A Review of Facial Nerve Anatomy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharnygeal Arch Set - Motor USMLE, Limited Edition > Neuroscience > Neuroscience
CNs 5, 7, 9, 10 - Pharnygeal Arch Set - Motor USMLE, Limited Edition > Neuroscience > Neuroscience PHARYNGEAL ARCH SET, CNS 5, 7, 9, 10 • They are derived from the pharyngeal (aka branchial) arches • They have special motor and autonomic motor functions CRANIAL NERVES EXIT FROM THE BRAINSTEM CN 5, the trigeminal nerve exits the mid/lower pons.* CN 7, the facial nerve exits the pontomedullary junction.* CN 9, the glossopharyngeal nerve exits the lateral medulla.* CN 10, the vagus nerve exits the lateral medulla.* CRANIAL NERVE NUCLEI AT BRAINSTEM LEVELS Midbrain • The motor trigeminal nucleus of CN 5. Nerve Path: • The motor division of the trigeminal nerve passes laterally to enter cerebellopontine angle cistern. Pons • The facial nucleus of CN 7. • The superior salivatory nucleus of CN 7. Nerve Path: • CN 7 sweeps over the abducens nucleus as it exits the brainstem laterally in an internal genu, which generates a small bump in the floor of the fourth ventricle: the facial colliculus • Fibers emanate from the superior salivatory nucleus, as well. Medulla • The dorsal motor nucleus of the vagus, CN 10 • The inferior salivatory nucleus, CN 9 1 / 3 • The nucleus ambiguus, CNs 9 and 10. Nerve Paths: • CNs 9 and 10 exit the medulla laterally through the post-olivary sulcus to enter the cerebellomedullary cistern. THE TRIGEMINAL NERVE, CN 5  • The motor division of the trigeminal nerve innervates the muscles of mastication • It passes ventrolaterally through the cerebellopontine angle cistern and exits through foramen ovale as part of the mandibular division (CN 5[3]). Clinical Correlation - Trigeminal Neuropathy THE FACIAL NERVE, CN 7  • The facial nucleus innervates the muscles of facial expression • It spans from the lower pons to the pontomedullary junction. -
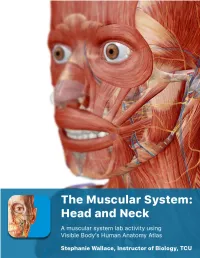
The Muscular System Views
1 PRE-LAB EXERCISES Before coming to lab, get familiar with a few muscle groups we’ll be exploring during lab. Using Visible Body’s Human Anatomy Atlas, go to the Views section. Under Systems, scroll down to the Muscular System views. Select the view Expression and find the following muscles. When you select a muscle, note the book icon in the content box. Selecting this icon allows you to read the muscle’s definition. 1. Occipitofrontalis (epicranius) 2. Orbicularis oculi 3. Orbicularis oris 4. Nasalis 5. Zygomaticus major Return to Muscular System views, select the view Head Rotation and find the following muscles. 1. Sternocleidomastoid 2. Scalene group (anterior, middle, posterior) 2 IN-LAB EXERCISES Use the following modules to guide your exploration of the head and neck region of the muscular system. As you explore the modules, locate the muscles on any charts, models, or specimen available. Please note that these muscles act on the head and neck – those that are located in the neck but act on the back are in a separate section. When reviewing the action of a muscle, it will be helpful to think about where the muscle is located and where the insertion is. Muscle physiology requires that a muscle will “pull” instead of “push” during contraction, and the insertion is the part that will move. Imagine that the muscle is “pulling” on the bone or tissue it is attached to at the insertion. Access 3D views and animated muscle actions in Visible Body’s Human Anatomy Atlas, which will be especially helpful to visualize muscle actions. -

Neuroanatomy Crash Course
Neuroanatomy Crash Course Jens Vikse ∙ Bendik Myhre ∙ Danielle Mellis Nilsson ∙ Karoline Hanevik Illustrated by: Peder Olai Skjeflo Holman Second edition October 2015 The autonomic nervous system ● Division of the autonomic nervous system …………....……………………………..………….…………... 2 ● Effects of parasympathetic and sympathetic stimulation…………………………...……...……………….. 2 ● Parasympathetic ganglia ……………………………………………………………...…………....………….. 4 Cranial nerves ● Cranial nerve reflexes ………………………………………………………………….…………..…………... 7 ● Olfactory nerve (CN I) ………………………………………………………………….…………..…………... 7 ● Optic nerve (CN II) ……………………………………………………………………..…………...………….. 7 ● Pupillary light reflex …………………………………………………………………….…………...