Connective Tissuetissue
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Basic Histology and Connective Tissue Chapter 5
Basic Histology and Connective Tissue Chapter 5 • Histology, the Study of Tissues • Tissue Types • Connective Tissues Histology is the Study of Tissues • 200 different types of cells in the human body. • A Tissue consist of two or more types of cells that function together. • Four basic types of tissues: – epithelial tissue – connective tissue – muscular tissue – nervous tissue • An Organ is a structure with discrete boundaries that is composed of 2 or more tissue types. • Example: skin is an organ composed of epidermal tissue and dermal tissue. Distinguishing Features of Tissue Types • Types of cells (shapes and functions) • Arrangement of cells • Characteristics of the Extracellular Matrix: – proportion of water – types of fibrous proteins – composition of the ground substance • ground substance is the gelatinous material between cells in addition to the water and fibrous proteins • ground substance consistency may be liquid (plasma), rubbery (cartilage), stony (bone), elastic (tendon) • Amount of space occupied by cells versus extracellular matrix distinguishes connective tissue from other tissues – cells of connective tissues are widely separated by a large amount of extracellular matrix – very little extracellular matrix between the cells of epithelia, nerve, and muscle tissue Embryonic Tissues • An embryo begins as a single cell that divides into many cells that eventually forms 3 Primary Layers: – ectoderm (outer layer) • forms epidermis and nervous system – endoderm (inner layer) • forms digestive glands and the mucous membrane lining digestive tract and respiratory system – mesoderm (middle layer) • Forms muscle, bone, blood and other organs. Histotechnology • Preparation of specimens for histology: – preserve tissue in a fixative to prevent decay (formalin) – dehydrate in solvents like alcohol and xylene – embed in wax or plastic – slice into very thin sections only 1 or 2 cells thick – float slices on water and mount on slides and then add color with stains • Sectioning an organ or tissue reduces a 3-dimensional structure to a 2- dimensional slice. -

Reactive Stroma in Human Prostate Cancer: Induction of Myofibroblast Phenotype and Extracellular Matrix Remodeling1
2912 Vol. 8, 2912–2923, September 2002 Clinical Cancer Research Reactive Stroma in Human Prostate Cancer: Induction of Myofibroblast Phenotype and Extracellular Matrix Remodeling1 Jennifer A. Tuxhorn, Gustavo E. Ayala, Conclusions: The stromal microenvironment in human Megan J. Smith, Vincent C. Smith, prostate cancer is altered compared with normal stroma and Truong D. Dang, and David R. Rowley2 exhibits features of a wound repair stroma. Reactive stroma is composed of myofibroblasts and fibroblasts stimulated to Departments of Molecular and Cellular Biology [J. A. T., T. D. D., express extracellular matrix components. Reactive stroma D. R. R.] and Pathology [G. E. A., M. J. S., V. C. S.] Baylor College of Medicine, Houston, Texas 77030 appears to be initiated during PIN and evolve with cancer progression to effectively displace the normal fibromuscular stroma. These studies and others suggest that TGF-1isa ABSTRACT candidate regulator of reactive stroma during prostate can- Purpose: Generation of a reactive stroma environment cer progression. occurs in many human cancers and is likely to promote tumorigenesis. However, reactive stroma in human prostate INTRODUCTION cancer has not been defined. We examined stromal cell Activation of the host stromal microenvironment is pre- phenotype and expression of extracellular matrix compo- dicted to be a critical step in adenocarcinoma growth and nents in an effort to define the reactive stroma environ- progression (1–5). Several human cancers have been shown to ment and to determine its ontogeny during prostate cancer induce a stromal reaction or desmoplasia as a component of progression. carcinoma progression. However, the specific mechanisms of Experimental Design: Normal prostate, prostatic intra- stromal cell activation are not known, and the extent to which epithelial neoplasia (PIN), and prostate cancer were exam- stroma regulates the biology of tumorigenesis is not fully un- ined by immunohistochemistry. -

