Digestive Disease & Surgery Institute
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Practice Parameters for the Treatment of Patients with Dominantly Inherited Colorectal Cancer
Practice Parameters For The Treatment Of Patients With Dominantly Inherited Colorectal Cancer Diseases of the Colon & Rectum 2003;46(8):1001-1012 Prepared by: The Standards Task Force The American Society of Colon and Rectal Surgeons James Church, MD; Clifford Simmang, MD; On Behalf of the Collaborative Group of the Americas on Inherited Colorectal Cancer and the Standards Committee of the American Society of Colon and Rectal Surgeons. The American Society of Colon and Rectal Surgeons is dedicated to assuring high quality patient care by advancing the science, prevention, and management of disorders and diseases of the colon, rectum, and anus. The standards committee is composed of Society members who are chosen because they have demonstrated expertise in the specialty of colon and rectal surgery. This Committee was created in order to lead international efforts in defining quality care for conditions related to the colon, rectum, and anus. This is accompanied by developing Clinical Practice Guidelines based on the best available evidence. These guidelines are inclusive, and not prescriptive. Their purpose is to provide information on which decisions can be made, rather than dictate a specific form of treatment. These guidelines are intended for the use of all practitioners, health care workers, and patients who desire information about the management of the conditions addressed by the topics covered in these guidelines. Practice Parameters for the Treatment of Patients With Dominantly Inherited Colorectal Cancer Inherited colorectal cancer includes two main syndromes in which predisposition to the disease is based on a germline mutation that may be transmitted from parent to child. -
High Resolution Anoscopy Overview
High Resolution Anoscopy Overview Naomi Jay, RN, NP, PhD University of California San Francisco Email: [email protected] Disclosures No Disclosures Definition of HRA Examination of the anus, anal canal and perianus using a colposcope with 5% acetic acid and Lugol’s solution. Basic Principles • Office-based procedure • Adapted from gynecologic colposcopy. • Validated for anal canal. • Similar terminology and descriptors. may be unfamiliar to non-gyn providers. • Comparable to vaginal and vulvar colposcopy. • Clinicians familiar with cervical colposcopy may be surprised by the difficult transition. Anal SCJ & AnTZ • Original vs. current SCJ less relevant. • TZ features less common, therefore more difficult to appreciate. • SCJ more subtle, difficult to see in entirety requires more manipulation & acetic acid. • Larger area of metaplastic changes overlying columnar epithelium compared to endocervix. • Most lesions found in the AnTZ. Atypical Metaplasia • Atypical metaplasia may indicate the presence of HSIL. • Radiate over distal rectum from SCJ. • Thin, may wipe off. • Features to look for indicating potential lesions: • Atypical clustered glands (ACG) • Lacy metaplastic borders (LM) • Epithelial Honeycombing (EH) Lugol’s. Staining • More utility in anus compared to cervix. • Adjunctive to help define borders, distinguish between possible LSIL/HSIL. • Most HSIL will be Lugol’s negative • LSIL may be Lugol’s partial or negative • Applied focally with small cotton swabs to better define an acetowhite lesion. •NOT a short cut to determine presence or absence of lesions, acetic acid is used first and is applied frequently. Anal vs. Cervical Characteristics • Punctation & Mosaic rarely “fine” mostly “coarse”. • Mosaic pattern mostly associated with HSIL. • Atypical vessels may be HSIL or cancer • Epithelial honeycombing & lacy metaplasia unique anal descriptors. -

Lower Gastrointestinal Tract