………….. 7 ● Visual field defects ……………………………………………...................................…………..………….. 8 ● Eye dynamics …………………………………………………………………………...…………...………….. 8 ● Oculomotor nerve (CN III) ……………………………………………………………...…………..………….. 9 ● Trochlear nerve (CN IV) ………………………………………………………………..…………..………….. 9 ● Trigeminal nerve (CN V) ……………………………………………………................…………..………….. 9 ● Abducens nerve (CN VI) ………………………………………………………………..…………..………….. 9 ● Facial nerve (CN VII) …………………………………………………………………...…………..………….. 10 ● Vestibulocochlear nerve (CN VIII) …………………………………………………….…………...…………. 10 ● Glossopharyngeal nerve (CN IX) …………………………………………….……….…………...………….. 10 ● Vagus nerve (CN X) …………………………………………………………..………..…………...………….. 10 ● Accessory nerve (CN XI) ……………………………………………………...………..…………..………….. 11 ● Hypoglossal nerve (CN XII) …………………………………………………..………..…………...…………. -

Cranial Nerve Palsy
Cranial Nerve Palsy What is a cranial nerve? Cranial nerves are nerves that lead directly from the brain to parts of our head, face, and trunk. There are 12 pairs of cranial nerves and some are involved in special senses (sight, smell, hearing, taste, feeling) while others control muscles and glands. Which cranial nerves pertain to the eyes? The second cranial nerve is called the optic nerve. It sends visual information from the eye to the brain. The third cranial nerve is called the oculomotor nerve. It is involved with eye movement, eyelid movement, and the function of the pupil and lens inside the eye. The fourth cranial nerve is called the trochlear nerve and the sixth cranial nerve is called the abducens nerve. They each innervate an eye muscle involved in eye movement. The fifth cranial nerve is called the trigeminal nerve. It provides facial touch sensation (including sensation on the eye). What is a cranial nerve palsy? A palsy is a lack of function of a nerve. A cranial nerve palsy may cause a complete or partial weakness or paralysis of the areas served by the affected nerve. In the case of a cranial nerve that has multiple functions (such as the oculomotor nerve), it is possible for a palsy to affect all of the various functions or only some of the functions of that nerve. What are some causes of a cranial nerve palsy? A cranial nerve palsy can occur due to a variety of causes. It can be congenital (present at birth), traumatic, or due to blood vessel disease (hypertension, diabetes, strokes, aneurysms, etc). -

Circuits in the Rodent Brainstem That Control Whisking in Concert with Other Orofacial Motor Actions
Neuroscience 368 (2018) 152–170 CIRCUITS IN THE RODENT BRAINSTEM THAT CONTROL WHISKING IN CONCERT WITH OTHER OROFACIAL MOTOR ACTIONS y y LAUREN E. MCELVAIN, a BETH FRIEDMAN, a provides the reset to the relevant premotor oscillators. HARVEY J. KARTEN, b KAREL SVOBODA, c FAN WANG, d Third, direct feedback from somatosensory trigeminal e a,f,g MARTIN DESCHEˆ NES AND DAVID KLEINFELD * nuclei can rapidly alter motion of the sensors. This feed- a Department of Physics, University of California at San Diego, back is disynaptic and can be tuned by high-level inputs. La Jolla, CA 92093, USA A holistic model for the coordination of orofacial motor actions into behaviors will encompass feedback pathways b Department of Neurosciences, University of California at San Diego School of Medicine, La Jolla, CA 92093, USA through the midbrain and forebrain, as well as hindbrain c areas. Howard Hughes Medical Institute, Janelia Research This article is part of a Special Issue entitled: Barrel Campus, Ashburn, VA 20147, USA Cortex. Ó 2017 IBRO. Published by Elsevier Ltd. All rights d Department of Neurobiology, Duke University Medical reserved. Center, Durham, NC 27710, USA e Department of Psychiatry and Neuroscience, Laval University, Que´bec City, G1J 2G3, Canada f Key words: coupled oscillators, facial nucleus, hypoglossal Section of Neurobiology, University of California at San Diego, La Jolla, CA 92093, USA nucleus, licking, orienting, tongue, vibrissa. g Department of Electrical and Computer Engineering, University of California at San Diego, La Jolla, CA 92093, USA Contents Introduction 153 Abstract—The world view of rodents is largely determined Coordination of multiple orofacial motor actions 153 by sensation on two length scales. -
Facial Nerve Disorders Cn7 (1)