Profiling Microdissected Epithelium and Stroma to Model Genomic Signatures for Cervical Carcinogenesis Accommodating for Covariates
Research Article Profiling Microdissected Epithelium and Stroma to Model Genomic Signatures for Cervical Carcinogenesis Accommodating for Covariates David Gius,1 Margo C. Funk,2 Eric Y. Chuang,1 Sheng Feng,3 Phyllis C. Huettner,4 Loan Nguyen,2 C. Matthew Bradbury,1 Mark Mishra,1 Shuping Gao,1 Barbara M. Buttin,2 David E. Cohn,2 Matthew A. Powell,2 Neil S. Horowitz,2 Bradford P. Whitcomb,2 and JanetS. Rader 2 1Radiation Oncology Branch, Center for Cancer Research, National Cancer Institute, NIH, Bethesda, Maryland and 2Division of Gynecologic Oncology, Department of Obstetrics and Gynecology; 3Division of Biostatistics; and 4Lauren V. Ackerman Laboratory of Surgical Pathology, Washington University School of Medicine, St. Louis, Missouri Abstract (CIN 1–3) and finally to squamous cell carcinoma antigen (SCCA) This study is the first comprehensive, integrated approach to have been well characterized. Histologically, CIN 1 consists of examine grade-specific changes in gene expression along the immature basal-type cells involving the lower third of the entire neoplastic spectrum of cervical intraepithelial neoplasia epithelium. In CIN 2, these immature basal-type cells involve more (CIN) in the process of cervical carcinogenesis. This was than the lower third, whereas CIN 3 involves the full thickness of the accomplished by identifying gene expression signatures of epithelium. In addition, higher CIN grades exhibit nuclear crowding, disease progression using cDNA microarrays to analyze RNA pleomorphism, loss of cell polarity, and increased mitotic activity from laser-captured microdissected epithelium and underlying (1). These transitions seemto be well conserved and, as such, stroma from normal cervix, graded CINs, cancer, and patient- provide an intriguing systemto use genomicsto identify the early matched normal cervical tissues. -

Normal Gross and Histologic Features of the Gastrointestinal Tract
NORMAL GROSS AND HISTOLOGIC 1 FEATURES OF THE GASTROINTESTINAL TRACT THE NORMAL ESOPHAGUS left gastric, left phrenic, and left hepatic accessory arteries. Veins in the proximal and mid esopha- Anatomy gus drain into the systemic circulation, whereas Gross Anatomy. The adult esophagus is a the short gastric and left gastric veins of the muscular tube measuring approximately 25 cm portal system drain the distal esophagus. Linear and extending from the lower border of the cri- arrays of large caliber veins are unique to the distal coid cartilage to the gastroesophageal junction. esophagus and can be a helpful clue to the site of It lies posterior to the trachea and left atrium a biopsy when extensive cardiac-type mucosa is in the mediastinum but deviates slightly to the present near the gastroesophageal junction (4). left before descending to the diaphragm, where Lymphatic vessels are present in all layers of the it traverses the hiatus and enters the abdomen. esophagus. They drain to paratracheal and deep The subdiaphragmatic esophagus lies against cervical lymph nodes in the cervical esophagus, the posterior surface of the left hepatic lobe (1). bronchial and posterior mediastinal lymph nodes The International Classification of Diseases in the thoracic esophagus, and left gastric lymph and the American Joint Commission on Cancer nodes in the abdominal esophagus. divide the esophagus into upper, middle, and lower thirds, whereas endoscopists measure distance to points in the esophagus relative to the incisors (2). The esophagus begins 15 cm from the incisors and extends 40 cm from the incisors in the average adult (3). The upper and lower esophageal sphincters represent areas of increased resting tone but lack anatomic landmarks; they are located 15 to 18 cm from the incisors and slightly proximal to the gastroesophageal junction, respectively. -

The Plantar Aponeurosis in Fetuses and Adults: an Aponeurosis Or Fascia?
