Facial Nerve Disorders Cn7 (1)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharnygeal Arch Set - Motor USMLE, Limited Edition > Neuroscience > Neuroscience
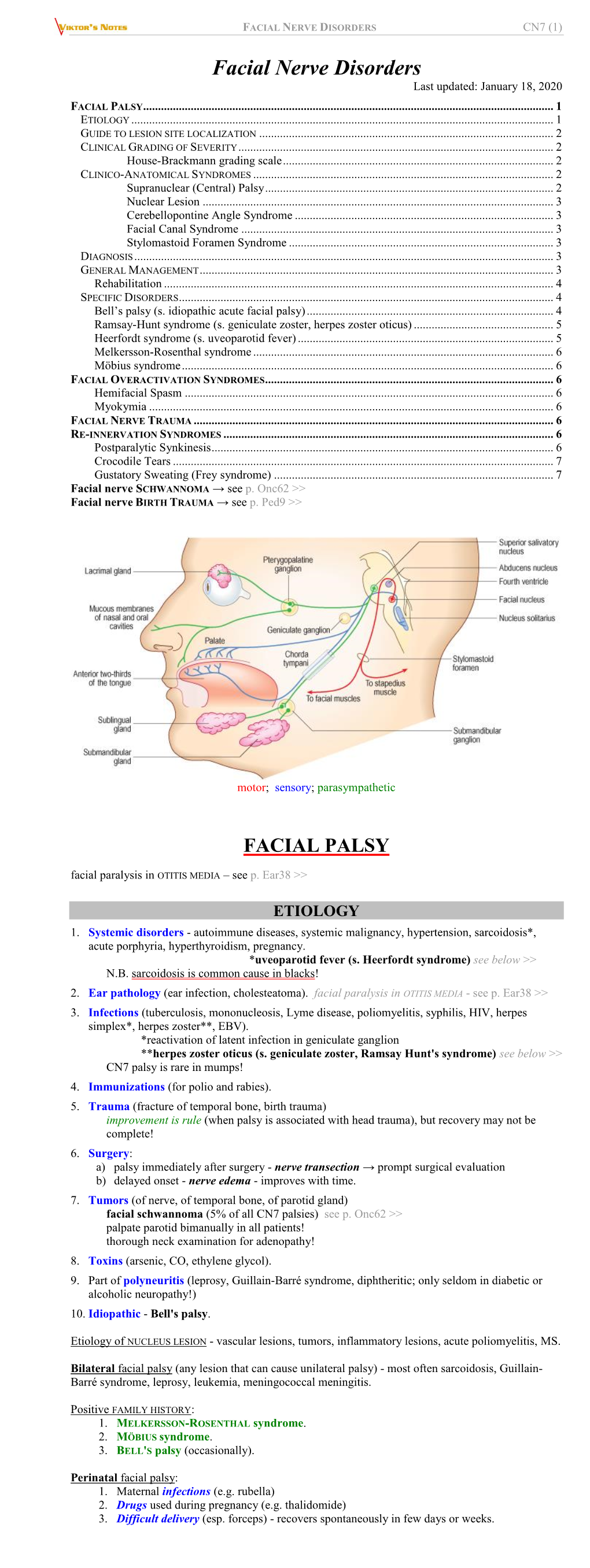
CNs 5, 7, 9, 10 - Pharnygeal Arch Set - Motor USMLE, Limited Edition > Neuroscience > Neuroscience PHARYNGEAL ARCH SET, CNS 5, 7, 9, 10 • They are derived from the pharyngeal (aka branchial) arches • They have special motor and autonomic motor functions CRANIAL NERVES EXIT FROM THE BRAINSTEM CN 5, the trigeminal nerve exits the mid/lower pons.* CN 7, the facial nerve exits the pontomedullary junction.* CN 9, the glossopharyngeal nerve exits the lateral medulla.* CN 10, the vagus nerve exits the lateral medulla.* CRANIAL NERVE NUCLEI AT BRAINSTEM LEVELS Midbrain • The motor trigeminal nucleus of CN 5. Nerve Path: • The motor division of the trigeminal nerve passes laterally to enter cerebellopontine angle cistern. Pons • The facial nucleus of CN 7. • The superior salivatory nucleus of CN 7. Nerve Path: • CN 7 sweeps over the abducens nucleus as it exits the brainstem laterally in an internal genu, which generates a small bump in the floor of the fourth ventricle: the facial colliculus • Fibers emanate from the superior salivatory nucleus, as well. Medulla • The dorsal motor nucleus of the vagus, CN 10 • The inferior salivatory nucleus, CN 9 1 / 3 • The nucleus ambiguus, CNs 9 and 10. Nerve Paths: • CNs 9 and 10 exit the medulla laterally through the post-olivary sulcus to enter the cerebellomedullary cistern. THE TRIGEMINAL NERVE, CN 5  • The motor division of the trigeminal nerve innervates the muscles of mastication • It passes ventrolaterally through the cerebellopontine angle cistern and exits through foramen ovale as part of the mandibular division (CN 5[3]). Clinical Correlation - Trigeminal Neuropathy THE FACIAL NERVE, CN 7  • The facial nucleus innervates the muscles of facial expression • It spans from the lower pons to the pontomedullary junction. -

The Corneomandibular Reflex1
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.34.3.236 on 1 June 1971. Downloaded from J. Neurol. Neurosurg. Psychiat., 1971, 34, 236-242 The corneomandibular reflex1 ROBERT M. GORDON2 AND MORRIS B. BENDER From the Department of Neurology, the Mount Sinai Hospital, New York, U.S.A. SUMMARY Seven patients are presented in whom a prominent corneomandibular reflex was observed. These patients all had severe cerebral and/or brain-stem disease with altered states of consciousness. Two additional patients with less prominent and inconstant corneomandibular reflexes were seen; one had bulbar amyotrophic lateral sclerosis and one had no evidence of brain disease. The corneomandibular reflex, when found to be prominent, reflects an exaggeration of the normal. Therefore one may consider the corneomandibular hyper-reflexia as possibly due to disease of the corticobulbar system. The corneomandibular reflex consists of an involun- weak bilateral response on a few occasions. This tary contralateral deviation and protrusion of the was a woman with bulbar and spinal amyotrophic lower jaw during corneal stimulation. It is not a lateral sclerosis. The other seven patients hadProtected by copyright. common phenomenon and has been rediscovered prominent and consistently elicited corneo- several times since its initial description by Von mandibular reflexes. The clinical features common to Solder in 1902. It is found mostly in patients with these patients were (1) the presence of bilateral brain-stem or bilateral cerebral lesions who are in corneomandibular reflexes, in some cases more coma or semicomatose. prominent on one side; (2) a depressed state of con- There have been differing opinions as to the sciousness, usually coma; and (3) the presence of incidence, anatomical basis, and clinical significance severe neurological abnormalities, usually motor, of this reflex. -