FACIAL NERVE DISORDERS CN7 (1) Facial Nerve Disorders Last updated: January 18, 2020 FACIAL PALSY .......................................................................................................................................... 1 ETIOLOGY .............................................................................................................................................. 1 GUIDE TO LESION SITE LOCALIZATION ................................................................................................... 2 CLINICAL GRADING OF SEVERITY .......................................................................................................... 2 House-Brackmann grading scale ........................................................................................... 2 CLINICO-ANATOMICAL SYNDROMES ..................................................................................................... 2 Supranuclear (Central) Palsy ................................................................................................. 2 Nuclear Lesion ...................................................................................................................... 3 Cerebellopontine Angle Syndrome ....................................................................................... 3 Facial Canal Syndrome ......................................................................................................... 3 Stylomastoid Foramen Syndrome ........................................................................................ -

Facial-Stapedial Synkinesis Following Acute Idiopathic Facial Palsy
CASE REPORT Facial-Stapedial Synkinesis Following Acute Idiopathic Facial Palsy Michael Hutz, MD; Margaret Aasen; John Leonetti, MD ABSTRACT complete resolution of their unilateral Introduction: While most patients note a complete resolution of facial paralysis in Bell’s Palsy, facial paralysis, the remaining patients up to 30% will have persistent facial weakness and develop synkinesis. All branches of the manifest persistent paralysis or develop facial nerve are at risk for developing synkinesis, but stapedial synkinesis has rarely been synkinesis, which occurs when a volun- reported in the literature. tary muscle movement causes a simulta- Case Presentation: A 45-year-old man presented with sudden onset, complete right facial neous involuntary contraction of other paralysis. One-and-a-half years later, he had persistent facial weakness and synkinesis. He muscles. The facial nerve is the 7th cra- noted persistent right aural fullness and hearing loss. Audiometry demonstrated facial-stapedial nial nerve and is primarily affected in synkinesis. Bell’s Palsy. It acts to control the muscles Discussion: The patient was diagnosed with stapedial synkinesis based on audiometric find- of facial expression and conveys taste sen- ings by comparing his hearing at rest and with sustained facial mimetic movement. A literature sation to the anterior two-thirds of the review revealed 21 reported cases of this disorder. tongue. Faulty facial nerve regeneration fol- Conclusions: Facial-stapedial synkinesis is an underdiagnosed phenomenon for patients recov- ering from idiopathic facial palsy. Patients who develop facial synkinesis also may have a com- lowing Bell’s Palsy commonly leads to ponent of stapedial synkinesis and should be referred to an otolaryngologist if they complain abnormal muscle contractions of the eye, of any otologic symptoms, such as unilateral hearing loss or tinnitus. -

Neurophysiological Aspects of the Trigeminal Sensory System: an Update
Rev. Neurosci. 2018; 29(2): 115–123 Frederic Van der Cruyssen* and Constantinus Politis Neurophysiological aspects of the trigeminal sensory system: an update https://doi.org/10.1515/revneuro-2017-0044 Keywords: infraorbital; mandibular; neurophysiology; Received June 21, 2017; accepted July 20, 2017; previously published ophthalmic nerve; oral somatosensory functioning; online November 8, 2017 trigeminal sensory system. Abstract: The trigeminal system is one of the most complex cranial nerve systems of the human body. Research on it has vastly grown in recent years and concentrated more and more on molecular mechanisms and pathophysiology, Introduction but thorough reviews on this topic are lacking, certainly Knowledge about physiological aspects of the trigeminal on the normal physiology of the trigeminal sensory system. system today is largely based on animal models (Akerman Here we review the current literature on neurophysiology and Goadsby, 2015; Herta et al., 2017), cadaver studies of the trigeminal nerve from peripheral receptors up to its (Ezure et al., 2001; Williams et al., 2003) or extrapola- central projections toward the somatosensory cortex. We tions from peripheral nerve functioning. Human studies focus on the most recent scientific discoveries and describe are frequently limited to pathophysiology and lack proper historical relevant research to substantiate further. One study designs (Tanaka and Zhao, 2016; Goadsby et al., chapter on new insights of the pathophysiology of pain 2017). Neurophysiological research in this area is difficult at the level of the trigeminal system is added. A database due to the invasive character of most neurophysiological search of Medline, Embase and Cochrane was conducted tests, the small caliber of fibers, high density of receptors, with the search terms ‘animal study’, ‘neurophysiology’, cross-connections between different cranial nerves, dif- ‘trigeminal’, ‘oral’ and ‘sensory’. -
The Articulatory System Chapter 6 Speech Science/ COMD 6305 UTD/ Callier Center William F. Katz, Ph.D
The articulatory system Chapter 6 Speech Science/ COMD 6305 UTD/ Callier Center William F. Katz, Ph.D. STRUCTURE/FUNCTION VOCAL TRACT CLASSIFICATION OF CONSONANTS AND VOWELS MORE ON RESONANCE ACOUSTIC ANALYSIS/ SPECTROGRAMS SUPRSEGMENTALS, COARTICULATION 1 Midsagittal dissection From Kent, 1997 2 Oral Cavity 3 Oral Structures – continued • Moistened by saliva • Lined by mucosa • Saliva affected by meds 4 Tonsils • PALATINE* (laterally – seen in oral periph • LINGUAL (inf.- root of tongue) • ADENOIDS (sup.) [= pharyngeal] • Palatine, lingual tonsils are larger in children • *removed in tonsillectomy 5 Adenoid Facies • Enlargement from infection may cause problems (adenoid facies) • Can cause problems with nasal sounds or voicing • Adenoidectomy; also tonsillectomy (for palatine tonsils) 6 Adenoid faces (example) 7 Oral structures - frenulum Important component of oral periphery exam Lingual frenomy – for ankyloglossia “tongue-tie” Some doctors will snip for infants, but often will loosen by itself 8 Hard Palate Much variability in palate shape and height Very high vault 9 Teeth 10 Dentition - details Primary (deciduous, milk teeth) Secondary (permanent) n=20: n=32: ◦ 2 incisor ◦ 4 incisor ◦ 1 canine ◦ 2 canine ◦ 2 molar ◦ 4 premolar (bicuspid) Just for “fun” – baby ◦ 6 molar teeth pushing in! NOTE: x 2 for upper and lower 11 Types of malocclusion • Angle’s classification: • I, II, III • Also, individual teeth can be misaligned (e.g. labioversion) Also “Neutrocclusion/ distocclusion/mesiocclusion” 12 Dental Occlusion –continued Other terminology 13 Mandible Action • Primary movements are elevation and depression • Also…. protrusion/retraction • Lateral grinding motion 14 Muscles of Jaw Elevation Like alligators, we are much stronger at jaw elevation (closing to head) than depression 15 Jaw Muscles ELEVATORS DEPRESSORS •Temporalis ✓ •Mylohyoid ✓ •Masseter ✓ •Geniohyoid✓ •Internal (medial) Pterygoid ✓ •Anterior belly of the digastric (- Kent) •Masseter and IP part of “mandibular sling” •External (lateral) pterygoid(?)-- also protrudes and rocks side to side. -

The Clinical Treatment and Outcome of Cerebellopontine Angle
www.nature.com/scientificreports OPEN The clinical treatment and outcome of cerebellopontine angle medulloblastoma: a retrospective study of 15 cases Tao Wu 1,4, Pei-ran Qu3,4, Shun Zhang2, Shi-wei Li1, Jing Zhang1, Bo Wang2, Pinan Liu 1,2, Chun-de Li1,2 & Fu Zhao 1,2 ✉ Medulloblastoma (MB) is the most common malignant pediatric brain tumor arising in the cerebellum or the 4th ventricle. Cerebellopontine angle (CPA) MBs are extremely rare tumors, with few cases previously described. In this study, we sought to describe the clinical characteristics, molecular features and outcomes of CPA MB. We retrospectively reviewed a total of 968 patients who had a histopathological diagnosis of MB at the Beijing Neurosurgical Institute between 2002 and 2016. The demographic