Int. J. Morphol., 35(2):684-690, 2017. The Plantar Aponeurosis in Fetuses and Adults: An Aponeurosis or Fascia? La Aponeurosis Plantar en Fetos y Adultos: ¿Aponeurosis o Fascia? A. Kalicharan; P. Pillay; C.O. Rennie; B.Z. De Gama & K.S. Satyapal KALICHARAN, A.; PILLAY, P.; RENNIE, C.O.; DE GAMA, B. Z. & SATYAPAL, K. S. The plantar aponeurosis in fetuses and adults: An aponeurosis or fascia? Int. J. Morphol., 35(2):684-690, 2017. SUMMARY: The plantar aponeurosis (PA), which is a thickened layer of deep fascia located on the plantar surface of the foot, is comprised of three parts. There are differing opinions on its nomenclature since various authors use the terms PA and plantar fascia (PF) interchangeably. In addition, the variable classifications of its parts has led to confusion. In order to assess the nature of the PA, this study documented its morphology. Furthermore, a pilot histological analysis was conducted to examine whether the structure is an aponeurosis or fascia. This study comprised of a morphological analysis of the three parts of the PA by micro- and macro-dissection of 50 fetal and 50 adult cadaveric feet, respectively (total n=100). Furthermore, a pilot histological analysis was conducted on five fetuses (n=10) and five adults (n=10) (total n=20). In each foot, the histological analysis was conducted on the three parts of the plantar aponeurosis, i.e. the central, lateral, and medial at their calcaneal origin (total n=60). Fetuses: i) Morphology: In 66 % (33/50) of the specimens, the standard anatomical pattern was observed, viz. -

Colposcopy of the Uterine Cervix
THE CERVIX: Colposcopy of the Uterine Cervix • I. Introduction • V. Invasive Cancer of the Cervix • II. Anatomy of the Uterine Cervix • VI. Colposcopy • III. Histology of the Normal Cervix • VII: Cervical Cancer Screening and Colposcopy During Pregnancy • IV. Premalignant Lesions of the Cervix The material that follows was developed by the 2002-04 ASCCP Section on the Cervix for use by physicians and healthcare providers. Special thanks to Section members: Edward J. Mayeaux, Jr, MD, Co-Chair Claudia Werner, MD, Co-Chair Raheela Ashfaq, MD Deborah Bartholomew, MD Lisa Flowers, MD Francisco Garcia, MD, MPH Luis Padilla, MD Diane Solomon, MD Dennis O'Connor, MD Please use this material freely. This material is an educational resource and as such does not define a standard of care, nor is intended to dictate an exclusive course of treatment or procedure to be followed. It presents methods and techniques of clinical practice that are acceptable and used by recognized authorities, for consideration by licensed physicians and healthcare providers to incorporate into their practice. Variations of practice, taking into account the needs of the individual patient, resources, and limitation unique to the institution or type of practice, may be appropriate. I. AN INTRODUCTION TO THE NORMAL CERVIX, NEOPLASIA, AND COLPOSCOPY The uterine cervix presents a unique opportunity to clinicians in that it is physically and visually accessible for evaluation. It demonstrates a well-described spectrum of histological and colposcopic findings from health to premalignancy to invasive cancer. Since nearly all cervical neoplasia occurs in the presence of human papillomavirus infection, the cervix provides the best-defined model of virus-mediated carcinogenesis in humans to date. -

Nomina Histologica Veterinaria, First Edition
NOMINA HISTOLOGICA VETERINARIA Submitted by the International Committee on Veterinary Histological Nomenclature (ICVHN) to the World Association of Veterinary Anatomists Published on the website of the World Association of Veterinary Anatomists www.wava-amav.org 2017 CONTENTS Introduction i Principles of term construction in N.H.V. iii Cytologia – Cytology 1 Textus epithelialis – Epithelial tissue 10 Textus connectivus – Connective tissue 13 Sanguis et Lympha – Blood and Lymph 17 Textus muscularis – Muscle tissue 19 Textus nervosus – Nerve tissue 20 Splanchnologia – Viscera 23 Systema digestorium – Digestive system 24 Systema respiratorium – Respiratory system 32 Systema urinarium – Urinary system 35 Organa genitalia masculina – Male genital system 38 Organa genitalia feminina – Female genital system 42 Systema endocrinum – Endocrine system 45 Systema cardiovasculare et lymphaticum [Angiologia] – Cardiovascular and lymphatic system 47 Systema nervosum – Nervous system 52 Receptores sensorii et Organa sensuum – Sensory receptors and Sense organs 58 Integumentum – Integument 64 INTRODUCTION The preparations leading to the publication of the present first edition of the Nomina Histologica Veterinaria has a long history spanning more than 50 years. Under the auspices of the World Association of Veterinary Anatomists (W.A.V.A.), the International Committee on Veterinary Anatomical Nomenclature (I.C.V.A.N.) appointed in Giessen, 1965, a Subcommittee on Histology and Embryology which started a working relation with the Subcommittee on Histology of the former International Anatomical Nomenclature Committee. In Mexico City, 1971, this Subcommittee presented a document entitled Nomina Histologica Veterinaria: A Working Draft as a basis for the continued work of the newly-appointed Subcommittee on Histological Nomenclature. This resulted in the editing of the Nomina Histologica Veterinaria: A Working Draft II (Toulouse, 1974), followed by preparations for publication of a Nomina Histologica Veterinaria. -