Heerfordt's Syndrome, Or Uveoparotid Fever
T h e new england journal o f medicine images in clinical medicine Lindsey R. Baden, M.D., Editor Heerfordt’s Syndrome, or Uveoparotid Fever A B C D Anisha Dua, M.D. 32-year-old woman presented with a 6-week history of swelling of both parotid glands, dry eyes, and dry mouth. She reported having difficulty West Penn Allegheny Health System Pittsburgh, PA A moving the right side of her face, and she felt tingling in the right side of her tongue. Physical examination revealed enlargement of both parotid glands, which were Augustine Manadan, M.D. firm and nontender, submandibular enlargement, and enlargement of lacrimal glands (Panel A). She did not have a fever, and there was no uveitis. She could not completely Rush University Medical Center Chicago, IL close her right eye, was unable to purse her lips, and was unable to smile on the right side of her face. Facial sensation was symmetric and intact. The results of a test for Lyme disease and the human immunodeficiency virus were negative. Serum IgG4 levels were normal. A chest radiograph suggested bilateral hilar adenopathy and possible right para tracheal adenopathy but was otherwise unremarkable. Computed tomography of the head revealed enlargement and increased uniform contrast enhancement of the both parotid glands (Panel B). A biopsy specimen from the right parotid gland revealed scattered granulomas with focal central necrosis. Stains for acid-fast bacilli and fungi were negative (Panel C, hematoxylin and eosin). She was given a diagnosis of Heer- fordt’s syndrome, a rare form of sarcoidosis in which the compression of the facial nerve results in palsy. -

The Clinical Treatment and Outcome of Cerebellopontine Angle
www.nature.com/scientificreports OPEN The clinical treatment and outcome of cerebellopontine angle medulloblastoma: a retrospective study of 15 cases Tao Wu 1,4, Pei-ran Qu3,4, Shun Zhang2, Shi-wei Li1, Jing Zhang1, Bo Wang2, Pinan Liu 1,2, Chun-de Li1,2 & Fu Zhao 1,2 ✉ Medulloblastoma (MB) is the most common malignant pediatric brain tumor arising in the cerebellum or the 4th ventricle. Cerebellopontine angle (CPA) MBs are extremely rare tumors, with few cases previously described. In this study, we sought to describe the clinical characteristics, molecular features and outcomes of CPA MB. We retrospectively reviewed a total of 968 patients who had a histopathological diagnosis of MB at the Beijing Neurosurgical Institute between 2002 and 2016. The demographic characteristics, clinical manifestations and radiological features were retrospectively analyzed. Molecular subgroup was evaluated by the expression profling array or immunohistochemistry. Overall survival (OS) and progression-free survival (PFS) were calculated using Kaplan-Meier analysis. In this study, 15 patients (12 adults and 3 children) with a mean age at diagnosis of 25.1 years (range 4–45 years) were included. CPA MBs represented 1.5% of the total cases of MB (15/968). Two molecular subgroups were identifed in CPA MBs: 5 WNT-MBs (33%) and 10 SHH-MBs (67%). CPA WNT-MBs had the extracerebellar growth with the involvement of brainstem (P = 0.002), whereas CPA SHH-MBs predominantly located within the cerebellar hemispheres (P = 0.004). The 5-year OS and PFS rates for CPA MB were 80.0% ± 10.3% and 66.7% ± 12.2%, respectively. -