characteristics, clinical manifestations and radiological features were retrospectively analyzed. Molecular subgroup was evaluated by the expression profling array or immunohistochemistry. Overall survival (OS) and progression-free survival (PFS) were calculated using Kaplan-Meier analysis. In this study, 15 patients (12 adults and 3 children) with a mean age at diagnosis of 25.1 years (range 4–45 years) were included. CPA MBs represented 1.5% of the total cases of MB (15/968). Two molecular subgroups were identifed in CPA MBs: 5 WNT-MBs (33%) and 10 SHH-MBs (67%). CPA WNT-MBs had the extracerebellar growth with the involvement of brainstem (P = 0.002), whereas CPA SHH-MBs predominantly located within the cerebellar hemispheres (P = 0.004). The 5-year OS and PFS rates for CPA MB were 80.0% ± 10.3% and 66.7% ± 12.2%, respectively. -

DR. Sanaa Alshaarawy
By DR. Sanaa Alshaarawy 1 By the end of the lecture, students will be able to : Distinguish the internal structure of the components of the brain stem in different levels and the specific criteria of each level. 1. Medulla oblongata (closed, mid and open medulla) 2. Pons (caudal, mid “Trigeminal level” and rostral). 3. Mid brain ( superior and inferior colliculi). Describe the Reticular formation (structure, function and pathway) being an important content of the brain stem. 2 1. Traversed by the Central Canal. Motor Decussation*. Spinal Nucleus of Trigeminal (Trigeminal sensory nucleus)* : ➢ It is a larger sensory T.S of Caudal part of M.O. nucleus. ➢ It is the brain stem continuation of the Substantia Gelatinosa of spinal cord 3 The Nucleus Extends : Through the whole length of the brain stem and upper segments of spinal cord. It lies in all levels of M.O, medial to the spinal tract of the trigeminal. It receives pain and temperature from face, forehead. Its tract present in all levels of M.O. is formed of descending fibers that terminate in the trigeminal nucleus. 4 It is Motor Decussation. Formed by pyramidal fibers, (75-90%) cross to the opposite side They descend in the Decuss- = crossing lateral white column of the spinal cord as the lateral corticospinal tract. The uncrossed fibers form the ventral corticospinal tract. 5 Traversed by Central Canal. Larger size Gracile & Cuneate nuclei, concerned with proprioceptive deep sensations of the body. Axons of Gracile & Cuneate nuclei form the internal arcuate fibers; decussating forming Sensory Decussation. Pyramids are prominent ventrally. 6 Formed by the crossed internal arcuate fibers Medial Leminiscus: Composed of the ascending internal arcuate fibers after their crossing. -

The Mandibular Nerve - Vc Or VIII by Prof
The Mandibular Nerve - Vc or VIII by Prof. Dr. Imran Qureshi The Mandibular nerve is the third and largest division of the trigeminal nerve. It is a mixed nerve. Its sensory root emerges from the posterior region of the semilunar ganglion and is joined by the motor root of the trigeminal nerve. These two nerve bundles leave the cranial cavity through the foramen ovale and unite immediately to form the trunk of the mixed mandibular nerve that passes into the infratemporal fossa. Here, it runs anterior to the middle meningeal artery and is sandwiched between the superior head of the lateral pterygoid and tensor veli palatini muscles. After a short course during which a meningeal branch to the dura mater, and the nerve to part of the medial pterygoid muscle (and the tensor tympani and tensor veli palatini muscles) are given off, the mandibular trunk divides into a smaller anterior and a larger posterior division. The anterior division receives most of the fibres from the motor root and distributes them to the other muscles of mastication i.e. the lateral pterygoid, medial pterygoid, temporalis and masseter muscles. The nerve to masseter and two deep temporal nerves (anterior and posterior) pass laterally above the medial pterygoid. The nerve to the masseter continues outward through the mandibular notch, while the deep temporal nerves turn upward deep to temporalis for its supply. The sensory fibres that it receives are distributed as the buccal nerve. The 1 | P a g e buccal nerve passes between the medial and lateral pterygoids and passes downward and forward to emerge from under cover of the masseter with the buccal artery.