Tumor-Associated Stromal Cells As Key Contributors to the Tumor Microenvironment Karen M
Bussard et al. Breast Cancer Research (2016) 18:84 DOI 10.1186/s13058-016-0740-2 REVIEW Open Access Tumor-associated stromal cells as key contributors to the tumor microenvironment Karen M. Bussard1,2, Lysette Mutkus3, Kristina Stumpf3, Candelaria Gomez-Manzano4 and Frank C. Marini1,3* Abstract The tumor microenvironment is a heterogeneous population of cells consisting of the tumor bulk plus supporting cells. It is becoming increasingly evident that these supporting cells are recruited by cancer cells from nearby endogenous host stroma and promote events such as tumor angiogenesis, proliferation, invasion, and metastasis, as well as mediate mechanisms of therapeutic resistance. In addition, recruited stromal cells range in type and include vascular endothelial cells, pericytes, adipocytes, fibroblasts, and bone-marrow mesenchymal stromal cells. During normal wound healing and inflammatory processes, local stromal cells change their phenotype to become that of reactive stroma. Under certain conditions, however, tumor cells can co-opt these reactive stromal cells and further transition them into tumor-associated stromal cells (TASCs). These TASCs express higher levels of proteins, including alpha-smooth muscle actin, fibroblast activating protein, and matrix metalloproteinases, compared with their normal, non-reactive counterparts. TASCs are also known to secrete many pro-tumorigenic factors, including IL-6, IL-8, stromal-derived factor-1 alpha, vascular endothelial growth factor, tenascin-C, and matrix metalloproteinases, among others, which recruit additional tumor and pro-tumorigenic cells to the developing microenvironment. Here, we review the current literature pertaining to the origins of recruited host stroma, contributions toward tumor progression, tumor-associated stromal cells, and mechanisms of crosstalk between endogenous host stroma and tumor cells. -
The 4 Types of Tissues: Connective
The 4 Types of Tissues: connective Connective Tissue General structure of CT cells are dispersed in a matrix matrix = a large amount of extracellular material produced by the CT cells and plays a major role in the functioning matrix component = ground substance often crisscrossed by protein fibers ground substance usually fluid, but it can also be mineralized and solid (bones) CTs = vast variety of forms, but typically 3 characteristic components: cells, large amounts of amorphous ground substance, and protein fibers. Connective Tissue GROUND SUBSTANCE In connective tissue, the ground substance is an amorphous gel-like substance surrounding the cells. In a tissue, cells are surrounded and supported by an extracellular matrix. Ground substance traditionally does not include fibers (collagen and elastic fibers), but does include all the other components of the extracellular matrix . The components of the ground substance vary depending on the tissue. Ground substance is primarily composed of water, glycosaminoglycans (most notably hyaluronan ), proteoglycans, and glycoproteins. Usually it is not visible on slides, because it is lost during the preparation process. Connective Tissue Functions of Connective Tissues Support and connect other tissues Protection (fibrous capsules and bones that protect delicate organs and, of course, the skeletal system). Transport of fluid, nutrients, waste, and chemical messengers is ensured by specialized fluid connective tissues, such as blood and lymph. Adipose cells store surplus energy in the form of fat and contribute to the thermal insulation of the body. Embryonic Connective Tissue All connective tissues derive from the mesodermal layer of the embryo . The first connective tissue to develop in the embryo is mesenchyme , the stem cell line from which all connective tissues are later derived. -
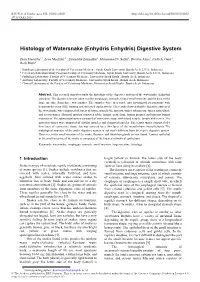
Histology of Watersnake (Enhydris Enhydris) Digestive System
