd Keßler Mitberichterstatter: Prof. Dr. Hans C. Korting Priv. Doz. Dr. Martin K. Angele Dekan: Prof. Dr. med. Dr. h.c. Maximilian Reiser, FACR Tag der mündlichen Prüfung: 20.11.2008 - 2 - INHALT 1. Einleitung: ........................................................................................................... - 6 - 1.1. Das Pyoderma gangränosum: ..................................................................... - 6 - 1.1.1. Geschichte: ......................................................................................... - 6 - 1.1.2. Inzidenz: ............................................................................................. - 6 - 1.1.3. Assoziierte Erkrankungen: .................................................................. - 7 - 1.1.4. Typen des Pyoderma gangränosum: .................................................. - 9 - 1.1.5. Histopathologie: ................................................................................ - 12 - 1.1.6. Pathogenese: ...................................................................................