Lower Gastrointestinal Tract Hemorrhoids—Office Management and Review for Gastroenterologists Mitchel Guttenplan, MD, FACS 1 and Robert A Ganz, MD, FASGE 2 1. Medical Director, CRH Medical Corp; 2. Minnesota Gastroenterology, Chief of Gastroenterology, Abbott-Northwestern Hospital, Associate Professor of Medicine, University of Minnesota Abstract symptomatic hemorrhoids and anal fissures are very common problems. This article provides a review of the anatomy and physiology of the anorectum along with a discussion of the diagnosis and treatment of hemorrhoids and the commonly associated matters of anal sphincter spasm and fissures. The various office treatment modalities for hemorrhoids are discussed, as are the specifics of rubber band ligation (rBL), and a strategy for the office treatment of these problems by the gastroenterologist is given. The crh o’regan system™ is a technology available to the gastroenterologist that provides a safe, effective, and efficient option for the non-surgical treatment of hemorrhoids in the office setting. Keywords hemorrhoids, anal fissure, rubber band ligation, crh o’regan system™ Disclosure: Mitchel guttenplan is Medical Director of crh Medical Products corporation, the manufacturer of the crh o’regan system™. robert A ganz is a consultant to and holds equity in crh Medical Products corporation. Received: 2 november 2011 Accepted: 30 november 2011 Citation: Touchgastroentorology.com ; December, 2011. Correspondence: Mitchel guttenplan, MD, fAcs, 3000 old Alabama rd, suite 119 #183, Alpharetta, gA 30022-8555, us. e: [email protected] Diseases of the anorectum, including hemorrhoids and anal fissures, are experience also makes it clear that hemorrhoid sufferers frequently very common. The care of these entities is typically left to general and have additional anorectal issues that may both confuse the diagnosis colorectal surgeons. -

Second European Evidence-Based Consensus on the Diagnosis and Management of Ulcerative Colitis: Special Situations
CROHNS-00649; No of Pages 33 Journal of Crohn's and Colitis (2012) xx, xxx–xxx Available online at www.sciencedirect.com SPECIAL ARTICLE Second European evidence-based consensus on the diagnosis and management of ulcerative colitis: Special situations Gert Van Assche⁎,1,2, Axel Dignass⁎⁎,2, Bernd Bokemeyer1, Silvio Danese1, Paolo Gionchetti1, Gabriele Moser1, Laurent Beaugerie1, Fernando Gomollón1, Winfried Häuser1, Klaus Herrlinger1, Bas Oldenburg1, Julian Panes1, Francisco Portela1, Gerhard Rogler1, Jürgen Stein1, Herbert Tilg1, Simon Travis1, James O. Lindsay1 Received 30 August 2012; accepted 3 September 2012 KEYWORDS Ulcerative colitis; Anaemia; Pouchitis; Colorectal cancer surveillance; Psychosomatic; Extraintestinal manifestations Contents 8. Pouchitis ............................................................ 0 8.1. General ......................................................... 0 8.1.1. Symptoms ................................................... 0 ⁎ Correspondence to: G. Van Assche, Division of Gastroenterology, Department of Medicine, Mt. Sinai Hospital and University Health Network, University of Toronto and University of Leuven, 600 University Avenue, Toronto, ON, Canada M5G 1X5. ⁎⁎ Correspondence to: A. Dignass, Department of Medicine 1, Agaplesion Markus Hospital, Wilhelm-Epstein-Str. 4, D-60431 Frankfurt/Main, Germany. E-mail addresses: [email protected] (G. Van Assche), [email protected] (A. Dignass). 1 On behalf of ECCO. 2 G.V.A. and A.D. acted as convenors of the consensus and contributed equally to this paper. 1873-9946/$ - see front matter © 2012 European Crohn's and Colitis Organisation. Published by Elsevier B.V. All rights reserved. http://dx.doi.org/10.1016/j.crohns.2012.09.005 Please cite this article as: Van Assche G, et al, Second European evidence-based consensus on the diagnosis and management of ulcerative colitis: Special situations, Journal of Crohn's and Colitis (2012), http://dx.doi.org/10.1016/j.crohns.2012.09.005 2 G. -

Management of Low Rectal Cancer Complicating Ulcerative Colitis: Proposal of a Treatment Algorithm