E3S Web of Conferences 151, 01052 (2020) https://doi.org/10.1051/e3sconf/202015101052 st 1 ICVAES 2019 Histology of Watersnake (Enhydris Enhydris) Digestive System Dian Masyitha1,*, Lena Maulidar 2 , Zainuddin Zainuddin1, Muhammad N. Salim3, Dwinna Aliza3, Fadli A. Gani 4 , Rusli Rusli5 1 Histology Laboratory of the Faculty of Veterinary Medicine, Syiah Kuala University, Banda Aceh 23111, Indonesia 2 Veterinary Education Study Program Faculty of Veterinary Medicine, Syiah Kuala University, Banda Aceh 23111, Indonesia 3 Pathology Laboratory, Faculty of Veterinary Medicine, Universitas Syiah Kuala , Banda Aceh, Indonesia 4 Anatomy Laboratory, Faculty of Veterinary Medicine, Universitas Syiah Kuala , Banda Aceh, Indonesia 5 Clinical Laboratory of the Faculty of Veterinary Medicine, Universitas Syiah Kuala , Banda Aceh, Indonesia Abstract. This research aimed to study the histology of the digestive system of the watersnake (Enhydris enhydris). The digestive system taken was the esophagus, stomach, frontal small intestine and the back of the large intestine from three watersnakes. The samples were then made into histological preparations with hematoxylin-eosin (HE) staining and observed exploratively. The results showed that the digestive system of the watersnake was composed of layers of tissue, namely the mucosa, tunica submucosa, tunica muscularis, and serous tunica. Mucosal mucosa consisted of the lamina epithelium, lamina propria, and mucous lamina muscularis. The submucosal tunica consisted of connective tissue with blood vessels, lymph, and nerves. The muscular tunica was composed of circular muscles and elongated muscles. The serous tunica consisted of a thin layer of connective tissue that was covered by a thin layer of the mesothelium (mesothelium). The histological structure of the snake digestive system is not much different from the reptile digestive system. -

Kumka's Response to Stecco's Fascial Nomenclature Editorial
Journal of Bodywork & Movement Therapies (2014) 18, 591e598 Available online at www.sciencedirect.com ScienceDirect journal homepage: www.elsevier.com/jbmt FASCIA SCIENCE AND CLINICAL APPLICATIONS: RESPONSE Kumka’s response to Stecco’s fascial nomenclature editorial Myroslava Kumka, MD, PhD* Canadian Memorial Chiropractic College, Department of Anatomy, 6100 Leslie Street, Toronto, ON M2H 3J1, Canada Received 12 May 2014; received in revised form 13 May 2014; accepted 26 June 2014 Why are there so many discussions? response to the direction of various strains and stimuli. (De Zordo et al., 2009) Embedded with a range of mechanore- The clinical importance of fasciae (involvement in patho- ceptors and free nerve endings, it appears fascia has a role in logical conditions, manipulation, treatment) makes the proprioception, muscle tonicity, and pain generation. fascial system a subject of investigation using techniques (Schleip et al., 2005) Pathology and injury of fascia could ranging from direct imaging and dissections to in vitro potentially lead to modification of the entire efficiency of cellular modeling and mathematical algorithms (Chaudhry the locomotor system (van der Wal and Pubmed Exact, 2009). et al., 2008; Langevin et al., 2007). Despite being a topic of growing interest worldwide, This tissue is important for all manual therapists as a controversies still exist regarding the official definition, pain generator and potentially treatable entity through soft terminology, classification and clinical significance of fascia tissue and joint manipulative techniques. (Day et al., 2009) (Langevin et al., 2009; Mirkin, 2008). It is also reportedly treated with therapeutic modalities Lack of consistent terminology has a negative effect on such as therapeutic ultrasound, microcurrent, low level international communication within and outside many laser, acupuncture, and extracorporeal shockwave therapy. -
Connective Tissue – Material Found Between Cells – Supports and Binds Structures Together – Stores Energy As Fat – Provides Immunity to Disease
Chapter 4 The Tissue Level of Organization • Group of similar cells – common function • Histology – study of tissues • Pathologist – looks for tissue changes that indicate disease 4-1 4 Basic Tissues (1) • Epithelial Tissue – covers surfaces because cells are in contact – lines hollow organs, cavities and ducts – forms glands when cells sink under the surface • Connective Tissue – material found between cells – supports and binds structures together – stores energy as fat – provides immunity to disease 4-2 4 Basic Tissues (2) • Muscle Tissue – cells shorten in length producing movement • Nerve Tissue – cells that conduct electrical signals – detects changes inside and outside the body – responds with nerve impulses 4-3 Epithelial Tissue -- General Features • Closely packed cells forming continuous sheets • Cells sit on basement membrane • Apical (upper) free surface • Avascular---without blood vessels – nutrients diffuse in from underlying connective tissue • Rapid cell division • Covering / lining versus glandular types 4-4 Basement Membrane • holds cells to connective tissue 4-5 Types of Epithelium • Covering and lining epithelium – epidermis of skin – lining of blood vessels and ducts – lining respiratory, reproductive, urinary & GI tract • Glandular epithelium – secreting portion of glands – thyroid, adrenal, and sweat glands 4-6 Classification of Epithelium • Classified by arrangement of cells into layers – simple = one cell layer thick – stratified = many cell layers thick – pseudostratified = single layer of cells where all cells