Validation of a Treatment-Based Classification System for Individuals
Validation of a Treatment-Based Classification System for Individuals With Facial Neuromotor Disorders Downloaded from https://academic.oup.com/ptj/article/78/7/678/2633301 by guest on 27 September 2021 Background and Purpose. A method for linking treatments to signs and symptoms of facial neuromotor disorders is needed. We describe the construct validation of a treatment-based classification system for facial neuromotor disorders. Subjects and Methods. Based on physical signs and symptoms, 148 patients (mean age=48.9 years, SD= 16.1, range = 20 -93) were assigned to treatment-based categories. The pattern of impairment and disability was compared with clinical expectations. Results. The distribution of impairment and disability scores demonstrated the expected signs and symptoms of the treatment-based categories. Confirmatory principal-components factor analysis indicated 4 factors, corresponding to the treatment-based categories; the factor loadings confirmed the presence of the key sign or symptom characteristic of the categories. Conclusion and Discus- sion. Classifying facial neuromotor disorders into treatment-based categories appears to be a valid method for categorizing patients with specific impairments or disabilities and may be useful in linking treatments to outcomes. [VanSwearingen JM, Brach JS. Validation of a treatment-based classification system for individuals with facial neuro- motor disorders. Phys Ther. 1998;78:678-689.1 Key Words: Classification, Facial paralysis, Rehabilitation. Jessie M VanSwearingen I Jennifer -

Lyme Disease Diagnostic Support Tool
1 / 11 For further details, click on the DIAGNOSTIC SUPPORT TOOL underlined words. Localized and disseminated stages of Lyme disease This diagnostic support tool is intended mainly for primary care clinicians. It is provided for information purposes only and should not replace the judgement of the clinician who performs the activities reserved under a statute or regulation. The recommendations in this tool were developed using a systematic process and are supported by the scientific literature and the knowledge and experience of Québec health professionals, experts and patients. For further details, go to the “Publications” section of INESSS’s website inesss.qc.ca. This tool does not deal with other tick-borne infections or with the much-debated form of Lyme disease, which is sometimes referred to as the chronic form. WHAT IS LYME DISEASE ? WHAT ARE THE DIFFERENT STAGES OF THE DISEASE? GENERAL INFORMATION • Lyme disease is an infectious disease caused by bacterial Localized stage (sometimes called the early stage): Beginning Patient with a tick genospecies of Borrelia burgdorferi, which are transmitted of the infection before dissemination of the bacteria in the • If tick is attached, refer to the procedure for removing it. to humans by black-legged ticks that are carriers. bloodstream. • Refer to the tick surveillance procedure. • Main manifestation observed: • It is a notifiable disease (MADO) • Consult the decision support tool or the Québec’s national and is on the increase in Québec. Not always present or noticed. medical protocol on post-exposure prophylaxis. • It can affect several anatomical systems at the same time. If present, usually appears • Identifying the tick and obtaining proof that it carries of Lym 3 to 30 days after infection or e d B. -

Oculomotor Nerve Palsy Associated with Rupture of Middle Cerebral Artery Aneurysm
online © ML Comm www.jkns.or.kr 10.3340/jkns.2009.45.4.240 Print ISSN 2005-3711 On-line ISSN 1598-7876 J Korean Neurosurg Soc 45 : 240-242, 2009 Copyright © 2009 The Korean Neurosurgical Society Case Report Oculomotor Nerve Palsy Associated with Rupture of Middle Cerebral Artery Aneurysm Sung Chul Kim, M.D.,1 Joonho Chung, M.D.,1 Yong Cheol Lim, M.D.,1 Yong Sam Shin, M.D.2 Department of Neurosurgery,1 Ajou University School of Medicine, Suwon, Korea Department of Neurosurgery,2 Kangnam St. Mary’s Hospital, The Catholic University of Korea, Seoul, Korea Oculomotor nerve palsy (ONP) with subarachnoid hemorrhage (SAH) occurs usually when oculomotor nerve is compressed by growing or budding of posterior communicating artery (PcoA) aneurysm. Midbrain injury, increased intracranial pressure (ICP), or uncal herniation may also cause it. We report herein a rare case of ONP associated with SAH which was caused by middle cerebral artery (MCA) bifurcation aneurysm rupture. A 58-year-old woman with clear consciousness suffered from headache and sudden onset of unilateral ONP. Computed tomography showed SAH caused by the rupture of MCA aneurysm. The unilateral ONP was not associated with midbrain injury, increased ICP, or uncal herniation. The patient was treated with coil embolization, and the signs of oculomotor nerve palsy completely resolved after a few days. We suggest that bloody jet flow from the rupture of distant aneurysm other than PcoA aneurysm may also be considered as a cause of sudden unilateral ONP in patients with SAH. KEY WORDS : Oculomotor nerve palsy ˙ Middle cerebral artery aneurysm ˙ Subarachnoid hemorrhage. -

Validation of a New Photogrammetric Technique to Monitor the Treatment
Eye (2013) 27, 860–864 & 2013 Macmillan Publishers Limited All rights reserved 0950-222X/13 www.nature.com/eye 1;2 1 1 CLINICAL STUDY Validation of a new NT Mabvuure , M-J Hallam , V Venables and C Nduka1 photogrammetric technique to monitor the treatment effect of Botulinum toxin in synkinesis Abstract Aims To validate a new photogrammetric Level of evidence 2c. technique for quantifying eye surface area Eye (2013) 27, 860–864; doi:10.1038/eye.2013.91; and using this to quantify the degree of published online 17 May 2013 improvement in symmetry in patients with oral–ocular synkinesis following Botulinum Keywords: synkinesis; botulinum toxin; facial toxin injection. palsy; photogrammetric Study design Feasibility study and retrospective outcomes analysis Introduction Methods Ten patients’ photographs were chosen from a photographic database. Patients with facial nerve injuries are frequently Their eye surface areas were measured afflicted by synkinesis, a movement disorder 1Queen Victoria Hospital independently by two raters using a graphics principally attributed to aberrant nerve NHS Foundation Trust, East tablet. One rater repeated the procedure after regeneration.1 The incidence of synkinesis in Grinstead, UK 15 days. Bland–Altman plots were computed, patients recovering from facial paralysis is ascertaining inter-rater and intra-rater between 15–50% depending on the series.2,3 2 Brighton and Sussex variability. The eye surface areas of 19 Synkinesis specifically refers to the involuntary Medical School, Brighton, UK patients were then derived from photographs contraction of a muscle or muscle group, in taken before and after Botulinum toxin addition to that required for a desired Correspondence: injections. -

Ocular Neuromyotonia Br J Ophthalmol: First Published As 10.1136/Bjo.80.4.350 on 1 April 1996
350 British Journal of Ophthalmology 1996; 80: 350-355 Ocular neuromyotonia Br J Ophthalmol: first published as 10.1136/bjo.80.4.350 on 1 April 1996. Downloaded from Eric Ezra, David Spalton, Michael D Sanders, Elizabeth M Graham, Gordon T Plant Abstract revealed a neurogenic pattern and they con- Aims/Background-Ocular neuromyo- cluded that neuromyotonic activity resulted tonia is characterised by spontaneous from spontaneous electrical activity in unstable spasm of extraocular muscles and has motor nerve membranes, followed by ephatic been described in only 14 patients. Three transmission of electrical activity to adjacent further cases, two with unique features, nerves, causing co-firing of different muscles are described, and the underlying mech- supplied by the third nerve. This hypothesis anism reviewed in the light of recent was supported by the fact that both patients experimental evidence implicating extra- responded and became asymptomatic after cellular potassium concentration in treatment with carbamazepine, an anticonvul- causing spontaneous firing in normal and sant. The term 'ocular neuromyotonia' was demyelinated axons. used to describe the syndrome. Further reports Methods-Two patients had third nerve in the literature have been sparse3-6 as sum- neuromyotonia, one due to compression marised in Table 1. by an internal carotid artery aneurysm, The condition is distinct from superior which has not been reported previously, oblique myokymia, which is characterised by while the other followed irradiation of a oscillopsia and -

Lipoma of the Midbrain
LIPOMA OF THE MIDBRAIN POST-MORTEM FINDING IN A PATIENT WITH BREAST CANCER VERÔNICA MAIA GOUVEA * — MYRIAM DUMAS HAHN ** — LEILA CHIMELLI ** SUMMARY — Intracranial lipomas are rare, usually do not have clinical expression and are located mare frequently in the corpus callosum. Other locations include the spinal cord, midbrain tectum, superior vermis, tuber cinereum, infundibulum and more rarely cerebello pontine angle, hypothalamus, superior medullary velum and insula. We report the case of a lipoma of the left inferior colliculus which was a post-mortem finding in a woman who died of breast cancer. Although there are reports of intracranial lipomas in patients with malignant tumors there is no explanation for the co-existence of the two tumors. The present tumor also includes a segment of a nerve which is not uncommon, but a less common finding was the presence of nests of Schwann cells within it, shown by immunohistochemistry. Lipoma do mesencéfalo: achado de necrópsia, em paciente com câncer da mama. RESUMO — Lipomas intracranianos são raros, em geral sem expressão clínica, localizados mais freqüentemente no corpo caloso. Outras localizações incluem medula espinhal, teto mesencefálico, vermis superior, tuber cinereum, infundibulum e mais raramente o ângulo ponto-cerebelar, hipotálamo, véu medular superior e insula. Relatamos o achado de necrópsia de um lipoma do colículo inferior esquerdo em uma mulher com câncer de mama. Embora haja relatos de lipomas intracranianos em pacientes com tumores malignos não há explicação para a co-existência dos dois tumores. O presente tumor também inclui o segmento de um nervo, o que não é incomum, mas um achado menos comum foi a presença de ninhos de células de Schwann no tumor, mostradas por imuno-histoquímica. -

Current Considerations in the Management of Facial Nerve Palsy
REVIEW CURRENT OPINION Current considerations in the management of facial nerve palsy Charles Kim and Gary J. Lelli Jr Purpose of review Facial nerve palsy is a potentially devastating condition that can arise from many different causes. Appropriate management is complicated by the wide spectrum of clinical presentation and disease severity that characterizes this condition. As such, recent studies have focused on augmenting our understanding of the underlying anatomy and pathophysiology of facial nerve palsy, while also exploring different treatment options. Recent findings There have been a multitude of radiologic investigations that have delineated anatomical considerations pertinent to facial neuropathy, whereas various grading schemes and software programs have been developed to facilitate the clinical assessment of patients. Furthermore, a wide variety of medical and surgical treatment options have been proposed – whereas some are variants of previously described methods, others represent novel approaches. Summary Appropriate management of facial nerve palsy is dependent on a multitude of factors and must be tailored to patients on an individual basis. The studies summarized in this article highlight the recent advancements geared toward refining the assessment and treatment of patients with facial neuropathy. Keywords Bell’s palsy, exposure keratopathy, facial nerve palsy, facial synkinesis INTRODUCTION Ramsay Hunt syndrome, herpes simplex virus, The facial nerve (cranial nerve VII) is intimately human immunodeficiency virus, Lyme -

Anatomy of the Brainstem
Anatomy of the Brainstem Neuroanatomy block-Anatomy-Lecture 5 Editing file Objectives At the end of the lecture, students should be able to: 01 List the components of brain stem. 02 Describe the site of brain stem 03 Describe the relations between components of brain stem & their relations to cerebellum. 04 Describe the external features of both ventral & dorsal surfaces of brain stem Color guide 05 List cranial nerves emerging from brain stem 06 Describe the site of emergence of each cranial nerve ● Only in boys slides in Green ● Only in girls slides in Purple ● important in Red ● Notes in Grey Development of Brain Brain stem ● The brain develops from the cranial part of neural tube. ● The brainstem is the region of the brain that connects the ● The cranial part is divided into 3 parts: cerebrum with the spinal cord. ● Site: It lies on the basilar part of occipital bone (clivus). - Subdivided into: ● Parts from above downwards : 1. Telencephalon: (cavities: 2 lateral ventricles) 1. Midbrain Two cerebral hemispheres. Forebrain 2. Pons 2. Diencephalon: (cavity: 3rd ventricle) 3. Medulla oblongata thalamus, hypothalamus, epithalamus & subthalamus ● Connection with cerebellum: Each part of the brain stem is connected to the Midbrain - (cavity: cerebral aqueduct) cerebellum by cerebellar peduncles (superior, middle & inferior). - (cavity: 4th ventricle) - Subdivided into: Hindbrain 1. Pons 2. Cerebellum 3. Medulla oblongata 3 Sagittal section of Brain 4 Functions of the Brain Stem Pathway of tracts between cerebral cortex & spinal cord (ascending and descending tracts). 1 Site of origin of nuclei of cranial nerves (from 3rd to 12th). 2 Site of emergence of cranial nerves (from 3rd to 12th).