cancers Viewpoint Management of Low Rectal Cancer Complicating Ulcerative Colitis: Proposal of a Treatment Algorithm Bruno Sensi 1,*, Giulia Bagaglini 1, Vittoria Bellato 1 , Daniele Cerbo 1 , Andrea Martina Guida 1 , Jim Khan 2 , Yves Panis 3, Luca Savino 4, Leandro Siragusa 1 and Giuseppe S. Sica 1 1 Minimally Invasive Surgery, Department of Surgery, Policlinico Tor Vergata, 00133 Rome, Italy; [email protected] (G.B.); [email protected] (V.B.); [email protected] (D.C.); [email protected] (A.M.G.); [email protected] (L.S.); [email protected] (G.S.S.) 2 Colorectal Surgery Department, Queen Alexandra Hospital, Portsmouth NHS Trust, Portsmouth PO6 3LY, UK; [email protected] 3 Service de Chirurgie Colorectale, Pôle des Maladies de L’appareil Digestif (PMAD), Université Denis-Diderot (Paris VII),Hôpital Beaujon, Assistance Publique-Hôpitaux de Paris (AP-HP), 100, Boulevard du Général-Leclerc, 92110 Clichy, France; [email protected] 4 Pathology, Department of Biomedicine and Prevention, Policlinico Tor Vergata, 00133 Rome, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-338-535-2902 Simple Summary: This article expresses the viewpoint of the authors’ management of low rectal cancer in ulcerative colitis (UC). This subject suffers from a paucity of literature and therefore management decision is very difficult to take. The aim of this paper is to provide a structured Citation: Sensi, B.; Bagaglini, G.; approach to a challenging situation. It is subdivided into two parts: a first part where the existing Bellato, V.; Cerbo, D.; Guida, A.M.; literature is reviewed critically, and a second part in which, on the basis of the literature review Khan, J.; Panis, Y.; Savino, L.; and their extensive clinical experience, a management algorithm is proposed by the authors to offer Siragusa, L.; Sica, G.S. -

Endoscopy Matrix
Endoscopy Matrix CPT Description of Endoscopy Diagnostic Therapeutic Code (Surgical) 31231 Nasal endoscopy, diagnostic, unilateral or bilateral (separate procedure) X 31233 Nasal/sinus endoscopy, diagnostic with maxillary sinusoscopy (via X inferior meatus or canine fossa puncture) 31235 Nasal/sinus endoscopy, diagnostic with sphenoid sinusoscopy (via X puncture of sphenoidal face or cannulation of ostium) 31237 Nasal/sinus endoscopy, surgical; with biopsy, polypectomy or X debridement (separate procedure) 31238 Nasal/sinus endoscopy, surgical; with control of hemorrhage X 31239 Nasal/sinus endoscopy, surgical; with dacryocystorhinostomy X 31240 Nasal/sinus endoscopy, surgical; with concha bullosa resection X 31241 Nasal/sinus endoscopy, surgical; with ligation of sphenopalatine artery X 31253 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including frontal sinus exploration, with removal of tissue from frontal sinus, when performed 31254 Nasal/sinus endoscopy, surgical; with ethmoidectomy, partial (anterior) X 31255 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior 31256 Nasal/sinus endoscopy, surgical; with maxillary antrostomy X 31257 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including sphenoidotomy 31259 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including sphenoidotomy, with removal of tissue from the sphenoid sinus 31267 Nasal/sinus endoscopy, surgical; with removal of -

Public Use Data File Documentation
Public Use Data File Documentation Part III - Medical Coding Manual and Short Index National Health Interview Survey, 1995 From the CENTERSFOR DISEASECONTROL AND PREVENTION/NationalCenter for Health Statistics U.S. DEPARTMENTOF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics CDCCENTERS FOR DlSEASE CONTROL AND PREVENTlON Public Use Data File Documentation Part Ill - Medical Coding Manual and Short Index National Health Interview Survey, 1995 U.S. DEPARTMENT OF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics Hyattsville, Maryland October 1997 TABLE OF CONTENTS Page SECTION I. INTRODUCTION AND ORIENTATION GUIDES A. Brief Description of the Health Interview Survey ............. .............. 1 B. Importance of the Medical Coding ...................... .............. 1 C. Codes Used (described briefly) ......................... .............. 2 D. Appendix III ...................................... .............. 2 E, The Short Index .................................... .............. 2 F. Abbreviations and References ......................... .............. 3 G. Training Preliminary to Coding ......................... .............. 4 SECTION II. CLASSES OF CHRONIC AND ACUTE CONDITIONS A. General Rules ................................................... 6 B. When to Assign “1” (Chronic) ........................................ 6 C. Selected Conditions Coded ” 1” Regardless of Onset ......................... 7 D. When to Assign -

The Natural History of Familial Adenomatous Polyposis Syndrome: a 24 Year Review of a Single Center Experience in Screening, Diagnosis, and Outcomes
Journal of Pediatric Surgery 49 (2014) 82–86 Contents lists available at ScienceDirect Journal of Pediatric Surgery journal homepage: www.elsevier.com/locate/jpedsurg The natural history of familial adenomatous polyposis syndrome: A 24 year review of a single center experience in screening, diagnosis, and outcomes Raelene D. Kennedy a,⁎, D. Dean Potter a, Christopher R. Moir a, Mounif El-Youssef b a Division of Pediatric Surgery, Department of Surgery, Mayo Clinic, Rochester, MN 55905 b Division of Gastroenterology and Hepatology, Department of Pediatrics, Mayo Clinic, Rochester, MN 55905 article info abstract Article history: Purpose: Understanding the natural history of Familial Adenomatous Polyposis (FAP) will guide screening and Received 17 September 2013 aid clinical management. Accepted 30 September 2013 Methods: Patients with FAP, age ≤20 years presenting between 1987 and 2011, were reviewed for presentation, diagnosis, extraintestinal manifestations, polyp burden, family history, histology, gene Key words: mutation, surgical intervention, and outcome. Familial adenomatous polyposis Results: One hundred sixty-three FAP patients were identified. Diagnosis was made by colonoscopy (69%) or Pediatric genetic screening (25%) at mean age of 12.5 years. Most children (58%) were asymptomatic and diagnosed via Screening screening due to family history. Rectal bleeding was the most common (37%) symptom prompting evaluation. Colon polyps appeared by mean age of 13.4 years with N50 polyps at the time of diagnosis in 60%. Cancer was found in 1 colonoscopy biopsy and 5 colectomy specimens. Family history of FAP was known in 85%. 53% had genetic testing, which confirmed APC mutation in 88%. Extraintestinal manifestations included congenital hypertrophy of the retinal pigment epithelium (11.3%), desmoids (10.6%), osteomas (6.7%), epidermal cysts (5.5%), extranumerary teeth (3.7%), papillary thyroid cancer (3.1%), and hepatoblastoma (2.5%). -
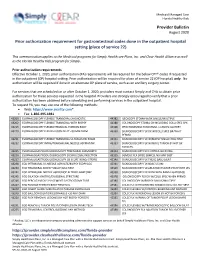
Provider Bulletin Prior Authorization Requirement for Gastrointestinal
Medicaid Managed Care Florida Healthy Kids Provider Bulletin August 2020 Prior authorization requirement for gastrointestinal codes done in the outpatient hospital setting (place of service 22) This communication applies to the Medicaid programs for Simply Healthcare Plans, Inc. and Clear Health Alliance as well as the Florida Healthy Kids program for Simply. Prior authorization requirements Effective October 1, 2020, prior authorization (PA) requirements will be required for the below CPT® codes if requested in the outpatient (OP) hospital setting. Prior authorization will be required for place of service 22 (OP hospital) only. No authorization will be required if done in an alternate OP place of service, such as an ancillary surgery center. For services that are scheduled on or after October 1, 2020, providers must contact Simply and CHA to obtain prior authorization for these services requested in the hospital. Providers are strongly encouraged to verify that a prior authorization has been obtained before scheduling and performing services in the outpatient hospital. To request PA, you may use one of the following methods: Web: https://www.availity.com* Fax: 1-866-495-1981 43200 ESOPHAGOSCOPY FLEXIBLE TRANSORAL DIAGNOSTIC 44382 ILEOSCOPY STOMA W/BX SINGLE/MULTIPLE 43202 ESOPHAGOSCOPY FLEXIBLE TRANSORAL WITH BIOPSY 44388 COLONOSCOPY STOMA DX INCLUDING COLLJ SPEC SPX 43215 ESOPHAGOSCOPY FLEXIBLE REMOVAL FOREIGN BODY 45308 PROCTOSGMDSC RIGID RMVL 1 LESION CAUTERY 43220 ESOPHAGOSCOPY FLEX BALLOON DILAT <30 MM DIAM 45330 SIGMOIDOSCOPY -

When a Case of Ulcerative Colitis Requires Mucosectomy and Hand-Sewn Ileo-Anal Pouch Anastomosis Mary Teresa M O’Donnell1,2*, Joshua IS Bleier3 and Gary Wind4
ISSN: 2378-3397 O’Donnell et al. Int J Surg Res Pract 2018, 5:079 DOI: 10.23937/2378-3397/1410079 Volume 5 | Issue 2 International Journal of Open Access Surgery Research and Practice CASE REPORT When a Case of Ulcerative Colitis Requires Mucosectomy and Hand-Sewn Ileo-Anal Pouch Anastomosis Mary Teresa M O’Donnell1,2*, Joshua IS Bleier3 and Gary Wind4 1Colon & Rectal Surgery Fellow, University of Pennsylvania, USA 2 Check for Assistant Professor of Surgery, Uniformed Services University of the Health Sciences, USA updates 3Associate Professor of Surgery, Department of Surgery, University of Pennsylvania, USA 4Professor of Surgery, Uniformed Services University of the Health Sciences, USA *Corresponding author: Mary Teresa M O’Donnell, Colon & Rectal Surgery Fellow, ACS AEI Educational Fellow, University of Pennsylvania, USA; Assistant Professor of Surgery, Uniformed Services University of the Health Sciences, USA, E-mail: [email protected] Summary who have undergone mucosectomy [4]. In addition, it is associated with increased risk of incontinence and Treatment of ulcerative colitis with total proctocol- operative difficulty. As a result, mucosectomy is rarely ectomy and ileal pouch anal anastomosis (IPAA) pro- performed. vides a near cure for the bowel component of ulcerative colitis, a restoration of bowel continuity, and the possi- Nevertheless, there are cases where mucosectomy and bility of normal defecation behaviors for patients. The hand-sewn ileal anal anastomosis may be required. If there majority of these procedures are carried out using end- are significant mucosal changes associated with ulcerative to-end circular stapling devices, which shorten surgery colitis that persist low in the rectum to the dentate line, times and have been shown to give better long-term the double-stapled anastomosis may be inadequate. -

APG Regulations
FINAL as of 8/22/08 Pursuant to the authority vested in the Commissioner of Health by Section 2807(2-a) of the Public Health Law, Part 86 of Title 10 of the Official Compilation of Codes, Rules and Regulations of the State of New York, is amended by adding a new Subpart 86-8, to be effective upon filing with the Secretary of State, to read as follows: SUBPART 86-8 OUTPATIENT SERVICES: AMBULATORY PATIENT GROUP (Statutory authority: Public Health Law § 2807(2-a)(e)) Sec. 86-8.1 Scope 86-8.2 Definitions 86-8.3 Record keeping, reports and audits 86-8.4 Capital reimbursement 86-8.5 Administrative rate appeals 86-8.6 Rates for new facilities during the transition period 86-8.7 APGs and relative weights 86-8.8 Base rates 86-8.9 Diagnostic coding and rate computation 86-8.10 Exclusions from payment 86-8.11 System updating 86-8.12 Payments for extended hours of operation § 86-8.1 Scope (a) This Subpart shall govern Medicaid rates of payments for ambulatory care services provided in the following categories of facilities for the following periods: (1) outpatient services provided by general hospitals on and after December 1, 2008; (2) emergency department services provided by general hospitals on and after January 1, 2009; (3) ambulatory surgery services provided by general hospitals on and after December 1, 2008; (4) ambulatory services provided by diagnostic and treatment centers on and after March 1, 2009; and (5) ambulatory surgery services provided by free-standing ambulatory surgery centers on and after March 1, 2009. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular